1. Background
Despite widespread efforts to control infectious diseases, human immunodeficiency virus (HIV) and Acquired Immune Deficiency Syndrome (AIDS) have created major public health problems worldwide (1). Approximately 75 million people have been infected with HIV since the beginning of the AIDS epidemic, and 36 million have died from this disease. It is estimated that 40.4 million people were living with HIV by the end of 2022, with 1.3 million new HIV-infected patients identified in the same year (2). Fortunately, the number of AIDS-related deaths has dropped from 2.3 million in 2005 to 630,000 in 2022 (2). The advent of anti-AIDS drugs appears to have contributed to a decrease in death rates related to AIDS. Effective treatment with anti-AIDS drugs has increased the survival of patients following infection with this virus from 10-12 years to 25 years (3, 4). Fortunately, AIDS is now regarded as a controllable disease (5, 6).
From a public health perspective, understanding the period required for an HIV-positive person to progress to AIDS and their survival time (with or without HIV treatment) is of high importance. Therefore, the use of cART drugs for the treatment of AIDS has caused significant changes and delayed the progression of the disease (7). However, the efficiency of cART drugs varies in different countries due to the burden of underlying diseases like tuberculosis, virus types, and genetic background. Despite the fact that a majority of studies have indicated that anti-AIDS treatment has significantly decreased the rate of disease progression from HIV to AIDS, there is heterogeneity in the survival rates of patients infected with HIV (8-11).
Despite the decline observed in AIDS mortality in recent years, identifying the predictor factors affecting the long-term survival of HIV-positive patients, especially in developing countries, remains critically important. Few studies have investigated the survival of HIV-infected individuals in Iran. Without reliable information on the survival rates of HIV-infected people, it is challenging to design intervention approaches to increase the life expectancy of these patients.
2. Objectives
The present retrospective cohort study was performed to evaluate the role of possible risk factors, especially the use of antiviral drugs and co-infection of AIDS patients with other diseases, in the progression of the disease from diagnosis to death.
3. Methods
The present study was a retrospective cohort study that used information from 201 HIV-positive or AIDS patients in Qazvin province during 1991 - 2021. The study population included all patients referred to the Behavioral Diseases Counseling Center in Qazvin Province. This center provides services such as reducing harm to drug abusers, treating sexually transmitted diseases, and treating, caring for, and supporting HIV-positive people as well as AIDS patients. The variables recorded by HIV-positive people or AIDS patients at the Behavioral Diseases Counseling Center included age, sex, occupation, marital status, education, mode of transmission (mother-to-child, reception of blood and its products, addiction, unspecified sexual behaviors), date of diagnosis and death, treatment with antiretroviral drugs (ART), history of tuberculosis, Hepatitis B, Hepatitis C, time from diagnosis to the onset of AIDS, and time from diagnosis to death.
The criteria for this classification of HIV stages are as follows:
-Stage I: Asymptomatic HIV infection with a CD4 cell count greater than 500 cells/µL. It may also include enlarged lymph nodes.
-Stage II: Mild symptoms, which may include mild mucosal changes and recurrent upper respiratory tract infections, with a CD4 cell count of less than 500 cells/µL.
-Stage III: Advanced symptoms, which may include chronic, unusual diarrhea for more than a month, along with severe bacterial infections, including pulmonary tuberculosis, and a CD4 cell count of less than 350 cells/µL.
-Stage IV or AIDS: Severe symptoms including toxoplasmosis of the brain, candidiasis of the esophagus, trachea, bronchus, or lung, and Kaposi's sarcoma. The number of CD4 cells reaches less than 200 cells/µL.
According to the standards of the Ministry of Health of Iran, an HIV-positive person is identified by the presence of the IgM antibody through 3rd and 4th generation ELISA tests, and confirmed by the detection of the IgG antibody via a western blot test (12). Advanced HIV infection is diagnosed based on clinical and/or immunological (CD4) criteria among people with confirmed HIV infection: CD4 count less than 350 per mm3 of blood in an HIV-infected adult or child (13). In this study, a person who had progressed to clinical stages III and IV with CD4 T-cell levels > 350 mm³ was considered an AIDS patient.
