1. Background
Today, chronic diseases are recognized as the most important health problem, especially in developing countries (1). Among chronic diseases, cardiovascular disease is one of the most common diseases in the world (2). According to the latest report of the World Health Organization in 2022, seven out of the ten most common causes of death worldwide in 2019 were related to non-communicable diseases, of which ischemic heart disease ranked first (3). In 2008, about 17 million people worldwide died of cardiovascular disease, which accounted for 30% of all global deaths, and this number is projected to reach over 23 million by 2030 (4). Although coronary heart disease is among the most common fatal diseases, arrhythmias, especially ventricular tachyarrhythmia, can cause life-threatening complications if left untreated (5). One method of rapid diagnosis and treatment of dangerous ventricular arrhythmias (ventricular tachycardia that causes hemodynamic dysfunction or drug-resistant ventricular fibrillation) is the use of an implantable defibrillator (6). With the advancement of science, Cardioverter-defibrillator (ICD), has long been used as the treatment of choice for the secondary prevention of SCD.
Despite a decrease in the overall mortality rate after the insertion of ICD, ICD recipients typically face challenges in adapting to life-threatening arrhythmias and treatment, which include fear of recurrent arrhythmias and sudden death, ICD dysfunction, and lack of control over energy discharge. Results of a study conducted on patients with ICD showed that 97% of patients did not have accurate and complete information about the device care, and this posed significant medical, social, and financial problems for them (7). Studies show that one of the major complaints frequently reported by patients with heart disease is the lack of awareness of self-care behaviors (8, 9), as 90% of patients have questions about self-care, diet, and medication at the time of discharge and at home (10). Control of risk factors and lifestyle modification in these patients play an important role that increases the need for self-care in them (11). Therefore, in patients with heart problems, increasing awareness and performance should be the main goal of care and treatment (12).
The installation of this device affects the individual's performance, social and family relationships, physical activity, psychological status, and quality of life. Studies show that patients who experience life with an ICD face fear and anxiety, results, outcomes, dependence on the device, lifestyle changes, lack of control, non-acceptance, mental conflict, psychological concern, reduced security, financial problems, changes in social relations, changes in roles, sleep disorders, and post-traumatic stress disorder (13).
As mentioned, patients with ICD experience a great deal of physical and mental stress, and this necessitates the need to be empowered in self-care. Implementing an effective strategy to empower patients in health-oriented behaviors has always been the goal of nurses.
2. Objectives
The present study was conducted to determine the effect of a continuous care program on short-term consequences of anxiety, the number of shocks received, and the number of emergency outpatient visits to the medical center in patients with ICD.
3. Methods
The present study is a randomized clinical trial with two groups, control and intervention. The research environment consisted of the electrophysiology clinic, CCU, and medical and surgical wards of Tehran Cardiovascular Training Center, Iran. The study population included all patients with the experience of a cardiac arrest or life-threatening dysrhythmia who were first on the list to receive ICD.
Inclusion criteria were: Being 20 - 80 years old, receiving ICD for the first time, having the ability to read, write, and speak in Persian, and having telephone access. Exclusion criteria included: Having cognitive impairment and participating in another intervention program at the same time as this study. Allocation of patients in the intervention and control groups was done by block randomization method. The allocation sequence was generated using a web-based system available at: Randomization Link.
