1. Background
In recent decades, significant advancements have been made in diagnostic and treatment tools for heart diseases in children (1). Advances in neonatal surgery, cardiac catheterization, anesthesia, intensive care, bypass systems, and mechanical devices have improved outcomes, particularly for critically ill patients (2). Although the incidence of congenital heart defects (CHD) is similar worldwide, the burden of these diseases is greater in countries with high fertility rates (3). Various scoring systems are used to categorize heart surgeries, with the risk adjustment for congenital heart surgery (RACHS-1) method being one of the most well-known. This system classifies patients into six groups based on the type of surgery and the patient’s age (4). The RACHS system was initially designed to predict mortality after cardiac surgery in children with CHD. However, its use has now broadened to assess postoperative complications, long-term outcomes, and to help healthcare providers make informed decisions about patient care and resource allocation (5). The use of cardiopulmonary bypass (CPB) during surgery triggers an inflammatory response and disrupts hemostasis (6). The neutrophil-to-lymphocyte ratio (NLR) has been recognized as an inflammatory and prognostic factor (6).
2. Objectives
This study aims to determine the prevalence and predisposing factors of pulmonary complications in surgical patients, as well as their relationship with the NLR. The study was conducted in the cardiac surgery intensive care unit at the Children's Medical Center Hospital (CMC) in Tehran, Iran, from October 2021 to October 2022.
3. Methods
This was a retrospective cohort study conducted at the CMC in Tehran, Iran. The study included patients aged 1 day to 18 years who underwent open-heart surgery between October 1, 2021, and October 1, 2022. All patients were transferred to the open-heart surgery intensive care unit (ICU-OH) following surgery. Patients who deceased during the study period were excluded from the analysis.
The sample size was calculated using the following formula for cohort studies: Z = 1.96 (corresponding to a 95% confidence level); d = Margin of error (0.05).
Considering potential dropouts and incomplete data, the final sample size was increased to 457 patients. A convenience sampling method was employed, where all eligible patients who underwent open-heart surgery during the study period were included.
The study was approved by the Ethics Committee of Tehran University of Medical Sciences (ethical code: IR.TUMS.CHMC.REC.1400.088). Informed consent was obtained from the parents or legal guardians of all participants.
All patients were transferred to the ICU-OH. Data was collected utilizing a structured checklist. The pulmonary complications monitored included pulmonary hemorrhage, pneumothorax, hemothorax, diaphragm paralysis, pulmonary edema, bronchomalacia, and chylothorax. Additionally, the RACHS-1 scoring system was employed to classify the patients. Preoperative and postoperative neutrophil and lymphocyte counts and the NLR were recorded, and its relation to the pulmonary complications was evaluated. In this study, patients who did not have pulmonary complications were included in the analysis, while those who had deceased were excluded.
Data were analyzed using SPSS version 28 (IBM Corp. Released 2021. IBM SPSS statistics for Mac, version 28.0. IBM Corp). Qualitative variables were expressed as percentages, while quantitative variables were reported as mean ± standard deviation (SD). For analytical comparisons and to ascertain the relationship between independent variables and the outcome variable, t-tests and chi-square tests were utilized, contingent upon the nature of the variables involved. In instances where data distribution deviated from normality, non-parametric equivalents such as Mann-Whitney U tests and Fisher’s exact tests were applied. A significance threshold was established at P < 0.05.
4. Results
A total of 457 patients were included in the study. The findings in Table 1 indicate the demographic and clinical characteristics of the patients. The average age of the patients was 25.84 months, with a SD of 36.9. The average weight of the patients was 10.48 kg, and the average length of hospital stay was 7.24 days. According to the RACHS-1, most patients were in risk categories 1 and 2. Ultimately, out of the total 457 patients, 433 (97%) survived and 14 (3%) deceased.
