1. Background
Congenital heart disease (CHD) refers to a spectrum of structural abnormalities in the heart and great vessels present at birth due to improper development during embryogenesis (1). These defects can range from minor abnormalities, such as a small ventricular septal defect, to complex malformations like hypoplastic left heart syndrome or transposition of the great arteries (2, 3). The global incidence of CHD is estimated to be between 8 and 12 per 1,000 live births, making it one of the most common congenital anomalies worldwide (4, 5). A meta-analysis revealed an overall CHD prevalence of 2.5 per 1,000 live births in Iran. Notably, the prevalence of CHD in Iran is lower than the global rates. However, the study also highlighted that the prevalence of CHD in Iran continues to rise, signaling a growing concern. This trend underscores the need for increased attention to CHD as a significant health challenge in Iran (6).
Depending on the nature and severity of the anomaly, CHD can significantly impair normal cardiac function, leading to compromised blood flow and oxygen delivery (7, 8). Children with CHD often experience delays in physical growth and neurodevelopment (9-11). The condition also imposes a substantial psychosocial and financial burden on families, as managing CHD often involves long-term medical care, repeated hospitalizations, and surgical interventions (12-14).
Surgical intervention is a cornerstone in the management of CHD. Open-heart surgery, which often requires the use of cardiopulmonary bypass (CPB), is employed to correct many structural heart defects (15-18). Over the past few decades, advances in surgical techniques, perioperative care, and postoperative management have drastically improved the survival rates of pediatric patients undergoing cardiac surgery (18, 19). Currently, survival rates for CHD surgeries now exceed 97% (20).
Despite the life-saving potential of cardiac surgery, it is not without risks (21-23). The surgical correction of CHD, particularly using CPB, places considerable stress on the body, triggering systemic inflammatory responses, hemodynamic instability, and organ dysfunction (24, 25). While significant focus has been placed on the cardiovascular and neurological complications associated with pediatric cardiac surgery (26-28), gastrointestinal (GI) complications remain a less explored aspect of postoperative care.
The GI system is highly susceptible to the physiological challenges posed by open-heart surgery, particularly in pediatric patients. Factors such as low cardiac output, hypoperfusion, systemic inflammatory response syndrome, and the effects of CPB can compromise intestinal perfusion, increasing the risk of GI complications (29, 30). These complications can range from mild issues, such as feeding intolerance, to severe and potentially life-threatening conditions, including necrotizing enterocolitis (NEC), GI bleeding, and intestinal ischemia (29-31). The GI complications not only delay recovery and prolong hospitalization but can also significantly increase mortality (32). Evidence also suggests that GI complications are associated with increased rates of renal failure, new-onset dialysis dependency, multisystem organ failure, and deep sternal wound infections (33).
Understanding the incidence and risk factors of GI complications is critical for improving perioperative care and overall outcomes for children undergoing cardiac surgery. While a few studies in high-resource settings have provided valuable insights into these complications (29, 30), data from low- and middle-income countries, including Iran, remain scarce. In these regions, resource limitations and differences in perioperative practices may influence the incidence of GI complications, underscoring the need for context-specific research.
2. Objectives
This study aimed to investigate the incidence of GI complications in pediatric patients undergoing open-heart surgery in a tertiary care center in Iran.
3. Methods
3.1. Study Design and Setting
This retrospective study was conducted at the Children's Medical Center Hospital, affiliated with Tehran University of Medical Sciences. It is the largest pediatric cardiac surgery hospital in Iran and serves as a major referral center for complex cases from across the country.
3.2. Study Population
The study included all pediatric patients aged 1 day to 18 years with CHD who underwent open surgery and were subsequently admitted to the open heart ICU between September 23, 2021, and September 22, 2022. Inclusion criteria encompassed all pediatric patients within the defined age range who underwent cardiac surgery and were admitted to the ICU postoperatively. Patients were excluded if their medical records had missing data related to the variables of this study, if they experienced mortality in the operating room before ICU admission, or if they had documented GI complications prior to surgery. Excluding patients with pre-existing GI complications ensured that the focus remained on the incidence of complications arising specifically after cardiac surgery.
