1. Background
Cardiopulmonary bypass (CPB) surgery has been shown to significantly disrupt the body’s homeostasis, with complications such as infection closely related to these disturbances. During CPB, the body undergoes a complex systemic inflammatory response, whose mechanisms remain poorly understood. This response has been attributed to various factors, including endothelial activation and dysfunction (1, 2), the immunomodulatory effects of anesthetics (1), cardiovascular and immunomodulatory impacts of anticoagulants (3, 4), perioperative factors such as extracorporeal membrane oxygenation, complement activation, and surgical trauma (5), and ischemia-reperfusion injury, which can independently induce inflammation (6). Other contributing factors include hypothermia and blood loss, both of which further stimulate the immune response (5).
The interaction among these factors triggers a pro-inflammatory response mediated by endothelial cells and neutrophils and their associated cytokine pathways (7), while simultaneously inducing a compensatory anti-inflammatory response. This anti-inflammatory phase results in peripheral immunosuppression through lymphocyte apoptosis, shifts in monocyte populations and functions, and their respective cytokine pathways (8). The balance, or imbalance, between these pro-inflammatory and anti-inflammatory responses has critical clinical implications: In patients who develop a SIRS-like state, mortality rates are significantly higher when elevated levels of IL-6 and IL-8, two key pro-inflammatory cytokines, are present (9).
Understanding the balance between these opposing inflammatory pathways is challenging due to their complex interactions, yet it is essential for evaluating how immune responses influence clinical outcomes after CPB. Neutrophils, lymphocytes, and monocytes play crucial roles in the inflammatory response and are thus promising targets for studying the body’s response to CPB (10). Both cell types are activated upon exposure to plasma from patients undergoing CPB (11).
The neutrophil-to-lymphocyte ratio (NLR) is one potential marker for assessing the inflammatory response, as it compares the relative levels of neutrophils to lymphocytes in circulating blood. An elevated NLR has been reported in cases of systemic inflammation, cardiac disorders, gastrointestinal cancers, and acute kidney injury (12, 13). Higher NLR values have been associated with poorer outcomes in adult populations undergoing CPB (14) and are also correlated with extended ICU stays and intubation time in pediatric patients (15). This suggests that NLR reflects important aspects of the inflammatory and immune response induced by CPB, capturing the balance between pro-inflammatory and anti-inflammatory activity, which carries significant clinical implications.
2. Objectives
The purpose of this study was to assess the prognostic value of measuring NLR in pediatric patients undergoing CPB.
3. Methods
This retrospective observational study was conducted at the Children’s Medical Center in Tehran, covering the period from November 2021 to November 2022. We aimed to measure NLR in patients undergoing CPB and evaluate its association with major outcomes, including overall mortality, ICU length of stay, and hours of mechanical ventilation. The study included all patients under 18 who underwent CPB for structural cardiac conditions during this period, with follow-up lasting until ICU discharge. Exclusion criteria were applied to cases with incomplete data.
Patient medical records were reviewed to gather data on age, ICU length of stay, hours of mechanical ventilation, and pre- and postoperative blood counts. For each patient, a white blood cell count with differential was obtained the day prior to surgery and again following the procedure. Any operative or postoperative complications were documented by the surgical and ICU teams.
The sample size was calculated with a 0.05 margin of error for a 95% confidence interval, considering a 20% complication rate based on prior studies (6), resulting in a minimum sample size of 246. This study ultimately included 416 patients.
Microsoft Excel (Microsoft Office 2019) was used for data arrangement and arithmetic operations required in calculating ratios and differences. IBM SPSS software (version 25.0) was used for conducting statistical analysis, including independent t-tests for quantitative variables such as length of ICU stay, duration of mechanical ventilation, and the blood cell count. A value of P < 0.05 was used as the cutoff level for statistical significance. Pearson correlations were calculated among the NLR, NCI and outcome variables, along with their P-values.
Our study was reviewed and approved by the Tehran University of Medical Sciences (IR.TUMS.CHMC.REC.1400.135).
