1. Background
Understanding the epidemiological characteristics of salivary lesions helps differentiate them from other oral lesions (1). Salivary gland lesions are a heterogeneous and rare group of head and neck lesions with a wide variety of clinical manifestations and are divided into two groups: Neoplastic lesions and non-neoplastic lesions (1, 2). Correct diagnosis and timely treatment of patients with salivary neoplastic lesions, which comprise about 3 - 10% of cervical cancers, are very important to improve the prognosis of these lesions. However, a number of non-neoplastic inflammatory and reactive salivary gland lesions may mimic the clinical appearance of neoplastic lesions. For this reason, ultrasound, magnetic resonance imaging (MRI), three-dimensional cone beam CT (CBCT), and sometimes biopsy are used during the diagnosis process of these lesions (2). According to studies, the prevalence of non-neoplastic salivary lesions ranges from 21.3% to 66.3% of all salivary lesions, with mucocele and sialadenitis reported as the most common ones (1). In some geographical areas, inflammatory lesions and connective tissue diseases, including rheumatoid arthritis, which are associated with salivary gland lesions, are more common (3, 4).
Most past epidemiological studies in the field of salivary gland lesions (especially in Iran) have focused on prevalence and have often selectively studied salivary neoplastic diseases, mainly malignant lesions, while the overall incidence of salivary gland lesions has been less studied (1, 2, 5). Additionally, it has been reported that the age and geographical region of the studied population affect the final result of investigating the incidence of salivary gland tumors (2).
2. Objectives
The present study was conducted with the aim of comprehensively investigating the occurrence of various types of salivary gland lesions during a 5-year period, including non-neoplastic lesions and benign and malignant neoplasms in Rasht, Iran.
3. Methods
3.1. Study Population and Methodology
To extract the data required for this descriptive-analytical retrospective study, all pathobiology laboratories focused on oral diseases in Rasht city were consulted, and the study method and objectives were explained to them. By accessing the archives of these laboratories, records with histopathological diagnoses of salivary gland lesions based on standard diagnostic criteria and the approval of several oral, maxillofacial, and facial pathology specialists working in those laboratories were collected, totaling 273 cases from 2016 to 2021. Twelve cases were excluded from the study due to information deficiencies, and 261 cases were included in the study. The required information, including the patient's age, sex, lesion location, and histopathological diagnosis, was extracted and recorded from the patient's records.
In order to analyze the data, salivary gland lesions were divided into two groups according to the WHO classification: Neoplastic lesions, including malignant and benign salivary gland tumors, and non-neoplastic lesions, including sialadenitis, inflammatory lesions, granulomatosis, mucocele, Sjogren's syndrome, sialolithiasis, and foreign body reactions (1).
3.2. Ethical Considerations
All information extracted from the records (names, demographic characteristics, and lesion diagnosis of the patients) remained confidential, and the research results were published in general and in the form of study groups. If necessary, the individual results were presented without mentioning the patients' names and details. The present research was approved by the Ethics Committee of the Research of the Faculty of Guilan Medical Sciences with the ethics code IR.GUMS.REC.1400.339.
3.3. Calculating the Crude Rate
To report the crude rate in this study, the cumulative incidence was calculated as the number of new events or cases of disease divided by the total number of individuals in the population at risk for a specific time interval.
3.4. Statistical Analysis
Before statistical analysis, all data were coded, anonymously registered, and analyzed using SPSS version 26 software at a significance level of less than 0.05 and in the form of descriptive statistical indices. Frequency and percentage were used to describe qualitative data, and mean and standard deviation were used for quantitative data. In this study, data were analyzed by Analysis of Variance (ANOVA) and Pearson chi-square tests for quantitative data and Fisher's exact test for qualitative data.
4. Results
From the total of 261 cases examined in the study, 136 were men (52.1%) and 125 were women (47.9%), with an overall average age of 49.89 ± 16.01 years. The frequency and incidence of salivary gland lesions were generally higher in men than in women. The frequency and incidence of salivary gland lesions had a significant relationship with sex (P = 0.015); for non-neoplastic and malignant lesions, the highest frequency and incidence were in women, and for benign tumors, the highest frequency and incidence were in men.
The highest frequency of salivary gland lesions was related to ages 50 - 60 years (24.5%), 40 - 50 years (20.3%), and 60 - 70 years (20.3%). Also, the highest rates of non-neoplastic salivary gland lesions, benign tumors, and malignant tumors per 100,000 people were related to the ages of 40 - 50 years, 50 - 60 years, and 30 - 40 years, respectively. Although the correlation between the types of salivary lesions (neoplastic and non-neoplastic) and age was not significant (P = 0.478).
