1. Background
Cardiovascular disease (CVD) is a leading cause of mortality in many countries worldwide, including Iran (1). Over the past two decades, there has been a notable rise in CVD mortality in low-income nations, accounting for more than three-quarters of all CVD-related deaths, while there has been a decline in high-income countries (2). Projections indicate that CVDs will continue to be the primary cause of death globally by 2030, with an estimated 23.6 million individuals expected to succumb to this condition (3).
The location of MI serves as a prognostic indicator for mortality post-MI, emphasizing the importance of identifying high-risk patient subcategories. The most common MI location is acute transmural MI of the anterior wall, and acute MI of the anterior wall has a worse prognosis than infarctions in other parts of the heart (1). It has been reported that the 1-year survival rate in patients with anterior wall MI is lower than in those with inferior wall MI (1). Previous studies have shown that patients with anterior-wall MI have a poorer prognostic outcome than those with inferior-wall MI (4, 5). Conversely, other studies have suggested that patients with inferior wall MI complicated by right ventricular infarction, complete heart block, or occlusion of the dominant left circumflex artery (LCX) have an unfavorable clinical outcome.
2. Objectives
Given these conflicting results, the aim of the current study is to compare one-year survival in patients with anterior versus inferior ST-elevation myocardial infarction.
3. Methods
3.1. Patient Population
In this retrospective cohort study based on a registry, we enrolled all individuals admitted to Imam Ali Hospital between July 2018 and December 2019 with acute ST-segment elevation MI (STEMI) who subsequently underwent PPCI within 12 hours of presentation. A total of 643 patients diagnosed with STEMI who met our inclusion criteria were enrolled. All eligible adult patients (≥ 18 years) with STEMI, diagnosed according to current guidelines (6), were included in the registry. Both inferior and anterior STEMI cases were considered in our analysis. Individuals who had been hospitalized for more than 24 hours before being transferred to Imam Ali Hospital were excluded from the study.
3.2. Baseline Assessment
Trained nurses collected demographic, lifestyle, and clinical data through personal interviews with patients and/or their caregivers, with data quality assurance conducted by a general practitioner. Past cardiovascular incidents, coronary interventions, diabetes, and hypertension were documented based on physician-validated self-reports. Information regarding vital signs, early reperfusion treatments, electrocardiograms, medical therapy, and lab examinations was extracted from hospital medical files. Early reperfusion treatments included PPCI, thrombolytic therapy, or no reperfusion. Body Mass Index (BMI) was calculated using established methods, and lipid profile levels were assessed upon admission. Glomerular filtration rate (GFR) was estimated using the CKD-EPI formula. Echocardiography findings were used to record the left ventricular ejection fraction (LVEF). Trained physicians ensured the quality of all documented data.
3.3. Study Outcome and Follow-up
The primary outcome was one-year all-cause mortality following STEMI, either during the initial hospitalization or post-discharge. In-hospital mortality rates were documented through hospital records. Upon admission, contact details of patients, family members, or caregivers were recorded. Patients were monitored via telephone calls one year after the incident. In cases of reported deaths, all clinical and hospital records, along with the cause of death, were gathered and assessed by the research team. Follow-up duration ranged from the date of STEMI diagnosis to the date of death, loss to follow-up, or up to 365 days post-STEMI, whichever occurred first.
3.4. Ethical Approval and Consent for Study
All participants provided written informed consent before participating in the study. The study protocol was approved by the Research Ethics Committee at the Office of Research of Kermanshah University of Medical Sciences, with the ethics registration code IR.KUMS.REC.1400.252.
3.5. Statistical Analysis
For analytical purposes, participants were divided into two distinct cohorts: Anterior and inferior ST-elevation myocardial infarction. Continuous variables were presented as mean ± standard deviation (SD), while categorical variables were shown as absolute values and percentages. Statistical methods such as the chi-squared test, t-test, and Mann-Whitney U test were used to compare the baseline characteristics between these two groups.