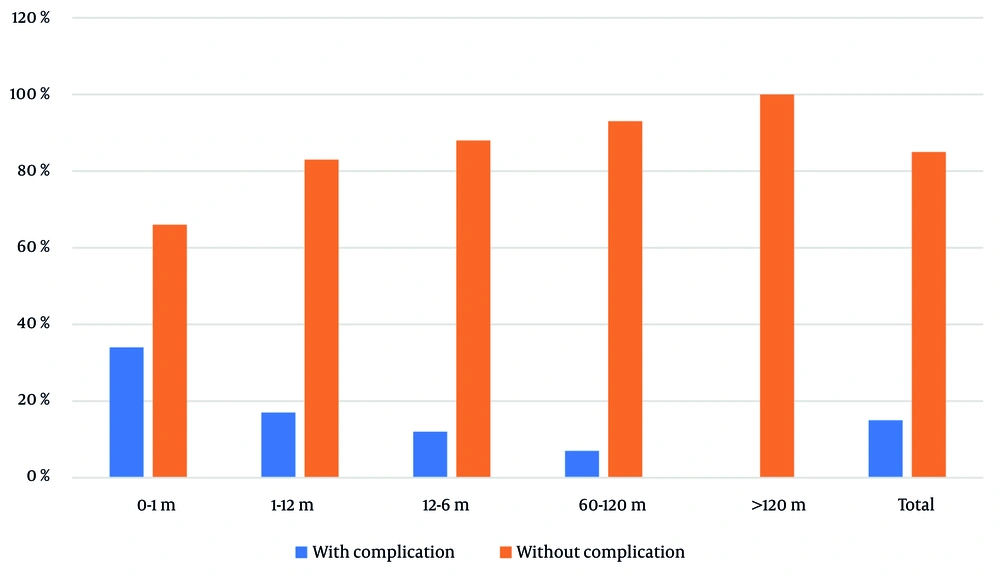
The results depicted in Figure 1 show that a total of 68 children (15%) suffered from pulmonary complications. The highest rate of pulmonary complications was observed in children less than one month old (18 patients, 34% of the total). The prevalence of complications across different age groups was statistically significant (P < 0.001).
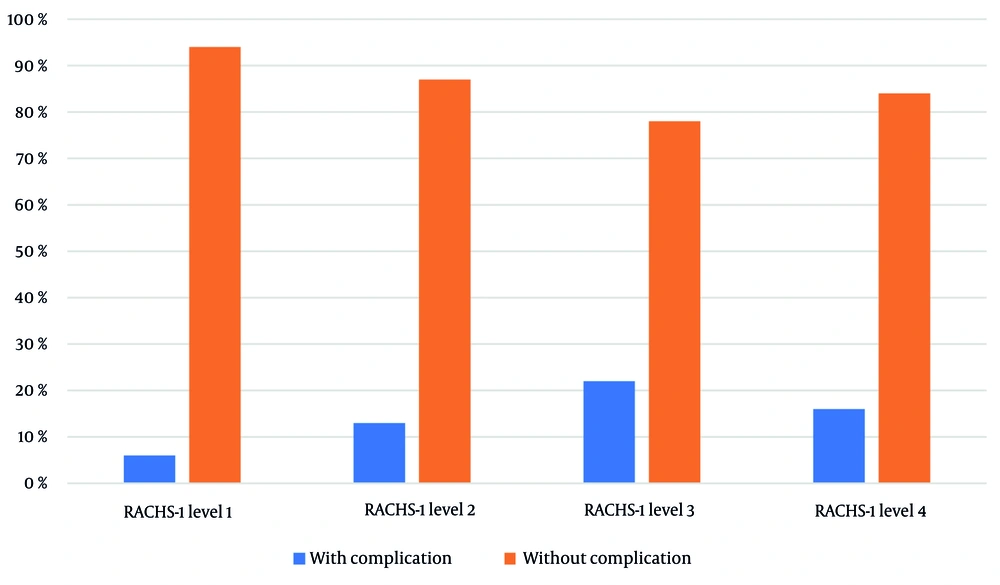
The frequency of pulmonary complications was 14% in boys and 16% in girls. Overall, the frequency of pulmonary complications did not show any significant difference between males and females (P = 0.847). Investigations regarding the risk of mortality (RACHS-1) show that pulmonary complications in patients who were in risk category 1 are 6%, while in risk category 4, they were 22%. The frequency of complications according to RACHS-1 was not statistically significant (P = 0.150) (Figure 2).
The data presented in Table 2 highlights several key findings comparing patients with and without pulmonary complications. While the CPB time (mean ± SD) shows a trend towards being longer in patients with complications (146 minutes versus 118 minutes), the difference is not statistically significant (P = 0.071). In contrast, the length of hospitalization is significantly greater in patients with complications (13 days compared to 6 days; P < 0.001), indicating that pulmonary complications lead to more severe health issues requiring extended recovery. Furthermore, the duration of mechanical ventilation is also significantly longer in those with complications (49 days versus 15 days; P < 0.001). Although white blood cell (WBC) counts before the operation do not show significant differences (9769 cells/mL in no complications versus 10874 cells/mL in complications; P = 0.294), the NLR before surgery is significantly higher in patients with complications (1.62 versus 1.08; P = 0.012), indicating a potentially heightened inflammatory state. The WBC counts on the first and second postoperative days do not demonstrate significant differences.