In this study, we examined two outcomes: AIDS and death. The first outcome was estimating the period from HIV infection to the onset of AIDS, and the second was measuring the time from HIV infection to death. Patients whose disease outcome was unknown due to reasons such as death from other events were considered as "censored." Although cART drugs were used to suppress the spread of HIV and prevent the disease from progressing to AIDS, the effect of treatment with these drugs on patient survival was investigated. The impact of co-infection with tuberculosis, history of Hepatitis B and C, and the effects of various factors such as sex, age, marital status, HIV transmission route, survival time in the two stages of AIDS and death were also explored.
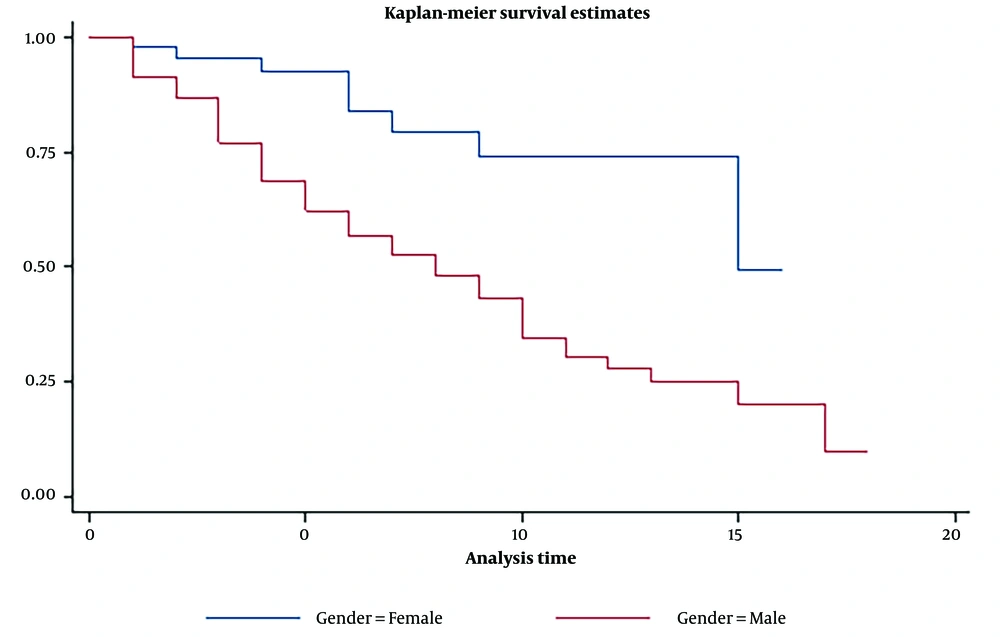
Additionally, the cumulative survival of HIV progression to death was analyzed by sex using the Kaplan-Meier approach, with a graph available. Cumulative rates of death and AIDS were tested in all subgroups using the log-rank test. In total, we calculated the adjusted and crude risk ratios of disease progression to death using the Cox proportional hazard model. To evaluate the appropriateness of the risk over time, we used the log-rank test, which assumed that the risk was constant over time in this model based on P = 0.550. To calculate the hazard ratio with higher precision, we investigated the interaction between sex and the use of anti-AIDS drugs (ART), and the bilateral interaction between variables in the model was controlled for using the forward method (P = 0.357). Data analysis was performed at a significance level of 5% using STATA 14.2 statistical software.