3.1. Data
There were 448 cases of CPB patients at Children’s Medical Center Hospital from November 2021 to November 2022. Total white blood cell counts, neutrophil counts, and lymphocyte counts were collected 1 day preoperatively and 1 day postoperatively, along with patient age, days in the ICU, hours of mechanical ventilation, and associated postoperative complications. Laboratory studies were conducted on patients the day before the operation and immediately following the operation, while complications were assessed by the surgical and critical care teams. Of the 448 cases, 32 were excluded due to incomplete data, resulting in a total sample size of 416.
The primary outcome was complications and mortality during ICU admission, with secondary outcomes including the length of intensive care stay and duration of mechanical ventilation.
The data were categorized into three groups: Patients without complications (NC group), patients with postoperative complications excluding mortality (SC group), and the group of deceased patients (EXP group). The SC and EXP groups do not overlap, and complications experienced by the EXP group are included in the overall rate of complications.
3.2. Statistical Analysis
Data management and statistical analysis were performed using Microsoft Excel 2019 and IBM SPSS 25.0 software. Statistical sample analysis was conducted on the data sets, including independent t-tests to identify differences between groups, and Pearson correlations to examine relationships between variables. A value of P < 0.05 was used as the cutoff level for statistical significance. Pearson correlation coefficients were calculated among the NLR, NCI, and outcome variables.
The neutrophil-lymphocyte ratio (NLR) was calculated for both preoperative and postoperative days. The primary focus of this study was the magnitude of the NLR and the change in NLR between these two time points. The change in NLR from the preoperative to the postoperative measurement is defined as the NLR Change Index (NCI) for the purposes of this study.
The mean and standard deviation were calculated for age, ICU stay, mechanical ventilation time, and all NLR measurements. Independent-sample t-tests were used to determine statistical significance between the NC, SC, and EXP groups. For calculations related to overall mortality risk, the surviving groups (NC and SC) were combined into a single group for comparison with the EXP group.
Correlation coefficients were calculated between the postoperative NLR, ICU stay length, and mechanical ventilation time, and these results are presented in Table 1.
| Variables Pair | Pearson Correlation | P-Value |
|---|---|---|
| NLR + ICU | -0.071 | 0.151 |
| NLR + MV | 0.097 | 0.049 |
| NCI + ICU | -0.140 | 0.004 |
| NCI + MV | -0.156 | 0.002 |
Correlation Coefficients Between Neutrophil-to-Lymphocyte Ratio and ICU Stay, and NLR and Mechanical Ventilation Time
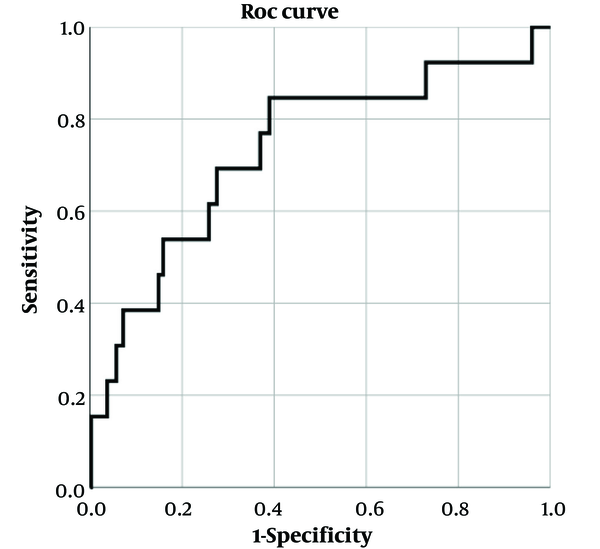
A ROC curve was generated to assess the relationship between the NCI and mortality, with the 13 mortality cases considered positive results. The test variable was the NCI, with smaller values being considered more likely to indicate positive results. This ROC curve is shown in Figure 1.
4. Results
This study included a total of 416 patients, ranging in age from 2 days to 17 years, with an average age of 27.2 months. Age was significantly higher in the NC group (P = 0.002), while no significant age differences were observed between the SC and EXP groups (P = 0.795). Among the 416 patients, 317 experienced no complications and were classified into the NC group; 86 experienced non-fatal complications during or following surgery, forming the SC group; and 13 patients died, forming the EXP group. The largest group was the NC group, which was overall older at the time of operation, spent less time in the ICU, and required less mechanical ventilation. The SC and EXP groups were similar in terms of age, ICU stay, and mechanical ventilation time (Table 2).