3.3. Data Collection
Data for this study were extracted retrospectively from patient medical records using a structured checklist. The checklist recorded demographic and clinical information, including age, gender, risk adjustment for congenital heart surgery (RACHS-1), duration of cardiopulmonary bypass, type of GI complication, and length of ICU stay.
3.4. Sample Size
The study included all 441 eligible pediatric patients who underwent cardiac surgery during the specified one-year period at the Children's Medical Center Hospital.
3.5. Data Analysis
The collected data were analyzed using SPSS version 21. Descriptive statistics, including the mean and standard deviation, were used to summarize continuous variables. Frequencies and percentages were calculated for categorical variables. Inferential statistics were employed to examine associations between variables and outcomes. Independent t-tests were used to compare the means of continuous variables between groups. The chi-square test was applied to categorical variables to determine whether there were significant associations between groups and specific outcomes. A significance level of 0.05 was set for all analyses.
3.6. Ethical Considerations
This study received ethical approval from the Ethics Committee of Tehran University of Medical Sciences (approval No. IR.TUMS.CHMC.REC.1400.088). The study adhered to the ethical principles outlined in the Declaration of Helsinki. To ensure confidentiality, all patient information was anonymized, and no identifiable data were recorded.
4. Results
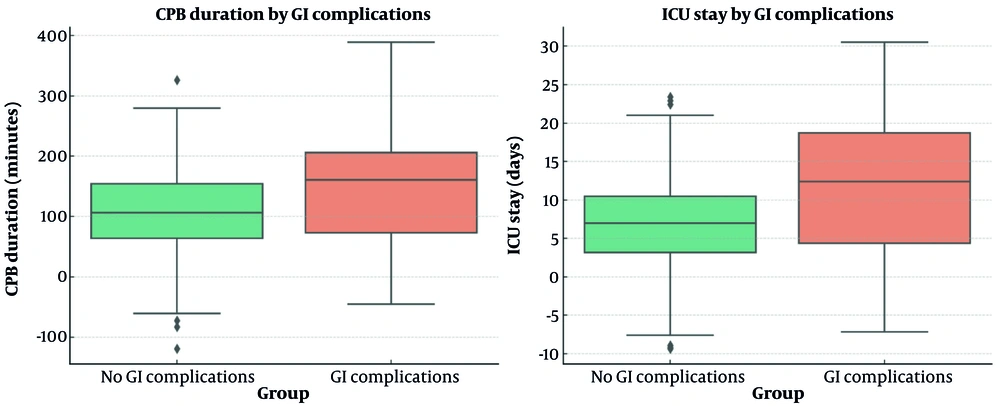
Among 441 pediatric patients undergoing open-heart surgery, 46 cases (10.4%) were identified as experiencing postoperative GI complications. The most common complication was vomiting, observed in 16 cases (34.78%), followed by chylothorax in 11 cases (23.91%) (Table 1). Gastrointestinal complications were distributed across different age groups without a statistically significant difference (P = 0.56). Gender was also not significantly associated with GI complications, with 24 cases (10.9%) occurring in males and 22 cases (9.9%) in females (P = 0.72). Risk adjustment for congenital heart surgery scores showed no statistically significant association with the incidence of GI complications (P = 0.78). The majority of complications occurred in patients with RACHS-1 scores of 2 (56.5%) and 3 (28.3%) (Table 2). Patients with complications had a mean CPB duration of 160 ± 92 minutes, compared to 118 ± 68 minutes in those without complications (P = 0.002). Additionally, the length of ICU stay was significantly longer in patients with GI complications, averaging 11 ± 9 days compared to 7 ± 6 days for those without complications (P < 0.001) (Figure 1).
