1. Introduction
Schwannoma are uncommon benign encapsulated tumors that contain Schwann cells of the nerve sheath; these neoplasms are slow-growing. A total of 25% of schwannomas are located in the head and neck region, and 1% of them are intraoral (1). Schwan cells develop from the neural crest that provide myelin sheath for axons of the peripheral nervous system (2). In the oral cavity, the most common site of involvement is the tongue, followed by the palate, buccal mucosa, lips, the vestibular mucosa, and gingiva (3). It has been reported that schwannoma is more common in adults; the pick of incidence of the lesion is between the ages of 10 to 40 years. The most common age of incidence of the tongue’s schwannoma is in the third decade of life. There is no gender prediction for schwannoma (4).
Clinically, schwannoma presents as a painless, smooth-surfaced mass that its overlying epithelium is intact. Schwannoma is usually solitary and multiple schwannomas are associated with neurofibromatosis (5). Differential diagnosis of intraoral schwannoma includes mucocele, eosinophilic granuloma, epidermoid and dermoid cyst, granular cell tumor, leiomyoma, lipoma, and benign salivary gland tumors (6). Histologically, schwannoma is present in two distinct types: Antoni A type and Antoni B type. Antoni A presents as fibroblast-like cells that arrange in a parallel design and accompany with Verocay bodies. Antoni B presents as a less cellular mass. Microvacuolation of the intercellular substance is obvious in this type. Staining for S-100 protein is positive in most of the tumor cells of schwannoma. The intensity of S-100 protein is much higher in Antoni A tissues (5).
Clinically, there are two forms of intraoral schwannoma: encapsulated and pediculated. The most frequent form is encapsulated in which the tumor is surrounded with dense fibrous connective tissue (7). Difference between pediculated schwannoma and other peripheral nervous system tumors is that although both of them originate from Schwann cells, but in schwannoma, peripheral nerve growth is mingled with Schwann cells, which result in tumor penetration into the surrounding tissues, and therefore, complete resection of the tumor will be difficult. Some literature claim that schwannoma is more common between the 4th and 6th decade of life, however, the most common age of oral involvement by schwannoma are the 2nd and 3rd decades of life, thus, schwannoma in childhood isn’t common (8).
2. Case Presentation
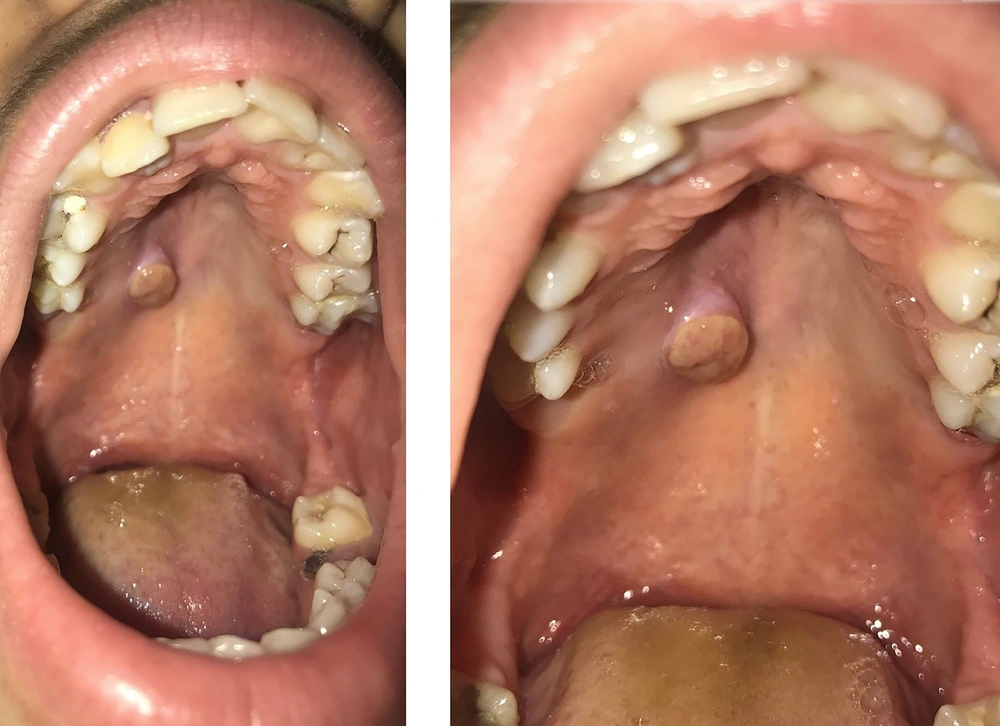
A 13 year old boy was referred to the oral medicine department of Tehran University of Medical Sciences. The patient’s chief complaint was palatal swelling since four months ago without any pain. Intraoral examination revealed a well-demarcated exophytic mass with a yellowish surface color, with a 0.6 ×0.5 cm diameter on the right side of the hard palate. No other lesions were seen in the other sites of the oral cavity. There was no lymph node enlargement in the neck (Figure 1).