4. Results
Of the 201 HIV-positive patients, 150 (74.6%) were male. The mean age of individuals at the time of diagnosis was 34.9 ± 11.81 years, with an age range of 2 - 76 years. According to these findings, the prevalence of HIV/AIDS was higher in men, the age group 25 - 34 years, married people, and injection drug users. Co-occurrence of tuberculosis and Hepatitis B was rare. Demographic characteristics and other clinical information of the subjects are shown in Table 1. Regardless of the clinical signs and symptoms, out of the 31 AIDS patients diagnosed in stages III and IV (AIDS), 23 had a CD4 T-cell level > 250 mm3. The ratios of people who progressed from HIV to AIDS in terms of sex (P < 0.001), route of transmission (P < 0.000), and co-occurrence of Hepatitis C (P < 0.000) were significantly different.
| Variables | Positive HIV | ADIS | Censored | Total | P-Value |
|---|---|---|---|---|---|
| Gender | 0.001 | ||||
| Female | 39 (76.47) | 9 (17.65) | 3 (5.88) | 51 | |
| Male | 70 (46.47) | 40 (26.67) | 40 (26.67) | 150 | |
| Age group | 0.637 | ||||
| 0 - 14 | 2 (40.00) | 0 (0.00) | 3 (60.00) | 5 | |
| 15 - 24 | 14 (58.33) | 5 (20.83) | 5 (20.83) | 24 | |
| 25 - 34 | 43 (51.81) | 20 (24.10) | 20 (24.10) | 83 | |
| 35 - 44 | 30 (57.69) | 14 (26.92) | 8 (15.38) | 52 | |
| 45 - 54 | 15 (55.56) | 8 (29.63) | 4 (14.81) | 27 | |
| ≥ 55 | 5 (50.00) | 2 (20.00) | 3 (30.00) | 10 | |
| Marital status | 0.168 | ||||
| Single | 29 (45.31) | 19 (29.69) | 16 (25.00) | 64 | |
| Married | 50 (53.76) | 22 (23.66) | 21 (22.58) | 93 | |
| Widow | 16 (59.26) | 5 (18.52) | 6 (22.22) | 27 | |
| Divorced | 14 (82.35) | 3 (17.65) | 0 (0.00) | 17 | |
| Ways of transmission | 0.001 | ||||
| Sexually transmission n | 49 (75.38) | 12 (18.46) | 4 (6.15) | 65 | |
| Mother to child | 2 (66.67) | 0 (0.00) | 1 (33.33) | 3 | |
| Blood productions | 0 (0.00) | 0 (0.00) | 2 (100.00) | 2 | |
| Injectable addiction | 58 (44.27) | 37 (28.24) | 36 (27.48) | 131 | |
| Co-occurrence with tuberculosis | 0.120 | ||||
| Negative Tuberculosis | 107 (55.15) | 45 (23.20) | 42 (21.65) | 194 | |
| Positive Tuberculosis | 2 (28.57) | 4 (57.14) | 1 (14.29) | 7 | |
| Morbid with Hepatitis B | 0.083 | ||||
| No | 106 (55.21) | 44 (22.92) | 42 (21.88) | 192 | |
| Yes | 3 (33.33) | 5 (55.56) | 1 (11.11) | 9 | |
| Morbid with Hepatitis C | 0.001 | ||||
| No | 48 (75.00) | 12 (18.33) | 5 (67.76) | 65 | |
| Yes | 61 (44.85) | 37 (27.21) | 38 (27.94) | 136 | |
| Total | 109 (54.23) | 49 (24.38) | 43 (21.39) |
Distribution of Demographic Features of HIV / AIDS Positive People in the First Care in Qazvin Province Between 1991 and 2021 a
The effects of prognostic factors on the hazard ratio of progression from HIV to death are shown in Table 2. Both the unadjusted and adjusted hazard ratios are shown for comparison. No two-way interactions were seen between the variables in the model. The risk of progression to death was higher in women compared to men, divorced subjects compared to single individuals, and those with mother-to-child transmission or injection drug use and blood products compared to sexual transmission. The risk of progression to death was higher in the 45 to 54 and over 55 age groups compared to the 0 - 14 age group. Additionally, the adjusted correlation was not statistically significant for most subgroups. The results showed a strong correlation between the use of AIDS drugs and progression to death. The risk ratio of death in patients receiving cART was 0.19, which was lower than in those who were not treated (P < 0.000). The risk ratio of AIDS-related death in people with tuberculosis was 4.1 times that of people without a history of tuberculosis (P < 0.029).