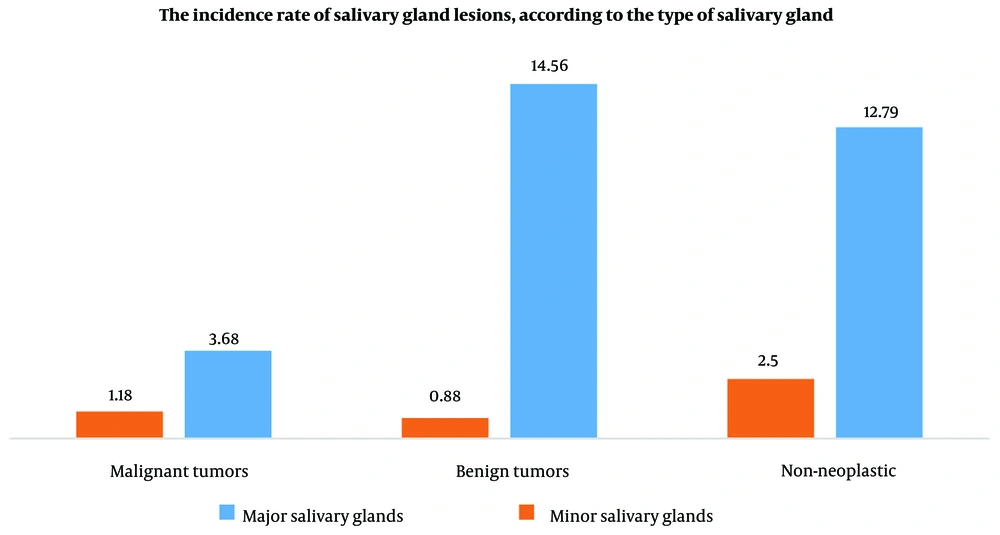
The frequency of neoplastic lesions (about 52.8%) was higher than that of non-neoplastic lesions, with benign tumors having the highest frequency of 40.2%. The most common lesion among non-neoplastic salivary gland lesions was inflammatory lesion in 35 cases (33.7%), among benign neoplastic lesions was pleomorphic adenoma in 73 cases (69.5%), and among malignant neoplastic lesions was adenoid cystic carcinoma in 10 cases (30.3%) (Table 1). The crude rate of salivary gland lesions from 2016 to 2021 included benign tumors (15.44 people), non-neoplastic salivary lesions (15.29 people), and malignant tumors (4.85 people) per 100,000 individuals.
| Group and Lesion | Number | Percentage (of Each Group | Total Number (%) of Total Lesions |
|---|---|---|---|
| Non-neoplastic lesions | 104 (39.8) | ||
| Inflammatory lesion | 35 | 33.7 | |
| Sialadenitis | 25 | 24 | |
| Sialolithiasis | 21 | 20.2 | |
| Mucocele | 9 | 8.7 | |
| Granulomatous lesions | 6 | 5.8 | |
| Sjogren's syndrome | 5 | 4.8 | |
| Reaction to a foreign body | 2 | 1.9 | |
| Unknown | 1 | 1 | |
| Benign tumors | 105 (40.2) | ||
| Pleomorphic adenoma | 73 | 69.5 | |
| Warthin tumor | 27 | 25.7 | |
| Oncocytoma | 2 | 1.9 | |
| Sialolipoma | 1 | 1 | |
| Unknown | 2 | 1.9 | |
| Malignant tumors | 33 (12.6) | ||
| Adenoid cystic carcinoma | 10 | 30.3 | |
| Mucoepidermoid carcinoma | 9 | 27.3 | |
| Acinic cell carcinoma | 3 | 9.1 | |
| Salivary duct carcinoma | 2 | 6.2 | |
| Adenocarcinoma | 1 | 3 | |
| Clear cell carcinoma | 1 | 3 | |
| SCC | 1 | 3 | |
| Malignant lymphoma | 1 | 3 | |
| Unknown | 5 | 15.2 | |
| Re-biopsy required | 19 (7.3) | ||
| Total | 261 (100) |
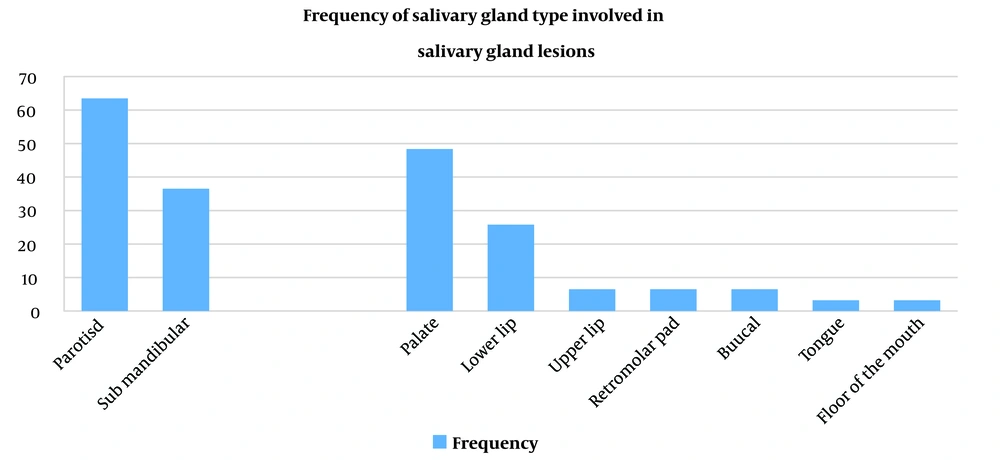