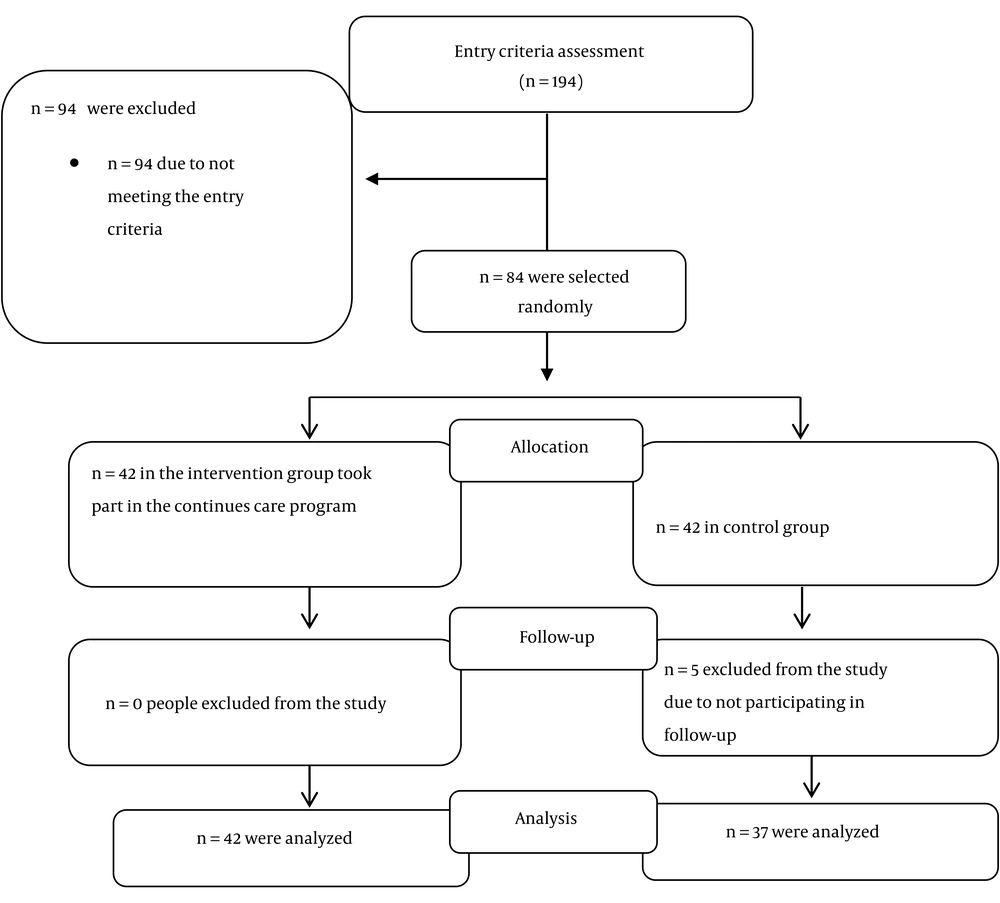
The sample size of this study was calculated to be 80 patients (n = 40 in each group) according to previous studies (14), taking into account Z1 = 96.1 and ZB = 0.85 and standard deviation S = 6.1 in both groups, and the mean of µ1 = 21.69 in the control group and µ2 = 22.48 in the intervention group. However, after considering the sample loss of 10%, 42 patients were considered for each group. From the 194 patients admitted to receive ICD for the first time and based on the inclusion and exclusion criteria, 94 were excluded and 100 patients remained, who were randomly allocated into two groups by blocked randomization, with block sizes of 2 containing A and B (Figure 1).
3.1. Data Collection Tools
In this study, two tools were used to collect information:
(1) Demographic and disease information questionnaire
(2) Spielberger State-Trait Anxiety Inventory (STAI)
The demographic and disease information questionnaire included 14 questions about personal characteristics (such as age, BMI, gender, nationality, marital status, education level, employment status, income level, place of residence, phone number, type of health insurance) and disease information (such as Carlson Comorbidity Index, Short Blessed Score, cause of ICD implantation, cardiac EF, and history of myocardial infarction). This questionnaire was made by the researcher.
The Spielberger State-Trait Anxiety Inventory (STAI) was standardized in 1970 by Spielberger et al. to measure state and trait anxiety and is one of the most appropriate tools for measuring anxiety. This questionnaire consists of 20 questions and its scoring system ranges from 20 to 80, with a higher score indicating a higher level of anxiety. The scores of 20 - 31 refer to mild anxiety, 32 - 42 refer to moderate to low anxiety, 43 - 53 characterize moderate to high anxiety, 54 - 64 highlight almost severe anxiety, 65 - 75 refer to severe anxiety, and above 75 refer to extremely severe anxiety. The validity and reliability of STAI in Iran were reported by Kalkhoran and Karimollahi with a Cronbach's alpha coefficient of 0.93 (15).
3.2. Intervention
In addition to the usual care (oral explanation of clinical nurses, physicians, and written brochures) provided in the heart center, patients in the intervention group received a continuous care program. For this purpose, two face-to-face training sessions for 1.5 hours were given to patients in the intervention group by the main researcher (Master of Science student in Nursing) individually at the time of discharge (familiarization stage) and then, at the time of follow-up visit to the electrophysiology clinic, which was usually a month later. In the first session and before discharge, the demographic and disease information questionnaire was completed by samples and their self-efficacy and level of anxiety were measured. The researcher then established an initial relationship with the patients in order to gain their trust and then explained the study objectives and methods as well as the ways of communication.