A Cox proportional hazard regression analysis was conducted to determine the hazard ratio and 95% confidence interval (HR, 95% CI) regarding the relationship between anterior and inferior STEMI and the occurrence of all-cause mortality. Four hazard ratios (95% CIs) were reported, including crude values, model 1 adjustments, and model 2 adjustments. In model 1, the correlation between anterior and inferior STEMI and mortality was assessed after controlling for age and gender. Model 2 further examined this association while adjusting for model 1 variables, as well as additional factors such as anterior wall myocardial infarction, inferior wall myocardial infarction, BMI, diabetes, GFR, low-density lipoprotein (LDL)-cholesterol, high-density lipoprotein (HDL)-cholesterol, hypertension, hyperlipidemia, heart rate > 100 bpm, systolic blood pressure < 100 mm Hg, LVEF, smoking, previous coronary artery bypass graft (CABG), previous percutaneous coronary intervention (PCI), previous MI, and reperfusion therapy (PPCI, thrombolytic, no reperfusion).
In this study, the number of missing values for the covariates was relatively small (GFR: 4, BMI: 21, LDL: 53, HDL: 54, EF: 20, previous CABG: 1). All analyses were performed on complete case data. Seven (1.09%) patients were lost to follow-up. All statistical analyses were performed using R software version 4.2.1. A P-value < 0.05 was considered statistically significant. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (7).
4. Results
4.1. Baseline Characteristics and Clinical Presentation
A total of 197 (30.64%) patients were diagnosed with anterior STEMI, while 446 (69.36%) had inferior STEMI. Table 1 displays the baseline characteristics of the individuals in these two cohorts. No statistically significant differences were observed between the groups in terms of risk factors and various comorbidities, except for a higher level of HDL and lower levels of EF and CABG in the anterior STEMI group.
| Variables | Total | Anterior STEMI; (197, 30.64) | Inferior STEMI; (446, 69.36) | P-Value |
|---|---|---|---|---|
| Age (y) | 61.24 ± 12.24 | 62.30 ± 12.26 | 60.77 ± 12.21 | 0.143 |
| GFR (mL/min/1.73 m2) | 67.95 ± 18.89 | 67.95 ± 18.89 | 69.52 ± 19.11 | 0.376 |
| BMI | 26.25 ± 4.25 | 26.30 ± 4.10 | 26.23 ± 4.31 | 0.976 |
| LDL | 97.45 ± 27.58 | 97.44 ± 25.71 | 97.46 ± 28.38 | 0.988 |
| HDL | 41.04 ± 8.44 | 42.66 ± 9.25 | 40.35 ± 7.98 | 0.007 |
| Ejection fraction | 40.16 ± 8.48 | 34.55 ± 7.45 | 43.34 ± 7.45 | < 0.001 |
| Gender | 0.393 | |||
| Male | 509 (79.16) | 160 (81.22) | 349 (78.25) | |
| Female | 134 (20.84) | 37 (18.78) | 97 (21.75) | |
| Atrial fibrillation | 0.824 | |||
| No | 609 (94.71) | 186 (94.42) | 423 (94.84) | |
| Yes | 34 (5.29) | 11 (5.58) | 23 (5.16) | |
| Diabetes mellitus | 0.758 | |||
| No | 501 (77.92) | 152 (77.16) | 349 (78.25) | |
| Yes | 142 (22.08) | 45 (22.84) | 97 (21.45) | |
| Hypertension | 0.588 | |||
