1. Background
Vitamin D (Vit-D) deficiency is known to be an epidemic condition (1). In Iran, the prevalence of Vit-D deficiency in men and women is 44% and 64%, respectively (2). The role of Vit-D is well-known in calcium and phosphorus homeostasis, but emerging evidence suggests that Vit-D may also play a significant role in cardiovascular health (3). Several studies have demonstrated an association between Vit-D deficiency and increased risk of cardiovascular diseases, including hypertension, coronary artery disease (CAD), and heart failure (4, 5). The myocardium is a vital target tissue for Vit-D (6). Three methods for Vit-D impact on the myocardium are proposed: (1) direct regulation of renin gene expression; (2) presence of Vit-D receptors on myocyte membrane; and (3) hyperparathyroidism caused by Vit-D deficiency may result in cardiac hypertrophy (4, 7). Low 25-hydroxyvitamin D levels have been discovered as an independent risk factor for overall, cardiovascular, and cancer mortality in patients referred for coronary angiography (8).
Despite evidence linking Vit-D deficiency with heart dysfunction, the relationship between Vit-D levels and ventricular function in normal coronary patients remains unclear, and objective evidence, such as echocardiographic findings, has not been adequately investigated. Previous studies have shown different and contradictory results (6-9). Previous studies have primarily investigated the relationship between Vit-D status and pulmonary hypertension; some of them revealed that patients with pulmonary hypertension have lower serum Vit-D levels than healthy individuals (10), and to the best of our knowledge, this is the first study to examine the relationship between Vit-D status and both left and right ventricular function. Therefore, an echocardiographic study was conducted to examine the association between Vit-D levels and ventricular systolic function in normal coronary patients. We hypothesized that Vit-D insufficiency or deficiency may be associated with impaired ventricular function, as assessed by echocardiography, even in the absence of significant CAD, which could provide insights into the potential cardioprotective effects of Vit-D supplementation.
3. Methods
3.1. Study Population
In 2019 and 2020, a cross-sectional investigation was carried out for this research project. Patients who were referred for angiography to Bu-Ali Sina Hospital in Qazvin but did not have normal CAD or had only mild CAD were included in the study sample. The following exclusion criteria were taken into consideration: A history of structural heart disease (valvular or congenital heart disease), arrhythmia or atrial fibrillation, use of medications that affect the heart's electrical conduction, use of Vit-D supplements within the previous month, cerebrovascular illness, abnormal thyroid tests, secondary hypertension, renal failure, and immunodeficiency. Patients’ histories, including Body Mass Index (BMI), body surface area (BSA), systolic blood pressure (SBP), diastolic blood pressure (DBP), underlying diseases such as dyslipidemia (DLP) and diabetes mellitus (DM), and drug histories were documented. Informed consent was obtained from all patients. We conducted our study in compliance with the Helsinki declaration, and the study was approved by the ethics committee of Qazvin University of Medical Sciences under the ethics code of IR.QUMS.REC.1399.104.