In the second session, one month after discharge, self-care methods and necessary changes in lifestyle, device function, expected feelings at the time of energy discharge, activity required by the patient after each shock, how to record cases of shock, and warnings that need to be followed were taught to patients and explanations were given about communication with family members and others. The researcher described anxiety-reducing methods, such as listening to music, saying dhikr, and methods of distraction and relaxation, and based on the patient's desire, explained the selected method to the patient and practiced it if necessary.
At the end of the second session, patients were given an educational booklet that contained two components: (1) explanation in simple language about the heart, the types of cardiac shocks, and the high-risk to low-risk conditions for the device; and (2) a description of patients' statements about their experiences in the first year of recovery from ICD insertion, which the patient is expected to encounter during the recovery period. Finally, the contact number was taken from the patient to follow-up the care program via weekly phone calls at the patient's chosen time, between 8 am to 8 pm for about 10 to 20 minutes according to the patient's needs. Telephone calls were made once a week for 8 weeks with the content of verbal encouragement, answering patient questions, helping to make decisions, solving everyday problems, and reinforcing instruction (control phase). At the end of the eighth week after discharge, the questionnaire of self-efficacy, anxiety, and short-term consequences was completed by the patient in both groups (evaluation stage). In the control group, after receiving routine care in this center and before discharge, they completed the self-efficacy and outcome expectation questionnaire as well as the anxiety questionnaire. Twelve weeks after discharge, patients' self-efficacy, anxiety, and short-term outcomes were re-assessed in both groups.
3.3. Data Analysis Method
In the present study, SPSS software version 16 was used to analyze the data. Descriptive statistics (such as mean and frequency percentage) and inferential statistics (independent Student, Mann-Whitney, paired t-test, and Wilcoxon) were used to compare the data.
3.4. Ethical Considerations
All ethical considerations, including written consent, maintaining anonymity, presenting results to hospital officials and participants upon request, and assuring patients in the control group that they will receive the content of the self-care guide for patients with cardiac shock (ICD) after completing the research, were preserved in this study. Freedom was given to the participants to withdraw from the study at any time without any consequences. This plan was approved by the ethics committee of the School of Nursing and Midwifery with the code pp/95/2. This study was also registered in the Clinical Trial Registration Center with the code: IRCT20100725004443N24.
4. Results
Demographic findings show that the mean and standard deviation of the participants’ age in the control group were 54.5 ± 11.0 years and in the intervention group were 51.1 ± 12.5 years. The mean height of patients in the control group was 166.8 ± 9.6 cm and in the intervention group was 170 ± 10.1 cm. The mean weight of patients in the control group was 76.5 ± 13.6 kg and in the intervention group was 76.2 ± 11.9 kg. The BMI of patients in the control group was 27.5 ± 4.1 and in the intervention group was 26.5 ± 4.2. Independent t-test did not show a significant difference between the two groups in terms of this variable (P = 0.258). Also, 83.8% of patients in the control group and 95.2% in the intervention group were married. Fisher's exact statistical test did not show a significant difference in marital status between the two groups (P = 0.138). In the control group, 73.0% of the subjects and in the intervention group, 78.6% of the subjects were male, and the chi-square test did not show a significant difference between the two groups in this regard (P = 0.561). Also, 59.5% of patients in the control group and 66.7% in the intervention group had a previous history of MI, and the chi-square test did not show a significant difference between the two groups in this regard (P = 0.507) (Table 1).