| Gastrointestinal Complications | Frequency (%) |
|---|---|
| Vomiting | 16 (34.78) |
| Chylothorax | 11 (23.91) |
| Ascites | 4 (8.70) |
| Diarrhea | 4 (8.70) |
| GI Bleeding | 2 (4.35) |
| Choleostasis | 2 (4.35) |
| Portal hypertension and esophageal varices | 1 (2.17) |
| Vomiting with GI bleeding | 1 (2.17) |
| Vomiting with ascites | 1 (2.17) |
| Rectorrhagia | 1 (2.17) |
| Ascites with NEC surgery and jaundice | 1 (2.17) |
| Pancreatitis | 1 (2.17) |
| Chylothorax with vomiting | 1 (2.17) |
| Total | 46 (100) |
Distribution of Gastrointestinal Complications in the Study Population
| Variables and Categories | Without GI Complications | With GI Complications | P-Value |
|---|---|---|---|
| Age (mo) | 0.56 b | ||
| 0 - 1 | 47 (10.7) | 6 (1.4) | |
| 1 - 12 | 155 (35.1) | 17 (3.9) | |
| 12 - 60 | 124 (28.1) | 15 (3.4) | |
| 60 - 120 | 54 (12.2) | 5 (1.1) | |
| > 120 | 14 (3.2) | 4 (0.9) | |
| Gender | 0.72 b | ||
| Male | 196 (44.4) | 24 (5.4) | |
| Female | 201 (45.6) | 22 (5.0) | |
| RACHS-1 | 0.78 b | ||
| 1 | 64 (14.5) | 6 (1.4) | |
| 2 | 208 (47.2) | 26 (5.9) | |
| 3 | 89 (20.2) | 13 (2.9) | |
| 4 | 30 (6.8) | 5 (1.1) | |
| CPB duration (min) | 118 ± 68 | 160 ± 92 | 0.002 c |
| Length of ICU stay (d) | 7 ± 6 | 11 ± 9 | < 0.001 c |
Demographic Variables and Their Association with the Incidence of Gastrointestinal Complications a
5. Discussion
This study investigated the incidence of GI complications in pediatric patients undergoing open-heart surgery for CHD at a tertiary care center in Iran. The findings contribute to understanding a relatively underexplored aspect of pediatric cardiac surgery, particularly in resource-limited settings. The incidence of GI complications was found to be 10.4%, with vomiting (34.78%) and chylothorax (23.91%) being the most common. Consistent with our results, a study conducted in China reported the incidence of GI bleeding in neonates, infants, and children as 22.6%, 2.0%, and 0.5%, respectively (30). In comparison, a study conducted in Iran on adult patients who underwent cardiac surgery reported a lower incidence rate of 4.5% for GI complications (34). Additionally, another study reported an overall rate of 2.4% for GI complications in adult patients after cardiac surgery (33). These findings suggest that pediatric patients may be more prone to GI complications than adults, possibly due to their developing physiological systems and increased vulnerability to surgical and perioperative stress.
The higher incidence of GI complications in pediatric patients compared to adults may be attributed to key physiological differences. Pediatric patients, particularly neonates and infants, have an immature GI system with reduced gastric capacity, underdeveloped mucosal barriers, and an immature enteric nervous system (35-37). These factors make them more susceptible to feeding intolerance, delayed gastric emptying, and other postoperative GI complications. Vomiting and chylothorax were the most common complications, accounting for 34.78% and 23.91% of cases, respectively. Chylothorax is particularly prevalent in pediatric cardiac surgery due to the high risk of lymphatic disruption during surgical procedures, especially near the thoracic duct, which is more delicate and anatomically variable in children (38, 39). Moreover, the use of central venous lines and extensive dissection around the heart and great vessels further increases the risk of chyle leakage (40).
