1. Background
Cardiovascular diseases are among the most common causes of death in most countries, accounting for more than 30% of deaths in industrialized nations (1-3). Various methods are used to treat these patients, including drug treatments, angioplasty, and coronary artery bypass grafting (CABG). Today, coronary artery surgery is considered the most common treatment method for advanced coronary artery disease (CHD). Statistics from the Tehran Heart Center indicate that approximately 3,000 cases of CABG are performed annually, highlighting its prevalence among individuals with this condition.
The prevalence of depression in individuals diagnosed with CHD ranges from 20% to 40%, while anxiety levels in these patients range from 20% to 55%. Similar rates have been reported in patients undergoing CABG (4-6). Depression, anxiety, or a combination of these two conditions independently increases the risk of cardiovascular diseases, regardless of other demographic and clinical risk factors. In patients undergoing CABG, symptoms of depression, mortality, and fatal cardiac events occur more frequently. Patients with depression before CABG have a 50% to 100% higher risk of death compared to those without depression. Research indicates that the prevalence of depression before CABG is 47%, increasing to 61% post-surgery (5, 6). A 2016 study reported a depression rate of 1.17% in patients undergoing heart surgery. Findings showed that patients experiencing depression before CABG continue to suffer from it for a longer period after the operation (7-9).
Cardiac rehabilitation aims to reduce risks through individual and group training and physical activity, with the goal of improving quality of life, returning the patient to pre-illness life, enhancing psychosocial status, facilitating recovery, and preventing cardiac events. Most studies indicate that patients in rehabilitation programs after cardiac surgery experience reduced depression and anxiety and improved quality of life. Cardiac rehabilitation includes three stages: The first stage may begin with the diagnosis of arteriosclerosis, involving low-level activities and basic education for the patient and their family. The second stage occurs after hospital discharge, typically lasting 4 - 6 weeks, and includes monitoring the patient’s actions and providing education and counseling related to lifestyle modification to reduce risk factors. The third stage focuses on maintaining cardiovascular stability and physical conditions over the long term (10, 11).
Given the increasing prevalence of cardiovascular diseases and the common use of CABG as a treatment method, as well as the high incidence of depression in these patients, it is essential to pay special attention to the psychological issues related to these patients. Depression symptoms are chronic and, with the progression of cardiovascular disease, lead to poor prognosis, inadequate physical performance, reduced quality of life, and negative effects on treatment outcomes. Additionally, the necessary training and rehabilitation for these patients are often incomplete and ineffective (12, 13).
2. Objectives
Therefore, the present study aimed to evaluate the effect of cardiac rehabilitation on anxiety and depression in patients undergoing coronary artery bypass surgery at Golestan Hospital, Ahvaz.
3. Methods
This study was an interventional and experimental study with two pre-test and post-test groups, investigating the effect of the independent variable of cardiac rehabilitation on the dependent variables of anxiety and depression in patients after coronary artery bypass surgery at Golestan Hospital in Ahvaz city. The study was conducted in three stages: Before, immediately after, and two months after the intervention. The research population included 80 patients who underwent coronary artery bypass surgery. Patients were selected based on specific inclusion criteria, such as age between 40 and 80 years, ejection fraction above 40% (verified by echocardiography and cardiology examinations), history of coronary artery surgery, ability to read and understand educational materials, and capacity to participate in exercises and sessions.
Patients were assigned to experimental and control groups using random sampling. In the experimental group, cardiac rehabilitation was performed over 8 sessions, including both exercise and educational programs conducted twice a week for 4 weeks (2 hours per session). The training focused on medication adherence, dietary guidelines, weight and stress management, smoking cessation, and relaxation techniques. The content of these sessions was developed by experts based on reliable sources. The control group received only standard care without additional interventions. After the intervention, participants in the control group were provided with an educational questionnaire and referred for rehabilitation. If patients required urgent education or rehabilitation during the study, they were tested and excluded from the analysis.
