1. Introduction
“Gossypiboma,” also known as “textiloma,” refers to retained surgical items left behind after an operation (1). These items can lead to a wide range of symptoms, from being asymptomatic to causing life-threatening complications, depending on their location and associated issues. Despite their rarity, gossypibomas can mimic malignant masses, posing significant diagnostic challenges. Therefore, they should be considered in the differential diagnosis for postoperative patients with unexplained symptoms. Imaging techniques such as X-ray, CT, MRI, and echocardiography are essential for their detection and management (2).
This case report adds to the current knowledge by detailing the clinical experience of a patient with an intrathoracic gossypiboma following coronary artery bypass graft (CABG) surgery—a rare occurrence with only a few cases documented. It underscores the critical need for meticulous surgical practices to prevent such incidents and serves as a reminder that retained surgical items can manifest years after the initial operation. This case highlights the importance of vigilance and thorough investigation in postoperative patients to ensure early identification and management of such complications.
2. Case Presentation
A 69-year-old female with a history of ischemic heart disease and CABG surgery ten years prior presented with exertional shortness of breath. She had been taking metoprolol, nitrocontin, losartan, and aspirin for ischemic heart disease.
On physical examination, there was an S3 heart sound and a mild systolic murmur, but no acute or alarming findings suggested a diagnosis beyond the underlying heart condition. Her rhythm was regular (80 BPM), blood pressure measured 125/80 in both arms, and body temperature was normal (36.2°C). Laboratory results, including a complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), were all within normal limits, indicating no underlying inflammatory process.
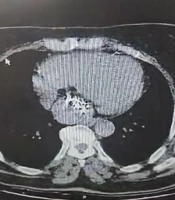
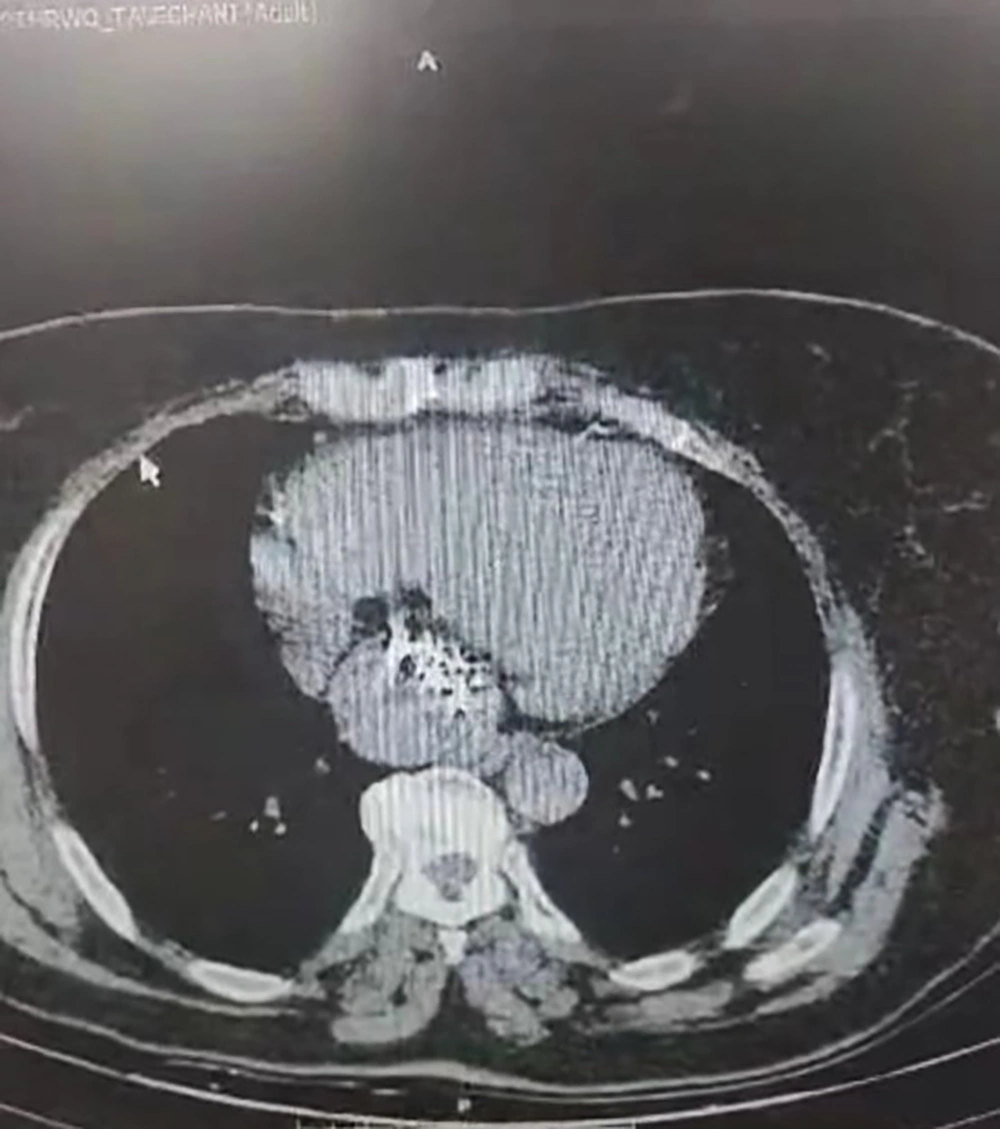
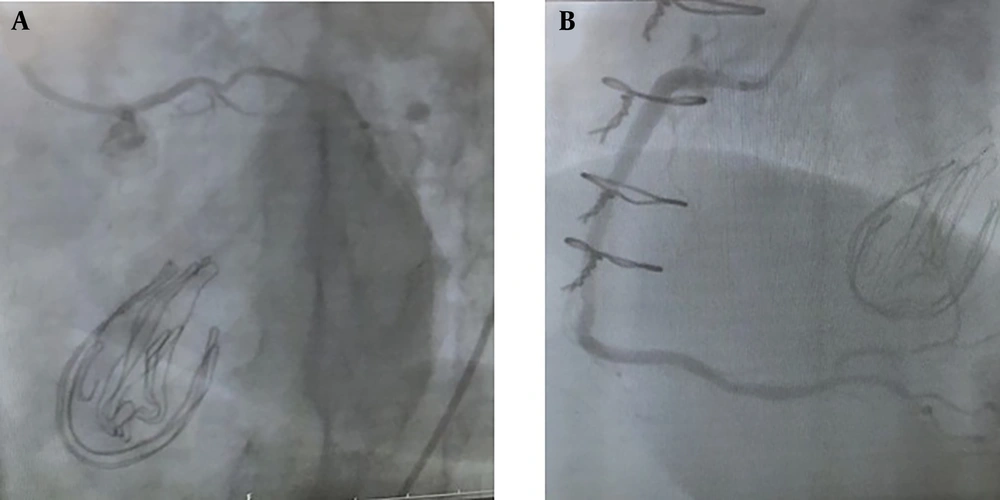
Despite the absence of acute physical signs, echocardiography revealed concerning findings: Mild left ventricular enlargement, moderate systolic dysfunction, moderate left atrial enlargement, and a large immobile mass (4 × 2 cm) in the left atrium. Her ejection fraction (EF) was recorded at 40%, correlating with her dyspnea symptoms. These findings prompted further investigation. Transesophageal echocardiography (TEE) identified a large, immobile, heterogeneous mass (40 × 24 mm) located near the mitral valve (Figure 1). Initially, it was suspected to be within the left atrium (LA), as indicated by TTE and TEE, raising concerns about a possible tumor. A CT scan later revealed the mass to be in the retrocardiac region (Figure 2). To further assess its nature, coronary angiography with fluoroscopy was performed, showing a large mass with a visible radio-opaque line inside, indicative of retained surgical gauze with metallic markers left from her prior CABG surgery (Figure 3).
Given the patient’s stable condition and absence of severe symptoms, surgical removal was deemed unnecessary. Regular follow-ups were recommended. The patient was relieved to learn that the mass was not malignant and agreed to the follow-up plan.