| No | 352 (54.74) | 111 (56.35) | 241 (54.04) | |
| Yes | 291 (45.26) | 86 (43.65) | 205 (45.96) | |
| Hyperlipidemia | 0.166 | |||
| No | 466 (72.47) | 150 (76.4) | 36 (70.85) | |
| Yes | 77 (27.53) | 47 (23.86) | 130 (29.15) | |
| Smoking | 0.063 | |||
| No | 393 (61.12) | 131 (66.50) | 262 (58.74) | |
| Yes | 250 (38.88) | 66 (33.50) | 184 (41.26) | |
| Previous PCI | 0.943 | |||
| No | 598 (93) | 183 (92.89) | 415 (93.05) | |
| Yes | 45 (7) | 14 (7.11) | 3 (6.95) | |
| Previous CABG | 0.004 | |||
| No | 63 (95.48) | 195 (98.98) | 418 (93.93) | |
| Yes | 29 (4.52) | 2 (1.02) | 27 (6.07) | |
| Old myocardial infarction | 0.407 | |||
| No | 571 (88.80) | 178 (90.36) | 393 (88.12) | |
| Yes | 72 (1.20) | 19 (9.64) | 53 (11.88) | |
| Reperfusion therapy | 0.052 | |||
| PPCI | 362 (56.30) | 122 (61.93) | 240 (53.81) | |
| Thrombolytic | 196 (30.48) | 47 (23.86) | 149 (33.41) | |
| No reperfusion | 85 (13.22) | 28 (14.21) | 57 (12.78) | |
| HR > 100 bpm | < 0.001 | |||
| No | 145 (73.60) | 393 (88.51) | 538 (83.93) | |
| Yes | 52 (26.40) | 51 (11.49) | 103 (16.07) | |
| SBP < 100 mmHg | 0.021 | |||
| No | 186 (94.90) | 397 (89.21) | 583 (90.95) | |
| Yes | 10 (5.10) | 48 (10.79) | 58 (9.05) | |
| Number of coronary arteries involvement | 0.04 | |||
| Normal | 10 (1.82) | 1 (0.57) | 9 (2.40) | |
| One vessel | 161 (29.33) | 64 (36.78) | 97 (25.87) | |
| Two vessels | 159 (28.87) | 47 (27.01) | 112 (29.87) | |
| Three vessels | 219 (39.89) | 62 (35.36) | 157 (41.87) | |
| In hospital mortality | 25 (3.89) | 8 (4.06) | 17 (3.81) | 0.880 |
| One-year mortality | 52 (8.18) | 15 (7.69) | 37 (8.39) | 0.767 |
Abbreviations: BMI, Body Mass Index; LDL-cholesterol, low-density lipoprotein cholesterol; HDL-cholesterol, high-density lipoprotein cholesterol; GFR, glomerular filtration rate; PPCI, primary percutaneous coronary intervention; HR, Heart rate; SBP, systolic blood pressure.
a Values are expressed as No. (%) or mean ± SD.
4.2. Short-term and Long-term Outcomes
During the 598-patient follow-up period, totaling 4,109 person-days, 7 patients (1.09%) were lost to follow-up in the inferior and anterior STEMI groups. No statistically significant difference was observed between the anterior and inferior groups, with mortality rates of 37 (8.39%) vs. 15 (7.69%), respectively, (P = 0.767).
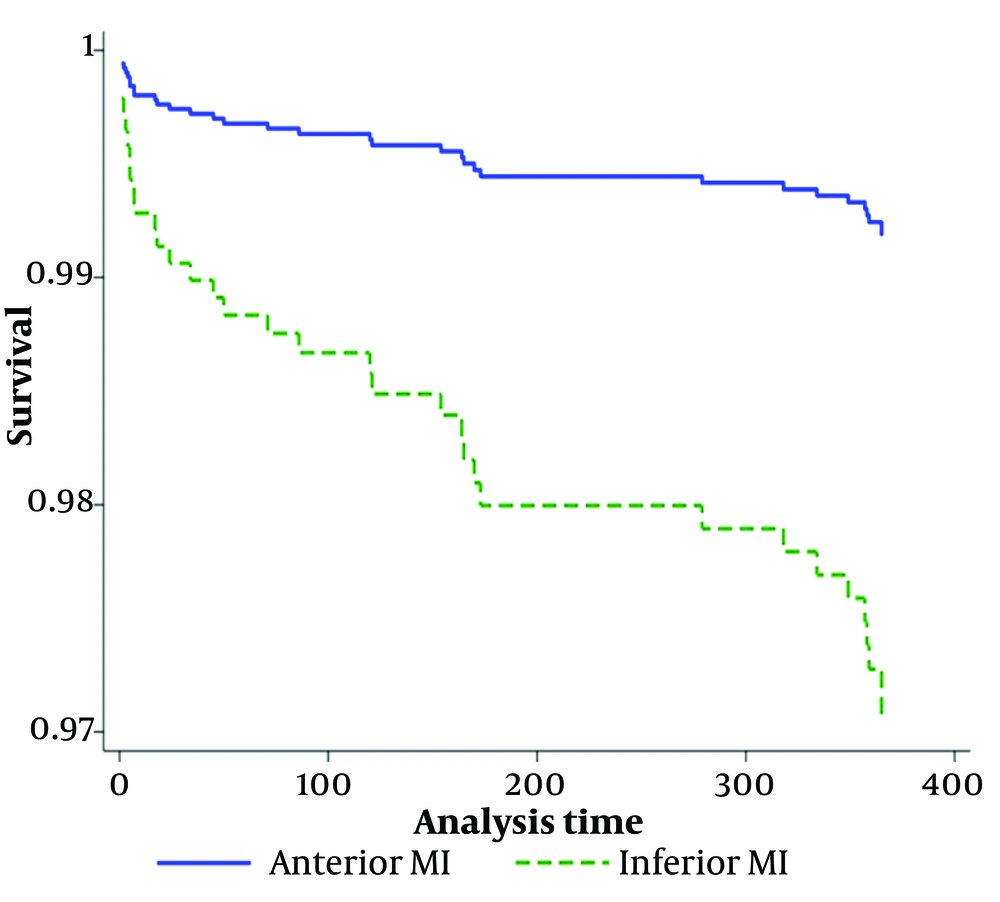
The analysis conducted using the multivariate Cox survival methodology to identify predictors of long-term mortality is presented in Table 2. After adjusting for age and sex, it was found that inferior STEMI cases had poorer outcomes, with a hazard ratio of 1.28 (95% CI: 0.70 - 2.38). Even after comprehensive adjustment for all variables, inferior STEMI remained associated with adverse outcomes, showing a hazard ratio of 3.63 (95% CI: 1.23 - 10.74). Kaplan-Meier curves depicting long-term survival for the two groups are shown in Figure 1.