3.1. Exclusion Criteria Included
history of mental-psychiatric disorders, attendance at prior rehabilitation programs, death or disease relapse during the study, disabilities preventing participation, prior heart surgery, use of sedatives or anti-anxiety medications, and prior engagement in activities like yoga or meditation. Participants reporting severe pain or depression were referred to specialists and excluded from further participation if necessary.
Data collection tools included demographic questionnaires as well as Spielberger’s Anxiety Inventory and Beck’s Depression Inventory. Demographic data comprised age, sex, marital status, occupation, and place of residence. The anxiety questionnaire consisted of 35 items rated on a 5-point Likert scale (e.g., never, rarely, sometimes, most of the time, always). Scores below 70 indicated low anxiety, while scores of 70 - 105 reflected moderate impairments in functioning (14, 15). The Beck Depression Inventory contained 30 items reflecting symptoms of depression. Responses ranged from 0 (no symptom) to 3 (severe symptom), yielding total scores between 0 and 90. Scores below 21 indicated health, scores between 22 - 53 reflected mild-to-moderate depression, and scores above 53 indicated severe depression (16). Psychometric properties of the inventory in an Iranian sample demonstrated high reliability, including an alpha coefficient of 0.91, a correlation between test halves of 0.89, and a retest coefficient of 0.94 (17, 18).
3.2. Statistical Analysis
Data analysis was performed using SPSS version 24, provided under a valid institutional license by Ahvaz University of Medical Sciences. Statistical methods included:
3.2.1. Repeated Measures ANOVA
To evaluate changes in anxiety and depression over the three measurement time points.
3.2.2. Independent <i>t</i>-Tests
To compare differences between the intervention and control groups.
3.2.3. Effect Sizes and Confidence Intervals
Calculated using Cohen’s d to determine the magnitude of observed effects and the precision of the estimates.
3.3. Ethical Considerations
The study protocol was approved by the Ethics Committee of Ahvaz University of Medical Sciences. All participants provided informed consent, and confidentiality of personal data was maintained throughout the study.
4. Results
4.1. Demographic Characteristics
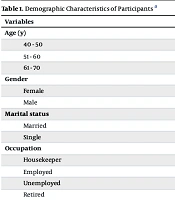
The demographic data of the participants are summarized in Table 1. The mean age of participants in the control group was 53.4 ± 2.8 years, while in the experimental group, it was 54.8 ± 3.1 years, indicating no statistically significant difference between the two groups in terms of age distribution. Participants were categorized into three age groups: 40 - 50 years, 51 - 60 years, and 61 - 70 years. In the control group, 22.5% of the participants were in the 40 - 50 age group, 42.5% were in the 51 - 60 age group, and 35% were in the 61 - 70 age group. Similarly, the experimental group showed a comparable distribution of age with 20%, 45%, and 35% in these respective age categories (P = 0.585).
| Variables | Experimental Group | Control Group | P-Value |
|---|---|---|---|
| Age (y); mean ± SD | 54.8 ± 3.1 | 53.4 ± 2.8 | 0.585 |
| 40 - 50 | 8 (20) | 9 (22.5) | |
| 51 - 60 | 18 (45) | 17 (42.5) | |
| 61 - 70 | 14 (35) | 14 (35) | |
| Gender | 0.765 | ||
| Female | 15 (37.5) | 17 (42.5) | |
| Male | 25 (62.5) | 23 (57.5) | |
| Marital status | 0.495 | ||
| Married | 35 (87.5) | 34 (85) | |
| Single | 5 (12.5) | 6 (15) | |
| Occupation | 0.322 | ||
| Housekeeper | 10 (25) | 9 (22.5) | |
| Employed | 17 (42.5) | 13 (32.5) | |
| Unemployed | 9 (22.5) | 9 (22.5) | |
| Retired | 4 (10) | 9 (22.5) | |
| Education | 0.535 | ||
| Below diploma | 27 (67.5) | 24 (60) | |
| Diploma and higher | 13 (32.5) | 16 (40) |
Demographic Characteristics of Participants a
Regarding gender, the proportion of males was slightly higher in both groups. In the experimental group, 25 participants (62.5%) were male, and 15 (37.5%) were female. Similarly, in the control group, 23 participants (57.5%) were male, and 17 (42.5%) were female (P = 0.765).