| Variables | Pulmonary Complication | P-Value | |
|---|---|---|---|
| Yes | No | ||
| CPB time (min) | 146 ± 64 | 118 ± 64 | 0.071 |
| Length of hospitalization (d) | 13 ± 10 | 6 ± 5 | < 0.001 |
| Duration of mechanical ventilation (h) | 49 ± 64 | 15 ± 17 | < 0.001 |
| WBC (number per milliliters) | 0.294 | ||
| Before the operation | 10874 ± 4100 | 9769 ± 3641 | |
| First day | 12007 ± 6463 | 12432 ± 5925 | |
| Second day | 13600 ± 5219 | 13564 ± 7221 | |
| NLR | 0.012 | ||
| Before the operation | 1.62 ± 2.09 | 1.08 ± 2.79 | |
| First day | 3.41 ± 2.8 | 3.53 ± 2.94 | |
| Second day | 6.1 ± 4.43 | 7.52 ± 5.7 | |
Review and Comparison of Paraclinical Findings of Patients by Pulmonary Complications a
Table 3 presents the distribution of frequency and prevalence of complications among hospitalized patients based on the RACHS-1 scoring system. The table shows that among patients in risk category four, 16% experienced pulmonary complications, while in risk category three, the prevalence of pulmonary complications increased to 22%. Patients in risk categories two and one showed lower instances of pulmonary complications at 13% and 10%, respectively.
| Two | One | Two | Three | Four |
|---|---|---|---|---|
| Pulmonary complications | 7 (10) | 31 (13) | 22 (22) | 5 (16) |
Table 4 investigated predictor variables and their association with the outcome. The CPB time (OR = 1.005, P = 0.008), length of hospitalization (OR = 1.147, P < 0.001), and duration of mechanical ventilation (OR = 1.029, P < 0.001) were identified as significant predictors, all associated with an increased risk. The WBC count before the operation (OR = 1.00, P = 0.028) also showed a significant association. However, the NLR at none of the measured time points (before the operation, first day, and second day) had a significant association with the outcome. The AUC values for length of hospitalization (0.79) and duration of mechanical ventilation (0.80) indicate relatively good accuracy of these variables in predicting the outcome. In contrast, other variables such as WBC on the first and second days and NLR at different time points had lower predictive accuracy (AUC close to 0.5).
| Predictor Variables | OR | P-Value | Lower CI | Upper CI | AUC |
|---|---|---|---|---|---|
| CPB time (min) | 1.005 | 0.008 | 1.001 | 1.009 | 0.57 |
| Length of hospitalization (d) | 1.147 | < 0.001 | 1.095 | 1.201 | 0.79 |
| Duration of mechanical ventilation (h) | 1.029 | < 0.001 | 1.02 | 1.038 | 0.80 |
| WBC (Number per milliliters) | |||||
| Before the operation | 1.00 | 0.028 | 1.00 | 1.00 | 0.57 |
| First day | 1.00 | 0.591 | 1.00 | 1.00 | 0.53 |
| Second day | 1.00 | 0.969 | 1.00 | 1.00 | 0.49 |
| NLR | |||||
| Before the operation | 1.049 | 0.219 | 0.972 | 1.133 | 0.58 |
| First day | 0.985 | 0.750 | 0.899 | 1.08 | 0.52 |
| Second day | 0.944 | 0.056 | 0.889 | 1.001 | 0.55 |
Estimation of Prediction of Pulmonary Complication by Potential Predictors
5. Discussion
Our study findings highlighted important aspects of pulmonary complications in pediatric patients undergoing cardiac surgery. The preoperative NLR was significantly higher in patients who developed complications (1.62 vs. 1.08; P = 0.012), suggesting that an elevated inflammatory state before surgery may predispose patients to adverse outcomes. This aligns with previous research which identified NLR as a prognostic marker for poor surgical outcomes, particularly when measured postoperatively (7). Our results extend this understanding by emphasizing the predictive value of preoperative NLR, which could serve as an early warning sign for clinicians to implement targeted interventions.
The study also revealed that pulmonary complications were most prevalent in infants under one month of age (34%), underscoring the vulnerability of this age group. This finding has significant clinical implications, as it suggests that neonates undergoing cardiac surgery require heightened monitoring and tailored respiratory support to mitigate risks. Furthermore, the duration of hospitalization and mechanical ventilation was significantly longer in patients with complications (13 days vs. 6 days and 49 hours vs. 15 hours, respectively; P < 0.001), reinforcing the need for strategies to reduce postoperative pulmonary complications and improve recovery times.