| Variables | Control Group | Intervention Group | Result of Independent t-Test |
|---|---|---|---|
| Age | 54.5 ± 11.0 | 51.1 ± 12.5 | t = 1.3, df = 77, P = 0.210 |
| Height | 166.8 ± 9.6 | 170.0 ± 10.1 | t = 1.4, df = 77, P = 0.156 |
| Weight | 76.5 ± 13.6 | 76.2 ± 11.9 | t = 0.1, df = 77, P = 0.910 |
| BMI | 27.5 ± 4.1 | 26.5 ± 4.2 | t = 1.1, df = 77, P = 0.258 |
| Marital status | |||
| Single | 6 (16.2) | 2 (4.8) | |
| Married | 31 (83.8) | 40 (95.2) | |
| Total | 37 (100) | 42 (100) | F = 0.23, P = 0.138 |
| Gender | 10 (27) | 9 (21.4) | K2 = 0.3, P = 0.56 |
| Women | 27 (73) | 33 (78.6) | |
| Men | 37 (100) | 42 (100) | |
| Total |
Mean and Standard Deviation of Age, Height, Weight and BMI in Patients with ICD in the Two Groups of Control and Intervention a
The short-term consequences examined in this study included the level of anxiety, the mean number of shocks received, and the number of emergency outpatient visits to the clinic and their reasons. In the control group, the level of anxiety decreased by 1.3 ± 6.4, but according to the paired t-test, this difference was not significant (P = 0.222). In the intervention group, the level of anxiety decreased by 10.8 ± 11.2, which, according to the paired t-test, was significant (P < 0.001). The independent t-test showed a significant difference in the mean scores of anxiety between the two groups (P < 0.001). In other words, only in the intervention group was the reduction of anxiety level after the intervention significant compared to before the intervention (Table 2).
| Anxiety Level | Control Group | Intervention Group | Results of Inter-Group Test |
|---|---|---|---|
| Before intervention | 39.2 ± 9.2 | 45.7 ± 10.5 | t = -2.9, df = 77, independent t-test P = 0.004 |
| After intervention | 37.9 ± 9.8 | 34.9 ± 8.7 | t = 1.4, df = 77, independent t-test P = 0.156 |
| Pre/post-difference | -1.3 ± 6.4 | -10.8 ± 11.2 | t = 4.7, df = 66, independent t-test P < 0.001 |
| Results of intra-group test | t = 1.2, df = 36, Paired t-test P = 0.222 | t = 6.3, df = 41, Paired t-test P < 0.001 |
Mean and Standard Deviation of Anxiety Level Before and After Intervention in the Two Groups of Control and Intervention a
Table 2 demonstrates the comparison of the frequency of patients with ICD in terms of the severity of anxiety before and after the intervention in the control and intervention groups. Before the intervention, in the control group, 21.6% of people had mild anxiety and 40.5% had moderate to low anxiety. After the intervention, in the control group, 21.6% of the subjects had mild anxiety and 45.9% of the subjects had moderate to low anxiety. The Wilcoxon test did not show this difference to be significant (P = 0.499). Before the intervention, in the intervention group, 4.8% of people had mild anxiety and 35.7% had moderate to low anxiety. After the intervention, in the intervention group, 35.7% of people had mild anxiety and 45.2% had moderate to low anxiety. The Wilcoxon test showed this difference to be significant (P < 0.001) (Table 3).
| Variables And Severity of Anxiety | Control Group | Intervention Group | Results of Test |
|---|---|---|---|
| Before intervention | |||
| Mild | 8 (21.6) | 2 (4.8) | |
| Moderate to low | 15 (40.5) | 15 (35.70) | |
| Over average | 10 (27.00) | 15 (35.70) | |
| Fairly Sever | 4 (10.8) | 7 (16.7) | |
| Severe | 0 (0.0) | 3 (7.10) | |
| Very Severe | 0 (0.0) | 0 (0.0) | |
| Total | 37 (100) | 42 (100) | X2 = 8.13, P = 0.08, chi-square test |
| After intervention | |||
| Mild | 8 (21.6) | 15 (35.70) | |
| Moderate to low | 17 (45.9) | 19 (45.20) | |
| Over average | 9 (24.30) | 7 (16.70) | |
| Fairly Sever | 3 (8.1) | 1 (2.4) | |
| Severe | 0 (0.0) | 0 (0.00) | |
| Very Severe | 0 (0.0) | 0 (0.0) | |
| Total | 37 (100) | 42 (100) | X2 = 3.18, P = 0.36, chi-square test |
| Test result inter-group test | McNemar bowker = 0.55, P = 0.43 |
Comparison of the Frequency of Patients with Implantable Heart Shock in Terms of the Severity of Anxiety Before and After the Intervention in the Control and Intervention Groups a
The mean and standard deviation of the number of emergency outpatient visits to the clinic in the control group was 0.2 ± 0.5, with a median of 0.3 and interquartile ranges (25th and 75th percentile) were Q1 = 0.1 and Q3 = 0.4. In the intervention group, the mean and standard deviation was 0.3 ± 0.6, with a median of 0.2 and interquartile ranges (25th and 75th percentile) were Q1 = 0.1 and Q3 = 0.4. The independent t-test showed that the difference between the two groups was not significant in this regard (P = 0.42).