In terms of marital status, the majority of participants in both groups were married. In the experimental group, 35 participants (87.5%) were married, while 5 (12.5%) were single. In the control group, 34 participants (85%) were married, and 6 (15%) were single. These differences were also not statistically significant (P = 0.495).
Educational attainment revealed that most participants in both groups had an educational qualification below a diploma level. In the experimental group, 67.5% of the participants had education below a diploma, and 32.5% had a diploma or higher qualification. Similarly, in the control group, 60% of the participants had education below a diploma, and 40% had a diploma or higher (P = 0.535).
Occupation status showed that in the experimental group, 42.5% of participants were employed, 25% were housekeepers, 22.5% were unemployed, and 10% were retired. In the control group, 32.5% were employed, 22.5% were housekeepers, 22.5% were unemployed, and 22.5% were retired. This distribution revealed no significant difference between the two groups (P = 0.322).
Overall, the demographic data confirmed that there were no significant differences between the control and experimental groups, ensuring comparability at baseline.
4.2. Anxiety and Depression Scores
4.2.1. Before the Intervention
The baseline scores for anxiety and depression in both groups were similar, with no statistically significant differences observed (P > 0.05). Specifically, the mean anxiety score in the experimental group was 35.20 ± 8.3, compared to 36.45 ± 6.3 in the control group (P = 0.202). Similarly, the mean depression score was 15.25 ± 3.3 in the experimental group and 14.90 ± 2.8 in the control group (P = 0.252).
4.2.2. Post-intervention and Two-Month Follow-up
Anxiety scores showed a decrease in both groups over time, with the experimental group demonstrating a more pronounced reduction. The mean anxiety score in the experimental group dropped to 29.70 ± 3.3 post-intervention and further decreased to 25.65 ± 6.3 at the two-month follow-up. In the control group, anxiety scores reduced to 31.90 ± 4.3 post-intervention and 29.78 ± 5.3 at the follow-up. Although anxiety levels decreased over time in both groups (P < 0.001 for time effect), the difference between the two groups did not reach statistical significance (P = 0.065).
Depression scores, however, showed a significant reduction in the experimental group compared to the control group. In the experimental group, depression scores dropped from 15.25 ± 3.3 at baseline to 10.65 ± 5.6 post-intervention and 5.85 ± 3.45 at follow-up. In contrast, the control group’s depression scores decreased from 14.90 ± 2.8 to 12.30 ± 3.6 post-intervention and 8.59 ± 4.35 at follow-up. Statistical analysis revealed a significant difference between the two groups in depression reduction (P = 0.025), as well as a significant interaction between time and group (P < 0.001). Table 2 presents a comparison of anxiety and depression scores.