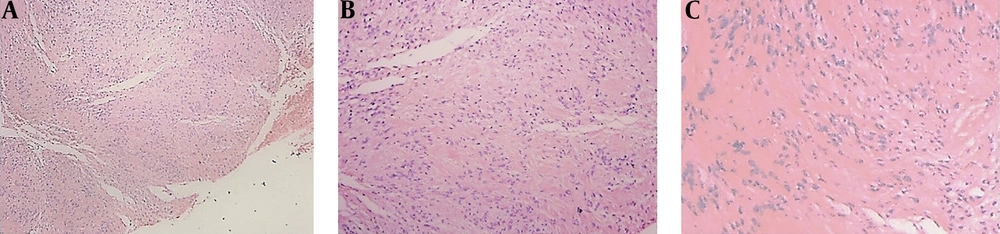
The patient’s medical history was unremarkable. In regards to the benign nature of the lesion and no remarkable medical history, an incisional biopsy of the lesion was performed. Histological examination of the surgical specimen revealed tumoral tissue composed of spindle cells arranged in fascicles and Antoni A and Antoni B like pattern. Immunohistochemistry showed positive staining for S-100 protein that proves the tumor origin. In the postoperative period, the patient has been followed for one year and there has been no evidence of recurrence. Histopathologic feature of the lesion are shown in Figure 2.
3. Discussion
Based on our knowledge, the prevalence of schwannoma in the hard palate, in a very young boy, is extremely rare, which is due to the fact that intraoral schwannomas tend to appear more often in adults. Lollar et al. reported a case of schwannoma in the hard palate in a 33-year-old male (2). Amir et al. reported a case of neurinoma in the entire surface of the hard palate in a 40 year old man, which caused dysphagia and garbled speech (9). The clinical sign of palatal schwannoma is a painless exophytic mass. Differential diagnosis of palatal schwannoma includes salivary gland tumors, mucocele, fibroma, traumatic neuroma, granular cell tumor, neurofibroma, and malignant lesions such as sarcoma.
Regarding the wide differential diagnosis and nonspecific clinical presentation, definitive diagnosis is made by histopathologic and immunohistochemically evaluation. As mentioned earlier, histologic appearance of schwannoma consists of two distinct components: Antoni A and Antoni B tissues. Antoni A tissue consist of aligned spindle cells forming a typical palisade, between the fibrils, there are small eosinophilic masses called Verocay body. Antoni B tissue, which is predominated in our case consists of smaller number of spindle cells which randomly scattered in a myxoid matrix. Immunohistochemical examination help to distinguish schwannoma from other neurogenic lesions. Reaction to S100 is seen in schwannoma and palisaded encapsulated neuroma. Reaction to CD57 is observed in a traumatic neuroma. The treatment of choice of schwannoma is complete excision. Our case was an encapsulated form, which its surgery was easy and its recurrence rate is very low. The prognosis is very good and the malignant transformation of the lesion is very rare. The most important point of this case is occurrence of a slow-growing schwannoma in the hard palate of a very young patient. Presence of an intraoral neural tumor in a young patient is very rare. Thus, considering neural tumors in the differential diagnosis of painless nodules in the oral cavity is mandatory.