3.2. Echocardiography
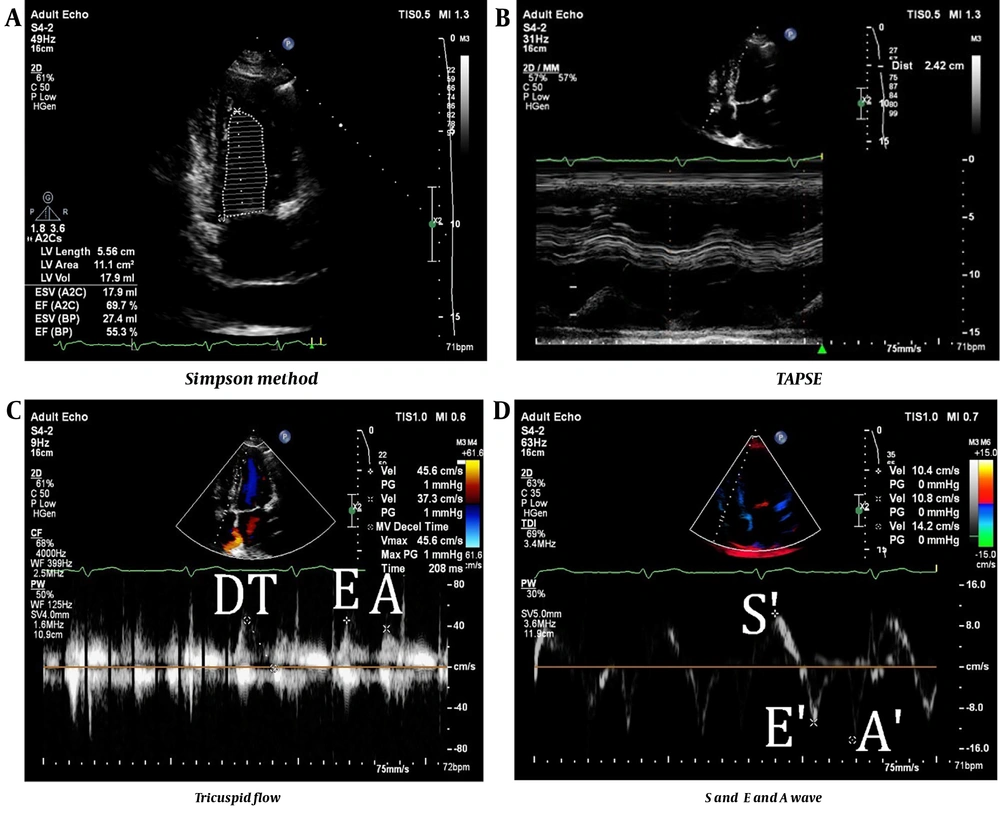
At the time of angiography, transthoracic echocardiography was done on each sample by an echocardiography fellow. With the Philips Affiniti 50 Ultrasound Machine (Philips Healthcare, Andover, MA, USA) in the left lateral decubitus position, the characteristics of the ventricle's systolic and diastolic function were measured. Probes operating at 2.5 MHz and 2.5 - 3.5 MHz were used, respectively, for the Doppler measurements. The measurements were carried out in compliance with guideline 14 of the American Echocardiographic Association. Atrial and ventricular volumes were indexed using BSA to standardize the volumetric comparisons. The Simpson method was used to compute the ejection fraction (LVEF) (11).
Right ventricular fractional area change (RVFAC) and tricuspid annular plane systolic excursion (TAPSE) were also measured as parameters of right systolic function (12). Diastolic function was assessed by recording the peak velocities of diastolic flow and calculating the E/A ratio and deceleration time (DT). Tissue Doppler echocardiography was used to evaluate right ventricle RV diastolic function by measuring velocities at the tricuspid annulus. These measurements were performed using appropriate imaging techniques and settings (13) (Figure 1).
Echocardiographic methods for evaluation of the left and right systolic functions. A, simpson method for evaluation of the left systolic function; B, tricuspid annular plane systolic excursion; C, trans-tricuspid flow and is delineated with pulse wave Doppler presenting E and A waves; D, right ventricular tissue using the pulse-wave tissue Doppler in the apical 4-chamber view
Serum levels of Vit-D3 in the blood of patients were measured using the chemiluminescent immunoassay (CLIA) technique (Abbott Diagnostics, USA), and the results were recorded. The CLIA technique is a highly sensitive and specific method for measuring Vit-D levels that uses a monoclonal antibody that binds to 25-hydroxyvitamin D, the main circulating form of Vit-D in the body (14). The normal range of Vit-D levels was defined as 30 - 100 ng/mL, according to Endocrine Society guidelines (15). In the present study, we divided the patients into two groups: Vit-D deficient (Vit-D < 30 ng/dL) and Vit-D sufficient (Vit-D ≥ 30 ng/dL) (16).
3.3. Statistical Analysis
This study was designed to detect the difference between ventricular function based on Vit-D levels in normal coronary patients. We calculated the sample size based on the following assumptions: (1) ESV in patients with normal Vit-D levels was 96 ± 20 mL and in patients with Vit-D deficiency was 119 ± 49 mL (10); (2) a case-control ratio (κ) of 2: 1; (3) the significance level 0.05; and (4) the power 0.8. Using the formula for independent t-test:
n1, 2 = sample size of Group 1 and 2, δ1,2 = standard deviation of Group 1 and 2, Δ = difference in group means, κ = ratio = n2/n1, Z1-α/2 = two-sided Z value, Z1-β = power, we obtained the total sample size of the study as 72 patients (24 patients per normal Vit-D group and 48 patients in Vit-D deficient group) (17).