| Variables and Groups | Before Intervention | Immediately After the Intervention | Two Months After the Intervention | P-Value | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | P-Value | Mean ± SD | Mean ± SD | Time | Group | Time and Groups | |
| Anxiety | 0.202 | < 0.001 | 0.065 | 0.005 | |||
| Test | 35.20 ± 8.3 | 29.70 ± 3.3 | 25.65 ± 6.3 | ||||
| The witness | 36.45 ± 6.3 | 31.90 ± 4.3 | 29.78 ± 5.3 | ||||
| Depression | 0.252 | < 0.001 | 0.025 | < 0.001 | |||
| Test | 15.25 ± 3.3 | 5.6 ± 10.65 | 3.45 ± 5.85 | ||||
| The witness | 2.8 ± 14.90 | 3.6 ± 12.30 | 4.35 ± 8.59 | ||||
Comparison of Anxiety and Depression Scores
5. Discussion
The present study investigated the effect of cardiac rehabilitation on anxiety and depression in 80 patients undergoing coronary artery bypass surgery at Golestan Hospital, Ahvaz University of Medical Sciences. The findings confirmed that cardiac rehabilitation significantly reduced depression, while the reduction in anxiety, although notable, was not statistically significant. These results are consistent with prior studies, emphasizing the psychological benefits of rehabilitation programs. Duarte Freitas et al. demonstrated that a 4-week intensive rehabilitation program could lead to substantial reductions in anxiety and depression, along with improvements in quality of life and sleep quality (19). Similarly, Choi et al. highlighted the antioxidative benefits of rehabilitation, indirectly contributing to psychological well-being (20). Kalko et al. further noted that even short-term rehabilitation programs can positively impact mental health outcomes (21). These findings reinforce the importance of structured interventions for improving patient recovery.
Regarding depression, the results align with the findings of Hazavehei et al., who highlighted the effectiveness of educational programs involving relaxation and breathing exercises in reducing depression among CABG patients (22). Another study also observed that long-term rehabilitation programs not only improved psychological outcomes but also sustained these benefits over 12 months, suggesting that extended durations may maximize effectiveness. In contrast, Lie et al. focused on home-based rehabilitation and found significant reductions in both anxiety and depression, particularly when tailored to individual patient needs (23).
The reduction in anxiety, while not statistically significant, highlights the complexity of addressing this psychological state. Rymaszewska and Kiejna noted that anxiety levels often decrease immediately after surgery but may resurface in the months following recovery, necessitating ongoing psychological support (24). Dugmore et al. and Lavie and Milani both emphasized the need for multifaceted approaches, combining physical training, psychological counseling, and social support to achieve meaningful improvements in anxiety levels (25, 26).
Physiological and psychological mechanisms play a critical role in these outcomes. Regular physical activity, as part of rehabilitation programs, has been shown to increase endorphin levels, enhance cardiovascular function, and reduce inflammation, all of which contribute to improved mental health (27). Group sessions within these programs foster a sense of community and reduce feelings of isolation, further enhancing psychological recovery (28).
Cultural and social factors also significantly influence rehabilitation outcomes. The marital status of participants, as observed in this study, provided a stable support system, contributing positively to psychological well-being. This aligns with the findings of Kulcu et al., who noted that incorporating family involvement into rehabilitation programs enhances patient outcomes (27). Sharif et al. also emphasized the importance of culturally tailored interventions to address unique patient needs in non-western settings (29).
Comparison with other studies highlights the robustness of the findings. For example, Duarte Freitas et al. and Yoshida et al. emphasized the long-term benefits of rehabilitation for depression, while Sharif et al. suggested that extending the duration of programs could yield more significant results for anxiety (19, 29, 30). Michie et al. also noted that psychological improvements post-rehabilitation correlate strongly with health outcomes and behavioral changes, reinforcing the broader impact of such programs (31).
5.1. Conclusions
Cardiac rehabilitation effectively reduces depression and shows promise for reducing anxiety in patients post-CABG surgery. Short-term programs demonstrate clear benefits; however, extending intervention durations and incorporating culturally tailored, family-centered approaches could further enhance outcomes. These findings support the integration of cardiac rehabilitation into standard post-operative care to comprehensively address both physical and psychological recovery.
5.2. Limitations
One limitation of this study is the relatively small sample size, which may limit the generalizability of the findings. Additionally, the single-center design restricts the applicability of results to broader populations. The reliance on self-reported questionnaires may also introduce response bias, as participants’ individual differences in understanding or emotional states could affect their answers. Future research should address these limitations by incorporating larger, multi-center samples and employing objective psychological assessments alongside self-reported measures.