| Variables | Frequency | Crude Hazard Ratio | 95% CI | P - Value | Standardized Hazard Ratio | 95% CI | P-Value |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Female | 51 | 1.00 | 1.00 | ||||
| Male | 150 | 3.39 | 1.62 - 7.07 | 0.001 | 0.70 | 0.15 - 3.09 | 0.640 |
| Age group | |||||||
| 0 - 14 | 5 | 1.00 | 1.00 | ||||
| 15 - 24 | 24 | 0.31 | 0.09 - 1.04 | 0.058 | 0.56 | 0.10 - 2.94 | 0.496 |
| 25 - 34 | 83 | 0.58 | 0.20 - 1.65 | 0.312 | 0.91 | 0.21 - 3.99 | 0.911 |
| 35 - 44 | 52 | 0.51 | 0.17 - 1.55 | 0.239 | 0.79 | 0.17 - 3.65 | 0.763 |
| 45 - 54 | 27 | 0.85 | 0.26 - 2.78 | 0.79 | 2.35 | 0.48 - 11.46 | 0.290 |
| ≥ 55 | 10 | 1.77 | 0.43 - 7.27 | 0.42 | 4.31 | 0.74 - 24.90 | 0.102 |
| Marital status | |||||||
| Single | 64 | 1.00 | 1.00 | ||||
| Married | 93 | 0.65 | 0.39 - 1.10 | 0.112 | 0.81 | 0.45 - 1.45 | 0.496 |
| Widow | 17 | 0.26 | 0.08 - 0.87 | 0.029 | 1.24 | 0.61 - 2.49 | 0.541 |
| Divorced | 27 | 0.93 | 0.48 - 1.77 | 0.813 | 0.84 | 0.14 - 5.08 | 0.855 |
| Ways of transmission | |||||||
| Sexually transmission n | 65 | 1.00 | 1.00 | ||||
| Mother to child | 3 | 4.00 | 0.84 - 18.91 | 0.080 | 2.32 | 0.21 - 25.32 | 0.488 |
| Blood productions | 2 | 5.00 | 1.05 - 23.68 | 0.042 | 1.44 | 0.20 - 10.41 | 0.716 |
| Injectable addiction | 131 | 4.67 | 2.24 - 9.77 | 0.000 | 2.38 | 0.83 - 6.83 | 0.107 |
| ART | |||||||
| No | 63 | 1.00 | 1.00 | ||||
| Yes | 138 | 0.17 | 0.10 - 0.28 | 0.000 | 0.19 | 0.11 - 0.33 | 0.001 |
| Tuberculosis | |||||||
| Negative Tuberculosis | 194 | 1.00 | 1.00 | ||||
| Positive Tuberculosis | 7 | 1.14 | 0.35 - 3.63 | 0.823 | 4.11 | 1.15 - 14.65 | 0.029 |
| Hepatitis B | |||||||
| No | 192 | 1.00 | 1.00 | ||||
| Yes | 9 | 1.43 | 0.44 - 4.56 | 0.545 | 2.44 | 0.66 - 9.04 | 0.180 |
| Hepatitis C | |||||||
| No | 65 | 1.00 | 1.00 | ||||
| Yes | 136 | 4.42 | 2.12 - 9.22 | 0.000 | 2.56 | 0.86 - 7.60 | 0.090 |
Effect of Various Predictors on Survival Times for Progression from HIV-Positive to Death Using the Cox Regression Model in Qazvin Province from 1991 to 2021
Survival rates from HIV infection to AIDS and death are shown in Table 3. Based on these results, the one-year, five-year, and ten-year survival rates from HIV infection to AIDS were 98%, 89%, and 71%, respectively. The one-year, five-year, and ten-year survival rates from the time of HIV infection recognition to death were 93%, 69%, and 43%, respectively.