While the RACHS-1 scoring system did not show a statistically significant association with pulmonary complications in our study, this may reflect variations in surgical expertise or patient management rather than a limitation of the scoring system itself. For instance, patients in higher RACHS-1 categories (e.g., category 4) had a higher incidence of complications (22%), but this trend did not reach statistical significance (P = 0.150). This contrasts with some other studies which found a strong correlation between RACHS-1 scores and mortality (8). The discrepancy may be attributed to differences in surgical skill or institutional protocols, highlighting the importance of standardized practices and continuous training for surgical teams.
The role of CPB time in postoperative outcomes remains a critical area of investigation. Although our study did not find a statistically significant difference in CPB duration between patients with and without complications (146 minutes vs. 118 minutes; P = 0.071), the trend toward longer CPB times in complicated cases aligns with findings from other studies (6, 9). Prolonged CPB is known to exacerbate systemic inflammation and disrupt hemostasis, which may contribute to postoperative complications. Future research should explore strategies to minimize CPB duration and mitigate its inflammatory effects.
The clinical implications of our findings are twofold. First, preoperative NLR measurement could be integrated into risk assessment protocols to identify high-risk patients early. Second, targeted interventions, such as enhanced respiratory care and inflammatory modulation, could be prioritized for neonates and patients with elevated NLR to reduce complications and improve outcomes. These measures, combined with standardized surgical practices and continuous monitoring, could significantly enhance the quality of care for pediatric cardiac surgery patients.
Additionally, the findings reveal that longer CPB time, extended hospitalization, and prolonged mechanical ventilation are significant predictors of adverse outcomes, consistent with previous literature. For instance, studies have shown that prolonged mechanical ventilation and extended hospital stays are strongly associated with increased morbidity and mortality in children undergoing cardiac surgery, likely due to the heightened inflammatory response and physiological stress imposed by these factors (7). The WBC count before surgery was also found to be a significant predictor, which aligns with existing evidence suggesting that preoperative inflammation or infection can exacerbate postoperative complications (6, 10).
However, the lack of significant predictive value for WBC counts on the first and second postoperative days, as well as for NLR at any time point, contrasts with some studies that have highlighted NLR as a useful marker of systemic inflammation and predictor of complications in cardiac surgery patients (8, 11). This discrepancy may be attributed to differences in patient populations, surgical techniques, or timing of NLR measurements. For example, some studies have reported that NLR is more predictive when measured at later postoperative stages or in specific patient subgroups (9).
The AUC values for length of hospitalization (0.79) and duration of mechanical ventilation (0.80) indicate good predictive accuracy, reinforcing their utility as clinical indicators of pulmonary complications. However, the relatively low AUC values for WBC and NLR suggest that these markers may have limited standalone predictive value in this context. This finding underscores the importance of integrating multiple clinical and laboratory parameters to improve risk stratification and postoperative management.
In conclusion, while this study highlights the significance of CPB time, hospitalization duration, and mechanical ventilation as predictors of pulmonary complications, the role of NLR and WBC counts remains less clear and warrants further investigation. Future studies with larger sample sizes and standardized measurement protocols are needed to clarify the predictive utility of inflammatory markers like NLR in pediatric cardiac surgery patients.
5.1. Conclusions
The study found that the average age of patients was 25.84 months, with a balanced gender distribution (49% male, 51% female). The survival rate was high (97%), but 15% experienced pulmonary complications, particularly infants under one month. A significantly higher preoperative NLR in patients with complications suggests a pre-existing inflammatory state. These findings highlight the importance of preoperative NLR as a predictive marker and the need for targeted care in high-risk groups, such as neonates, to improve outcomes in pediatric cardiac surgery.
5.2. Limitations
This study has several limitations. Due to its retrospective design, there was limited control over confounding variables, which affects the ability to establish causality. The single-center nature of the study further limits the generalizability of the findings. Additionally, the small sample size for complications, involving only 68 patients, may reduce the statistical power of the study. The absence of long-term follow-up data precludes insights into long-term outcomes. Furthermore, the incomplete analysis of confounding factors, such as comorbidities and surgical techniques, may have impacted the comprehensiveness of the findings. Technical issues also restricted access to certain data, preventing the performance of regression analyses and receiver operating characteristic (ROC) curve analyses.
5.3. Recommendations
Future studies should consider adopting a prospective design and involve multi-center collaboration to enhance generalizability and increase sample size. Incorporating long-term follow-up, subgroup analysis, dynamic NLR monitoring, additional biomarkers such as C-reactive protein (CRP), and standardized NLR measurement methods would provide stronger evidence and deeper insights.