The NLR was calculated at both the preoperative and postoperative time points, and the NCI was calculated based on the change in NLR from before to after the operation (Table 2). Preoperative NLR was not significantly different between the groups (P = 0.153). The postoperative NLR was highest in the NC group and lowest in the EXP group, although no statistical significance was found in post-surgical NLR magnitude between the three groups (P = 0.773).
| Group/Variables | NC | SC | EXP |
|---|---|---|---|
| N | 317 | 86 | 13 |
| Age, mo | 30.3 ± 38.9 | 17.6 ± 30.1 | 15.7 ± 22.5 |
| ICU stay, d | 6.38 ± 4.0 | 15.38 ± 11.2 | 13.15 ± 9.0 |
| Mechanical ventilation, h | 20.32 ± 29.1 | 56.49 ± 73.5 | 39.61 ± 69.4 |
| Pre-operative N | 3.53 ± 2.65 | 3.93 ± 2.88 | 4.53 ± 3.19 |
| Post-operative N | 8.87 ± 5.28 | 8.03 ± 4.50 | 6.77 ± 3.70 |
| Pre-operative L | 5.29 ± 4.45 | 4.84 ± 2.58 | 4.60 ± 3.26 |
| Post-operative L | 2.96 ± 1.58 | 2.64 ± 1.35 | 3.14 ± 1.49 |
| NLR (pre-surgery) | 1.00 ± 1.19 | 1.14 ± 1.13 | 2.05 ± 2.41 |
| NLR (post-surgery) | 3.715 ± 2.84 | 3.616 ± 2.69 | 2.759 ± 2.57 |
| NCI (change in NLR) | 2.718 ± 2.63 | 2.475 ± 2.68 | 0.709 ± 3.07 |
Measured Secondary Outcomes and Blood Counts in the No-complications, Surviving Complications, and Expiry Groups
For the NCI, all groups exhibited positive NCI values perioperatively, indicating an increase in their NLR. However, the NC and SC groups showed statistically significantly higher NCI values than the EXP group (P = 0.009).
Overall, the NC group had fewer ICU days (6.4 ± 4.0) and fewer hours of mechanical ventilation (20.3 ± 29.1) compared to the other two groups. The SC group had an average of 15.4 ± 11.2 ICU days and 56.4 ± 73.5 hours of mechanical ventilation, while the EXP group had an average of 13.2 ± 9.0 ICU days and 38.5 ± 74.3 hours of mechanical ventilation. The differences in ICU stay length were statistically significant between the NC group and the other two groups (P < 0.001), but not between the SC and EXP groups (P = 0.495). Mechanical ventilation time showed a similar pattern, with significant differences between the NC group and the others (P < 0.001), but no statistically significant difference between the SC and EXP groups (P = 0.651).
5. Discussion
5.1. Neutrophil-to-Lymphocyte Ratio and Neutrophil Change Index
All three groups in our study showed an increase in the NLR following surgery, with post-surgical NLR being significantly higher across all groups. However, our study did not find a significant difference between the groups based on post-operative NLR alone. While all groups experienced an overall increase in NLR from preoperative to postoperative values, the EXP group exhibited the smallest overall change, as measured by the Neutrophil Change Index.
The more notable finding is the dynamic change in NLR surrounding the CPB procedure, as measured by the NCI. The NC and SC groups had statistically significantly higher NCI values than the EXP group (P = 0.037 and P = 0.032). In other words, the NC and SC groups showed larger increases in their neutrophil population proportions perioperatively, while the EXP group also demonstrated a positive NCI but still had a significantly lower NCI compared to the two surviving groups.
Prior studies have described elevated postoperative NLR as an independent risk factor for postoperative complications (14). In our study, however, the NLR was not found to be statistically related to the overall risk of complications (P = 0.513) or to mortality (P = 0.237). Furthermore, the NCI was more significantly related to mortality (P = 0.009) but not to other complications (P = 0.122).
The ROC curve (Figure 1) relating NCI to mortality among patients showed an AUC of 0.734 with a 95% confidence interval.