The frequency and incidence of salivary gland lesions in the main salivary glands were higher than those in the secondary salivary glands (Figure 1), and among the main salivary glands, the parotid gland had the highest frequency of incidence (63.5%). Among the minor salivary glands, the palate had the highest frequency of incidence (48.4%) (Figure 2). The relationship between the types of salivary gland lesions and the location of salivary gland involvement was significant. For minor salivary glands, the highest frequency and incidence of non-neoplastic lesions were related to the lower lobe, and for benign and malignant tumors, the highest frequency and incidence were related to the palate (P = 0.001). For the main salivary glands, the highest frequency and incidence of non-neoplastic lesions were related to the submandibular gland, and for benign and malignant tumors, the highest frequency and incidence were related to the parotid gland (P < 0.001) (Table 2).
| Type of Salivary Gland, Location and Lesion | Frequency | Incidence per 100,000 People | P-Value |
|---|---|---|---|
| Major Salivary Gland | < 0.001 b | ||
| Parotid | |||
| Non-neoplastic | 33 | 4.85 | |
| Benign tumor | 85 | 12.50 | |
| Malignant tumor | 18 | 2.65 | |
| Submandibular | |||
| Non-neoplastic | 54 | 7.94 | |
| Benign tumor | 14 | 2.05 | |
| Malignant tumor | 7 | 1.03 | |
| Minor Salivary Glands | 0.001 c | ||
| Floor of mouth | |||
| Non-neoplastic | 1 | 0.15 | |
| Palate | |||
| Non-neoplastic | 2 | 0.29 | |
| Benign tumor | 5 | 0.73 | |
| Malignant tumor | 8 | 1.18 | |
| Tongue | |||
| Non-neoplastic | 1 | 0.15 | |
| Upper lobe | |||
| Non-neoplastic | 2 | 0.29 | |
| Lower lobe | |||
| Non-neoplastic | 8 | 1.18 | |
| Retromolar pad | 2 | 0.29 | |
| Non-neoplastic | |||
| Buccal mucosa | |||
| Non-neoplastic | 1 | 0.15 | |
| Benign tumor | 1 | 0.15 | |
a Average population size: 679995.
b Pearson chi-square test.
c Fisher's exact test.
The types of non-neoplastic lesions and benign and malignant salivary gland tumors are shown in Table 3, according to the lesion type, frequency according to gender, average age, most common gland involved, most common location of sub-salivary gland involvement, and the crude rate per 100,000 individuals.