| Survival Time (y) | Total Patients | Event | Missing | Probability of Survival | Standard Error | 95% CI |
|---|---|---|---|---|---|---|
| From HIV infection to AIDS | ||||||
| 1 | 132 | 2 | 4 | 0.98 | 0.010 | 0.94 - 0.99 |
| 2 | 126 | 1 | 14 | .097 | 0.013 | 0.93 - 0.99 |
| 3 | 111 | 3 | 12 | 0.95 | 0.019 | 0.89 - 0.97 |
| 4 | 96 | 1 | 17 | 0.94 | 0.021 | 0.87 - 0.97 |
| 5 | 78 | 4 | 7 | 0.89 | 0.031 | 0.81 - 0.93 |
| 6 | 67 | 5 | 9 | 0.82 | 0.040 | 0.72 - 0.89 |
| 7 | 53 | 1 | 9 | 0.81 | 0.042 | 0.70 - 0.87 |
| 8 | 43 | 2 | 0 | 0.77 | 0.048 | 0.66 - 0.85 |
| 9 | 41 | 1 | 5 | 0.75 | 0.050 | 0.63 - 0.83 |
| 10 | 35 | 2 | 6 | 0.71 | 0.056 | 0.58 - 0.80 |
| From HIV infection to death | ||||||
| 1 | 173 | 12 | 5 | 0.93 | 0.019 | 0.88 - 0.96 |
| 2 | 456 | 7 | 14 | 0.88 | 0.024 | 0.83 - 0.92 |
| 3 | 135 | 11 | 10 | 0.81 | 0.030 | 0.74 - 0.86 |
| 4 | 114 | 10 | 16 | 0.74 | 0.035 | 0.66 - 0.80 |
| 5 | 88 | 6 | 5 | 0.69 | 0.038 | 0.61 - 0.76 |
| 6 | 77 | 7 | 9 | 0.63 | 0.041 | 0.54 - 0.70 |
| 7 | 61 | 4 | 8 | 0.58 | 0.043 | 0.49 - 0.66 |
| 8 | 49 | 3 | 1 | 0.55 | 0.045 | 0.45 - 0.63 |
| 9 | 45 | 4 | 2 | 0.50 | 0.047 | 0.40 - 0.59 |
| 10 | 39 | 5 | 7 | 0.43 | 0.049 | 0.34 - 0.53 |
Survival Time from HIV Infection to AIDS and Dying in Qazvin Province Between 1991 Until 2021
The survival rate of progression from HIV to death by gender is shown in Figure 1, indicating that the survival rate from HIV to death was higher in women than in men.
5. Discussion
In this study, the survival rates of people living with HIV and AIDS within 1, 5, and 10 years were evaluated. The one-year, five-year, and ten-year survival rates from diagnosis of HIV to AIDS were 98%, 89%, and 71%, respectively, and the one-year, five-year, and ten-year survival rates from HIV diagnosis to death were 93%, 69%, and 43%, respectively. The use of antiretroviral (ART) drugs has been identified as the most important preventive factor for reducing the progression of disease to death from AIDS.
A few studies have calculated the time course from HIV to AIDS and from HIV to death. For instance, a study in Brazil estimated the 30-month survival rate of HIV-infected patients to be 70% (14). In Italy, the 10-year survival rate of HIV-infected individuals with non-AIDS-related complications was 44% (15). In the present study, the survival rate of HIV-positive patients receiving combination antiretroviral therapy (cART) was 0.19 compared to those who did not receive treatment. This shows that, although HIV/AIDS was a major cause of death in the 1980s, people living with HIV/AIDS today have a longer life expectancy due to the emergence of HIV/AIDS drugs (16). Observational studies in both high- and low-income countries have indicated that ART treatment has significantly reduced AIDS-related death rates from 92% to 52% (17).