3. Discussion
Masses in the mediastinal area near the heart can arise for various reasons. A common cause is the formation of a pericardial cyst, which typically manifests in individuals in their thirties or forties. These cysts are most often located in either the right or left costophrenic angle. However, they may also appear in the mediastinal region, not necessarily near the diaphragm, or may result from previous thoracic surgery. Other potential causes include rare purulent abscesses in the chest, a pancreatic pseudocyst extending into the thorax, lymphomas, other malignancies, or a foreign object inadvertently retained post-surgery. Such masses often go unnoticed when they are small and situated in the retrocardiac area. Since 23.5% of these masses have the potential to be malignant, prompt diagnosis is essential for effective patient management (3).
One specific type of retained foreign body is known as a “gossypiboma,” a term derived from “Gossypium,” meaning “cotton,” and "bomba," meaning “place of concealment.” It refers to a mass within the surgical site after an operation, comprising a foreign body granuloma encasing a central cotton matrix. Gossypibomas are estimated to occur in 1 out of every 1,000 to 10,000 surgeries, with the most common locations being the abdomen (56%), pelvis (18%), and thorax (11%). Although gossypibomas are most frequently found after intra-abdominal and pelvic surgeries, they can also occur following cardiovascular procedures. Risk factors for gossypiboma include emergency surgeries with prolonged operative time, inexperienced staff, hemodynamically unstable patients, miscommunication during sponge counts, unexpected changes in surgical steps, and patient obesity (1).
Gossypiboma often presents with nonspecific symptoms. The clinical spectrum can vary widely, from being completely asymptomatic (discovered incidentally) to life-threatening, depending on the location and complications associated with the retained foreign object. The clinical and radiological features of intrathoracic gossypibomas can also vary, influenced by factors such as the location and duration of the retained sponge. Intrathoracic gossypibomas are commonly found in the pericardial and pleural cavities (2).
Detecting gossypibomas can be challenging, especially when a radio-opaque marker is present, which can lead to potential misdiagnosis or oversight. In complex or chronic cases, imaging modalities such as ultrasound, CT scans, or MRI are typically employed, as the lesion may mimic a malignant mass. CT scans are particularly useful for identifying radio-opaque foreign bodies and can reveal distinctive signs of gossypiboma, such as a typical spongiform pattern and a heterogeneous, low-density mass with a thin, high-density capsule that shows significant enhancement following contrast administration. Additionally, high-density, striped, wavy areas within the mass often indicate the presence of a retained sponge. MRI is also effective in visualizing the characteristic internal structure of gauze granulomas and can differentiate between inflammatory pseudotumors and neoplastic lesions, further aiding in the accurate diagnosis and management of gossypibomas. In cases where no radio-opaque marker is visible on X-ray or CT, echocardiography may be used to identify an encapsulated mass (4). Transesophageal echocardiography is a valuable imaging technique, allowing precise localization of a mass in the pericardial space, visualizing its relationship with adjacent structures, assessing tissue invasion, and identifying specific features indicative of a foreign body (3). Similarly, coronary angiography is another useful tool for detecting the mass and assessing its characteristics. In some studies, coronary catheterization has been preferred over computed tomography angiography due to its capability to provide detailed information about the tumor’s blood supply, aiding in ruling out alternative differential diagnoses (5, 6).
The treatment approach for a retained foreign body (RFB) depends on the type of item retained and its anatomical location. The potential risks associated with removal must be weighed against the risks of leaving the item in place (7). Surgical exploration is the preferred treatment for gossypibomas in symptomatic patients. However, in certain asymptomatic patients, especially those with a long duration of retention, conservative management may be considered (8). While prior literature has documented cases in which the RFB was surgically removed (3, 8, 9), in this case, given the patient’s stable health status and mild symptoms, the decision was made to leave the gossypiboma undisturbed and to conduct regular follow-ups.
In conclusion, this case report highlights the critical importance of meticulous surgical practices, effective communication, and vigilant postoperative monitoring to prevent the retention of surgical materials, known as gossypibomas. These retained items can cause considerable medical and legal challenges and may present diagnostic difficulties even years after surgery. Errors involving the entire surgical team can lead to mental strain for those involved and potentially damage the reputation of the healthcare providers. Therefore, clear communication and accurate gauze counting in the operating room are essential for preventing such incidents and ensuring patient safety.