| Variables | Crude; HRs (95%CI) | Model 1; HRs (95%CI) | Model 2; HRs (95%CI) |
|---|---|---|---|
| Anterior myocardial infraction | Reference | Reference | Reference |
| Inferior myocardial infraction | 1.093 (0.60 - 1.99) | 1.28 (0.70 - 2.38) | 3.63 (1.23 - 10.74) |
a Data are hazard ratios (HRs) with 95% confidence intervals (95%CIs).
b Model 1 = adjusted by sex and age.
c Model 2 = full adjusted.
5. Discussion
The current investigation examined the relationship between 1-year survival in anterior and inferior STEMI patients. The results show that the mortality rate in the inferior group is about one time higher than that in the anterior group.
The site of the infarct itself may independently affect the prognosis. Some recent studies have hypothesized that inferior wall STEMI can be associated with a significantly higher risk of mortality than anterior wall STEMI, based on long-term evaluations (5). It has been shown that the infarct location can influence early outcomes but not long-term prognosis (8). Inferior myocardial infarctions that cause substantial myocardial damage are usually large and often include right ventricular involvement, a factor that influences long-term prognosis (9). Additionally, patients with inferior wall acute MI are more prone to atrioventricular nodal conduction issues (10). Several complicating factors can increase the mortality of inferior MI, including right ventricular infarction, heart block, and cardiogenic shock (11, 12).
The current study found that patients with inferior wall MI had a higher rate of previous CABG surgery compared to those with anterior wall MI. Furthermore, the number of occluded coronary arteries was significantly higher in the inferior myocardial infarction group. As illustrated in Table 1, 35.63% of inferior wall myocardial infarction patients had three-vessel coronary artery disease, compared to 35.63% of anterior wall myocardial infarction patients. This finding is in accordance with a previous study that found half of the patients with confirmed acute inferior myocardial infarction had three-vessel disease (13).
In our study, primary PCI was the more common reperfusion protocol in the anterior group, although this difference was not statistically significant. It has been reported that patients with anterior wall MI treated with primary PCI have better clinical outcomes than patients with other types of MI (14). Additional research has demonstrated that PCI produces better outcomes compared to fibrinolytic therapy for patients suffering from MI, particularly when the MI affects the anterior wall of the heart (15).
This study demonstrates several strengths that enhance its validity and impact. First, the use of a large and well-defined cohort of 643 patients with STEMI from a single hospital registry ensures a robust dataset for analysis. The study’s design, including the use of Cox proportional hazards models, allows for a detailed examination of the impact of anterior versus inferior STEMI on one-year all-cause mortality while controlling for a comprehensive range of confounding variables. Rigorous data collection methods, including physician-validated self-reports and detailed follow-up procedures with a low rate of loss to follow-up, contribute to the reliability of the findings. Additionally, adherence to STROBE guidelines and the careful handling of missing data further bolster the study’s credibility. Collectively, these strengths provide a solid foundation for understanding the effects of STEMI location on mortality outcomes and contribute valuable insights to the field of cardiovascular research.
However, the study has some limitations, including being a single-center experience, the use of self-reported data for conditions such as hypertension, and the differing number of patients in the two groups.
5.1. Conclusions
Regarding the angiographic reports, inferior wall MI is associated with a greater number of involved coronary vessels and an increased risk of mortality, suggesting that the location of MI can predict long-term mortality.