Evidence from randomized clinical trials has shown that early initiation of antiviral therapy (ART) combined with anti-tuberculosis therapy reduces mortality, especially in patients with severe immune deficiency. In studies conducted in Cambodia, the United States, and South Africa, the Hazard Ratio for AIDS and tuberculosis was reduced by 38 - 68% after antiretroviral therapy (ART) and treatment for tuberculosis (18). According to available evidence, tuberculosis has always been a significant cause of disease progression in people living with HIV (19). In this study, the risk of death due to AIDS in people with tuberculosis was 4.1 times that of non-infected individuals, which was statistically significant. This is likely due to the simultaneous infection of these two diseases, leading to an increased risk (P < 0.029). Lopez-Gatell et al. showed that the risk of death from AIDS in HIV-positive people with TB is 2.4 times that in people who are only infected with HIV (20), highlighting the importance of anti-tuberculosis treatment in HIV-positive individuals. In 2004, the World Health Organization (WHO) issued temporary policies on joint HIV/TB programs, emphasizing three distinct goals: Establishing and strengthening the mechanism of co-administration of anti-TB and anti-HIV drugs; reducing the burden of tuberculosis among people living with HIV and starting antiviral treatment on time; and decreasing the HIV burden among people suspected of having TB (21).
In the univariate analysis, the progression of AIDS to death was higher in men than in women, which can be attributed to the small sample size of women compared to men and the possibility of random error. Due to the difference in sample size between men and women, the difference in survival between the two groups, and the higher rates of sensitization in men than in women (12% vs. 8%, respectively), the survival rate between men and women should be compared with caution.
In the present study, the majority of HIV-positive individuals were men, with 75% of injecting drug users being infected with AIDS. The main mode of transmission was drug injection, and 82% of the HIV-infected men were injecting drug users. One reason for the high transmission rate of injecting drug addiction in comparison to sexual relationships could be the prohibition of homosexuality and certain heterosexual practices in the Islamic Republic of Iran. However, HIV transmission has been reported to vary in different parts of the world. For example, in Taiwan, the most common mode of HIV transmission is reported to be contact with homosexuals and heterosexuals, while transmission of infection through the use of injectable drugs (IDUs) is less common (22). Evidence has indicated that access to equipment such as sterile injections, methadone therapy, and services for the underprivileged has successfully reduced the risk of HIV transmission among injecting drug users (19, 20, 22-24). According to studies by the US Centers for Disease Control, the most common way of transmitting AIDS in the USA is through heterosexual contact (24).
This study also had several limitations. First, a more accurate estimate of survival requires dependable sources of data from prospective studies, whereas the present research was a retrospective cohort study and was registered at the AIDS Behavioral Disease Counseling Center. The quality and precision of the estimated survival rate depended primarily on the quality of the recorded data, which could not be changed, and information bias was possible. Second, in order to assess the time of survival from HIV to death, the "diagnosis time" was considered to be the beginning of HIV infection, while some people may have been infected long before diagnosis, which can result in an underestimation of the actual interval between the onset of HIV infection and the onset of AIDS or death. Third, continuous follow-up is needed to determine the true time of AIDS onset. Because some patients do not visit regularly, the actual onset time of AIDS may be delayed. Fourth, there is the possibility of a statistically significant difference between the basic characteristics of the participants in this study and those who were lost to follow-up, which could lead to selection bias in the results of the study. Additionally, considering that in this study, we evaluated the cumulative incidence of HIV to AIDS and from HIV to death only among those who were referred to the Behavioral Diseases Counseling Center, the generalization of the study findings to all HIV/AIDS-infected patients in the main population should be treated with caution. However, despite some limitations, this study contains a number of important messages for health policymakers.
5.1. Conclusions
This research focuses on the most prevalent and main factors affecting the interval between HIV infection and AIDS, and from HIV to death. Our study showed that ART increased the survival of patients living with HIV. The risk of death from AIDS in patients receiving ART was 0.19 compared to those who did not receive treatment. We demonstrated that co-infection with TB was among the most important prognostic factors for progression to death. Thus, the risk of death due to AIDS in patients with tuberculosis is 4.1 times that in non-infected people.