Other GI complications, such as ascites, diarrhea, and GI bleeding, occurred less frequently but highlight the diverse nature of GI issues following cardiac surgery. In comparison, another study that focused on adult patients identified postoperative ileus as the most common GI complication, followed by GI hemorrhage (41). Another study on adults revealed that paralytic ileus, GI bleeding, and acute cholecystitis are the most common GI complications following cardiac surgery (34). The differences between the GI systems of pediatric and adult patients, such as the smaller gastric capacity and the underdeveloped lower esophageal sphincter in neonates, may account for the observed variations. Additionally, the greater sensitivity of the pediatric GI system to stress, surgical interventions, and feeding changes may further contribute to the differences in the prevalence and nature of GI complications between pediatric and adult populations.
In this study, longer CPB duration emerged as a significant risk factor for GI complications. Prolonged CPB is known to exacerbate systemic inflammatory responses and reduce splanchnic perfusion, which may explain its association with GI complications (30, 42). The GI organs receive approximately 20% - 25% of the body's cardiac output and consume 20% of oxygen under normal physiological conditions. Their demand for blood supply significantly increases during stressful situations, such as cardiac surgery. The GI complications during CPB are primarily linked to reduced cardiac output, causing visceral hypoperfusion, mucosal ischemia, and necrosis due to altered splanchnic blood flow (42). Consistent with our results, a systematic review and meta-analysis reported that CPB times were significantly longer in patients with GI complications (43). Additionally, our results align with those of a study conducted on adult patients in Iran (34). The results indicate that patients with GI complications had longer ICU stays, likely reflecting the additional care needed to manage these complications and their adverse effects on recovery. In line with our results, a study of adults revealed that patients with GI complications had significantly higher mortality rates, as well as longer ICU and hospital stays (34).
Demographic variables, including age and gender, showed no significant association with the occurrence of GI complications. Similarly, the absence of a significant association between RACHS-1 scores and GI complications suggests that these factors may not be primary determinants of GI complications. These findings suggest that the occurrence of GI complications is likely influenced more by factors such as postoperative management. This underscores the importance of identifying risk factors and optimizing clinical practices to reduce the incidence of GI complications. Therefore, further studies are needed to better understand the risk factors contributing to these complications.
Given the limited data on GI complications in pediatric cardiac surgery in low- and middle-income countries, this study contributes to the growing body of literature. The study underscores the need for heightened vigilance and proactive management of GI complications in pediatric cardiac surgery patients, particularly in those undergoing prolonged CPB. Additionally, the findings highlight the importance of optimizing perioperative strategies to reduce CPB duration and mitigate its adverse effects.
This study is one of the few to assess the incidence of GI complications in pediatric patients undergoing open-heart surgery. Its strength lies in being conducted at a major referral hospital that admits patients from across all regions of Iran, providing a diverse and representative dataset that enhances the reliability and applicability of the findings. Additionally, the inclusion of detailed demographic and clinical variables allows for a comprehensive analysis of potential risk factors. However, several limitations warrant consideration. The retrospective design may affect the validity of the results, as it relies on the accuracy and completeness of previous medical records. Furthermore, the study was conducted in a single center, which may limit the generalizability of the findings to other healthcare settings. Unmeasured variables, such as preoperative nutritional status, may have influenced the outcomes but were not assessed due to incomplete documentation in the medical records. Multicenter studies are needed to validate these results and explore potential regional variations.
Further research should focus on identifying modifiable risk factors and developing targeted interventions to prevent and manage GI complications. Investigating the role of nutritional support and postoperative care protocols could provide valuable insights. Additionally, studies examining the long-term impact of GI complications on the growth and development of children with CHD are strongly recommended.
5.1. Conclusions
The results showed an overall incidence of 10.4%, with vomiting and chylothorax identified as the most common GI complications. Longer CPB duration was associated with a higher likelihood of GI complications. Additionally, GI complications were associated with prolonged ICU stays. Demographic variables such as age and gender were not significantly associated with GI complications. The findings emphasize the critical role of procedural factors, particularly the effects of prolonged CPB. Future studies are needed to identify additional risk factors for GI complications and to develop strategies for their prevention and management.