| Group and Type of Lesion | Male-Prevalence | Female-Prevalence | Most Commonly Involved Gland | The Most Common Site of Involvement of the Parathyroid Glands | Incidence per 100,000 People |
|---|---|---|---|---|---|
| Non-neoplastic | |||||
| Inflammatory lesions | 16 (45.7) | 19 (54.3) | Parotid (60) | - | 5.14 |
| Sialadenitis | 16 (64) | 9 (36) | Submandibular (72) | Palate | 3.67 |
| Sialolithiasis | 14 (66) | 7 (33) | Submandibular (95) | - | 3.08 |
| Mucocele | 2 (33) | 7 (77) | Minor glans (100) | Lower lip | 1.32 |
| Granulomatosis | 2 (33) | 4 (66) | Parotid (66) | - | 0.88 |
| Sjogren's syndrome | - | 5 (100) | Minor glands (80) | Lower lip | 0.73 |
| Reaction to a foreign body | 1 (50) | 1 (50) | Parotid (100) | - | 0.29 |
| Benign tumors | |||||
| Pleomorphic adenoma | 37 (50.7) | 36 (49.3) | Parotid (79) | Palate | 10.73 |
| Warthin tumor | 27 (100) | - | Parotid (81) | - | 3.97 |
| Oncocytoma | 1 (50) | 1 (50) | Parotid (100) | - | 0.29 |
| Sialolipoma | - | 1 (100) | Parotid (100) | - | 0.14 |
| Unknown | 1 (50) | 1 (50) | Parotid (100) | - | 0.29 |
| Malignant tumors | |||||
| Mucoepidermoid carcinoma | 4 (44) | 5 (55) | Parotid and minor glans | Palate | 1.32 |
| Adenoid cystic carcinoma | 1 (10) | 9 (90) | Parotid (70) | Palate | 1.47 |
| Acinic tubercle carcinoma | 1 (33) | 2 (66) | Parotid (100) | - | 0.44 |
| Salivary duct carcinoma | 2 (100) | - | Submandibular (100) | - | 0.29 |
| Adenocarcinoma | - | 1 (100) | Minor glans (100) | Palate | 0.14 |
| Clear cell carcinoma | - | 1 (100) | Minor glands (100) | Palate | 0.14 |
| SCC | - | 1 (100) | Submandibular (100) | - | 0.14 |
| Malignant lymphoma | 1 (100) | - | Parotid (100) | - | 0.14 |
| Unknown | 3 (60) | 2 (40) | Parotid (60) | - |
a Values are presented as No. (%).
5. Discussion
The present retrospective study considered 273 salivary gland lesions from 2016 to 2021, which were archived in all pathobiology laboratories focusing on oral diseases in Rasht, Iran. Given that the prevalence of a disease is influenced by factors such as the number of new disease cases, recovery speed, and the number of deaths due to the disease (6), this study examined the incidence of salivary gland lesions sent to Rasht pathology centers from 2016 to 2021.
In the present study, 261 cases, including 136 men (52.1%) and 125 women (46.4%), with an overall average age of 49.89 ± 16.01 years, were examined. According to the results, the highest frequency of lesions was related to the sixth decade of life (24.5%). McKenzie et al. also reported the highest frequency of salivary gland lesions in the sixth decade (7). This study revealed that although the average age of people with non-neoplastic lesions (50.15 ± 54.59 years) was higher than that of malignant tumors (49.18 ± 51.46 years), and the average age of people with malignant tumors was slightly higher than that of benign tumors (47.15 ± 88.14 years), the types of salivary lesions (neoplastic and non-neoplastic) had no significant relationship with age. This result contrasts with the study by Movahedian et al., who reported a significant correlation between benign and malignant salivary tumors with age (8). Given that certain habits and long exposure to alcohol or tobacco have been reported as causes of most oral cancers, including salivary gland neoplasms, in older people (1), the differences in the obtained results can be attributed to differences in the amount of alcohol consumption or smoking in the studied populations.
As the results indicated, the frequency and incidence of salivary gland lesions are generally higher in men than in women, and there is a significant relationship between the types of examined salivary gland lesions and gender (including non-neoplastic lesions, benign and malignant salivary tumors) (P = 0.015). The highest frequency and incidence of non-neoplastic lesions and malignant tumors were observed in women, while benign salivary tumors were more common in men. This higher frequency of benign tumors and malignant tumors in women compared to men aligns with the results of past studies such as those by McKenzie et al., Cunha et al., and Baghaei et al. (7, 9, 10). Meanwhile, during an epidemiological study investigating the prevalence of salivary gland tumors in the population of Tehran between 2005 and 2016, Shamloo et al. concluded that benign and malignant tumors were slightly more prevalent in men than in women (11). The difference in the above results may be related to racial and geographic factors and possibly differences in individual habits such as diet, oral hygiene, chewing gum, drug use, smoking, etc., although no explanation has been provided for the difference between the frequency in men and women in different studies.