The mean and standard deviation of the number of shocks in the control group was 1.2 ± 4.4, and in the intervention group was 5.1 ± 12.3. According to the independent t-test, this difference was significant (P = 0.02). In other words, the number of ICD shocks in patients in the intervention group was significantly higher than in the control group.
In the control group, 7 patients had an emergency visit to the clinic due to general questions about the ICD device, rather than adjustment of the device, while in the intervention group, 3 patients had such visits. The K2 test showed that although the number of clinic visits after discharge decreased in the intervention group compared to the control group, this decrease was not significant (P = 0.11). The same was true for adjustment of the ICD device (P = 0.8) (Table 4).
| Reason For Visiting the Clinic | Control Group | Intervention Group | Results of Test | |
|---|---|---|---|---|
| K2 | P | |||
| General question about: | ||||
| The device | 3 (7.15) | -2.46 | 0.11 | |
| Have | 7 (18.9) | |||
| Does not have | 30 (8.1) | 39 (92.85) | ||
| Adjustment of the ICD device | 0.36 | 0.8 | ||
| Have | 1 (2.7) | 8 (19 | ||
| Does not have | 36 (97.3) | 34 (81) | ||
Comparison Frequency of Patients with ICD in Terms of the Reason of Visiting in the Clinic After Discharge in Control and Intervention Groups a
5. Discussion
The aim of this study was to investigate the effect of a continuous care program on the short-term consequences of anxiety, the number of shocks received, and the number of emergency outpatient visits to the clinic and their reasons. Findings of this study showed that the continuous care program significantly reduced patients' anxiety levels and its severity. Similar to the results of this study, Agarwal et al. on behalf of Dougherty et al. (as cited in Agarwal) in a study in the United States showed that providing telephone intervention by cardiovascular nurses during the first 8 weeks of ICD insertion reduced patients’ symptoms of ICD-related anxiety and also increased their knowledge of SCD after three months (16). Various studies, including the study of Moradi et al. (13), have shown that patients with ICD experience certain adversities in life, including physical distress (limited mobility, pain from electric shock discharge, loss of self-control), psychological distress (living with fear, facing death while receiving a shock, waiting to receive a shock), and device-related distress (device failure, device financing, device-related limitations). Anxiety, as a psychological disorder, is usually associated with ICD patients (13, 17, 18), and according to the results of the present study, the continuous care program can significantly reduce the level of anxiety in these patients.
Another variable examined in this study was the emergency outpatient visit to the clinic, which was significantly reduced after the intervention. A study conducted in the Philippines also found that a three-day post-discharge structural program presented by cardiovascular nurses had a positive effect on satisfaction, self-efficacy, and emergency outpatient visits of heart patients (19, 20).
The results of the present study revealed that a continuous care program can significantly reduce the outpatient visits and anxiety of patients with ICD, although the number of shocks in the intervention group was higher, showing that the intervention does not affect the number of shocks variable. This can be due to the pathology of heart electrical activity, which is unique in each patient and is not in control of the researcher. Based on these results, this program can be used as an effective care model in the nursing care of patients with ICD to reduce the short-term consequences of ICD insertion, or in other words, the burden of disease. The continuous care program, as a native model, has the potential to be used continuously in Iran’s health care system to care for patients receiving ICD. One of the limitations of this study was its sample loss due to patient death and unwillingness to stay until completion of research, which was taken into account when considering the sample size. Among the other limitations of the present study is the influence of adverse environmental conditions and factors on the mental and emotional state (like bad news) and anxiety level of the patients. There was also a time limit for the research.
5.1. Conclusions
Due to the significant effect of planned intervention for patients with an ICD device, the implementation of continuous care programs after discharge from the hospital is necessary for these patients. As the number of heart patients is increasing day by day, the need for new and effective programs to control complications in these patients is felt more than ever, and the continuous care program can be introduced as an effective care model in this regard.