5.2. Ventilation and ICU Stay
The NC group had fewer hours of mechanical ventilation and shorter ICU stays overall. The NC group showed statistically significant differences compared to both the SC and EXP groups (P = 0.003 and P = 0.019). However, the length of ICU stay and mechanical ventilation time between the SC and EXP groups were not significantly different. While both groups experienced complications requiring longer stays and extended care, the surviving SC group had a higher NCI than the EXP group (P = 0.032).
The NLR was not correlated with the length of ICU stay, and it showed only a weak positive correlation with mechanical ventilation time. The NCI, on the other hand, was more strongly correlated with ICU stay and mechanical ventilation time, showing negative correlations with both (Table 2). A lower NCI was correlated with longer ICU stays and mechanical ventilation times (P = 0.004 and P = 0.002).
Previous studies have shown a correlation between the NLR and the length of mechanical ventilation and ICU stay (15, 16). Higher postoperative NLR has been shown to be significantly related to both the length of ICU stay and mechanical ventilation time (14).
In contrast, our study found that while the NLR increased significantly from preoperative to postoperative time points, the magnitude of the postoperative NLR was not statistically different among the groups. The NLR was only found to be significantly correlated with mechanical ventilation time, and not with ICU stay (Table 2).
5.3. Complications
In this study, the SC group represents a non-fatal complication rate of 20.7%, and the EXP group represents a 3.1% mortality rate, for a combined overall complication rate of 23.8% (99 cases). Of the 99 patients who experienced complications of any kind, the most common were the need for reintubation within 48 hours of extubation (20.2%), cardiac arrhythmia (20.2%), chorea (15.2%), seizure (12.1%), phrenic nerve palsy (11.1%), and chylothorax (12.1%). Infections (8.1%) and intracranial hemorrhage (ICH) (4.0%) were less frequent but still present.
Other studies have reported similar complication rates for pediatric CPB procedures, typically around 20% (6). Our study had an overall complication rate of 23.8%, including mortalities.
5.4. Final Words
A lower NCI was correlated with longer ICU stays and mechanical ventilation times, and our data suggest that the NCI has some value as a discriminative predictive factor for patient mortality (Figure 1). The NCI is significantly related to mortality.
5.5. Conclusions
This study compared three groups of patients who underwent CPB. The NC group experienced fewer complications and, consequently, had shorter ICU stays and better outcomes. Among the patients who experienced complications, including mortality, their care involved more mechanical ventilation and longer ICU stays overall. Most intriguing were the similarities between the SC group and the EXP group, which were found to be statistically similar in terms of ICU stays and mechanical ventilation times. However, the SC group had significantly higher NCI values, indicating a greater postoperative increase in their NLR compared to the EXP group. The magnitude of the NLR was not related to outcomes; however, the perioperative change in NLR (NCI) was correlated with the length of ICU stay, mechanical ventilation time, and risk of mortality. Notably, the NCI was found to be related to mortality but not to overall complications. While NLR increased postoperatively across all groups, patients who had a lower overall increase in NLR showed statistically worse outcomes.
This suggests that the NCI is a more useful tool for patient evaluation than the NLR alone. Monitoring NLR perioperatively and identifying a low NCI could signal the need for early or more aggressive intervention to improve clinical outcomes. The applicability, feasibility, and specifics of such interventions are beyond the scope of this study.
Determining the NLR and NCI for patients undergoing CPB surgery and examining their immune response patterns can help clinicians identify at-risk patients more quickly and guide decisions on which patients may require closer monitoring in the postoperative period. The feasibility and effectiveness of early interventions for these populations is a topic for future research.
5.6. Limitations and Directions for Future Research
Given the demonstrated relationship between NCI and mortality, further research with larger sample sizes is needed to better understand the extent of this correlation. The study of perioperative changes in NLR and other inflammatory markers remains an evolving field, and additional studies are required to explore the significance of biomarker profiles in patients undergoing CPB. Further validation of perioperative NLR values is also necessary for a more precise measurement of its relationship to mortality following CPB.
One important limitation of this study is that patients were not followed up after discharge from the ICU, so their long-term prognosis and risk of complications remain undetermined. While this study provides important insights, conducting a comprehensive long-term follow-up program for all patients is beyond its scope. Additionally, we did not have a validation cohort to confirm the findings related to NLR and NCI in this study. The relatively low sample size of mortality cases is another limitation.