According to the findings of the present study, the highest frequency of salivary gland lesions was observed in the parotid gland (63.5%), followed by the minor salivary glands of the palate (48.4%). The highest frequency and incidence of non-neoplastic lesions were located in the lower lobe and submandibular salivary glands, respectively. For benign and malignant tumors, the highest frequency and incidence were in the minor and main salivary glands, including the palate and parotid glands, respectively. Similar to the results of our study, most previous studies reported the most common site of involvement for salivary gland tumors, especially the benign type, in the parotid gland, and the most common site of involvement of the minor salivary glands as the palate (1, 8, 11, 12). However, in a study by Cunha et al., the most common site of involvement in salivary gland tumors was the minor salivary glands of the palate, followed by the parotid, lips, and buccal mucosa, respectively (9).
In the study by Baghaei et al., the highest frequency of non-neoplastic lesions among the main salivary glands was observed in the submandibular gland, and among the secondary glands, it was observed in the lower lobe, consistent with our study (10). The high frequency in the submandibular gland is likely due to the higher prevalence of inflammatory lesions and sialolithiasis in the duct of the submandibular gland. Lower lobe involvement seems to be due to the high prevalence of mucoceles (caused by trauma) in the lower lobe (10). In the study by Baghaei et al., sialolithiasis had the highest frequency among non-neoplastic salivary gland lesions (10), while in the present study, inflammatory lesions and sialadenitis had the highest frequency.
The incidence of neoplastic lesions versus non-neoplastic lesions has been variably reported in different studies (1, 7, 11, 13). In the present study, the highest frequency and incidence were associated with benign salivary gland tumors (40.8%), followed by non-neoplastic lesions (39.8%), and finally malignant salivary tumors (12.6%). This finding is consistent with the findings of most epidemiological studies conducted in Iran and other countries in terms of the prevalence of previously biopsied samples (7, 9, 11, 12). In a study by Baghaei et al., who investigated the frequency of salivary gland lesions in Hamedan from 2006 to 2017, the frequency of non-neoplastic lesions was 65%, and the frequency of benign and malignant neoplastic lesions was 24.3% and 10.3%, respectively, which differs from the findings of the present study (10). Similarly, Saravani et al., who investigated the frequency of salivary lesions in Isfahan patients from 1998 to 2003, reported the prevalence of non-neoplastic lesions to be 46% and benign and malignant salivary tumors to be 32% and 20%, respectively (1), which is inconsistent with the results of the present study. These differences in results can be due to the sources of the referred cases. Given that age and sex can affect the incidence of certain salivary gland lesions (such as Sjögren's syndrome), the discrepancy in the results may relate to different sample sizes and environmental factors in the two studies. Additionally, clinical diagnosis and treatment of many non-neoplastic lesions of the salivary glands often rely on clinical signs and symptoms or radiographic images (10). Therefore, the need for biopsy may be lower, and histopathological samples may not be included in the studies, leading to potential errors in examining the frequency of lesions in previously biopsied samples.
According to the results of the present study, pleomorphic adenoma and adenoid cystic carcinoma are the most common benign and malignant tumors, respectively. Most previous epidemiological studies have reported pleomorphic adenoma as the most common benign salivary tumor (8, 9, 11). However, the most common malignant salivary tumor has been reported as adenoid cystic carcinoma in some past studies (11, 14-16) and mucoepidermoid carcinoma in others (1, 8, 9, 17). The second most common benign tumor of the salivary glands has been reported similarly in most previous studies, consistent with the results of our study (8, 17). Significant differences in the incidence of salivary gland tumors have been reported based on age, sex, and lesion location.
Also, according to the results of the present study, the parotid gland (60 - 100%) is the most common site of benign tumors in general, and the minor salivary glands of the palate are the most common sites of malignant tumors, consistent with the results of Alsanie et al.'s study (17).
5.1. Strengths and Limitations
The most important strength of the present study is the determination of the incidence along with the prevalence of all salivary lesions because most previous epidemiological studies have only considered the prevalence rate of salivary gland lesions without determining their incidence rate and often only studied salivary gland tumors.
One of the limitations of this study is the lack of access to information such as occupation, social and economic status, personal habits, and medical history, which can be effective factors in the prevalence and occurrence of salivary gland diseases. The retrospective nature of the current study is another limitation.
5.2. Conclusions
Based on the results of the present study, the incidence of salivary glands' neoplastic lesions has increased in the last 5 years. Pleomorphic adenoma and adenoid cystic carcinoma were the most common benign and malignant tumors reported in this study, respectively. These findings highlight the need for further studies on the causes of salivary gland neoplasms.