Statistical analysis was performed using SPSS software version 25 (IBM Corp., USA). The quantitative data were reported as mean and standard deviation, whereas the qualitative variables were recorded as frequency and percentage. The chi-square test and, if applicable, the Fisher exact test were used to compare the groups' qualitative data. The quantitative data, on the other hand, were compared using an independent t-test. A statistically significant P-value of less than 0.05 was evaluated.
4. Results
Finally, 74 patients entered the study: 27 patients with normal Vit-D levels and 47 patients with Vit-D deficiency. In both groups, the average patient age was 54 ± 10 years. There were no significant differences in baseline factors such as gender, weight, medications, diabetes history, or hypertension (P > 0.05). However, patients with Vit-D deficiency had higher DBP (P = 0.019). The demographic data of the patients are demonstrated in Table 1.
| Variables | Vitamin D Level | P-Value | ||
|---|---|---|---|---|
| Deficiency n = 47 | Normal n = 27 | Total n = 74 | ||
| Age (y) | 54 ± 10 | 54 ± 10 | 54 ± 10 | 0.996 |
| Sex | 0.111 | |||
| Male | 19 (40.4) | 6 (22.2) | 25 (33.8) | |
| Female | 28 (59.6) | 21 (77.8) | 49 (66.2) | |
| Weight (kg) | 77.7 ± 13.3 | 74.0 ± 11.2 | 76.3 ± 12.6 | 0.227 |
| Height (m) | 163.3 ± 9.2 | 160.8 ± 11.6 | 162.4 ± 10.1 | 0.305 |
| SBP (mmHg) | 123 ± 13 | 124 ± 14 | 123 ± 13 | 0.752 |
| DBP (mmHg) | 78 ± 7 | 73 ± 10 | 76 ± 8 | 0.019 |
| DM | 11 (23.4) | 5 (18.5) | 16 (21.6) | 0.623 |
| Hypertension | 13 (27.7) | 9 (33.3) | 22 (29.7) | 0.607 |
| Smoker | 10 (21.3) | 3 (11.1) | 13 (17.6) | 0.269 |
| Hyperlipidemia | 2 (4.3) | 0 (0.0) | 2 (2.7) | 0.277 |
| Blood sugar (mg/dL) | 121 ± 43 | 118 ± 39 | 120 ± 41 | 0.817 |
| Blood urea nitrogen test (mg/dL) | 15.4 ± 4.9 | 17.9 ± 5.3 | 16.3 ± 5.2 | 0.046 |
| Creatinine (mg/dL) | 0.95 ± 0.21 | 0.93 ± 0.24 | 0.94 ± 0.22 | 0.756 |
| Hemoglobin (mg/dL) | 13.9 ± 1.7 | 13.6 ± 1.6 | 13.8 ± 1.6 | 0.379 |
| Acetylsalicylic acid | 12 (25.5) | 12 (44.4) | 24 (32.4) | 0.094 |
| Beta blocker | 11 (23.4) | 13 (48.1) | 24 (32.4) | 0.029 |
| ACE/arbs | 9 (19.1) | 6 (22.2) | 15 (20.3) | 0.752 |
| Statin | 8 (17.0) | 9 (33.3) | 17 (23.0) | 0.108 |
| Oral hypoglycemic medications | 9 (19.1) | 5 (18.5) | 14 (18.9) | 0.947 |
The Demographic Data of the Patients a
Table 1 shows that there was no significant change in LVEF, Left Ventricular End-Diastolic Volume Index (LVEDVi), or Left Ventricular End-Systolic Volume Index (LVESVi) between the groups (P > 0.05). Additionally, 29.6% of the patients with normal Vit-D levels had abnormal LVEF, compared to 21.3% of patients with Vit-D deficiency, which is not a significant difference.
As mentioned in Table 2, we found no significant difference in right ventricular systolic and diastolic function parameters (P > 0.05). While 18.5% of patients with normal Vit-D levels had a TAPSE above 1.6, 23.4% of Vit-D deficient patients had an abnormal TAPSE, which is not statistically significant. The majority of patients in both groups had right and left ventricular function metrics within normal limits, and there was no correlation observed between ventricular dysfunction and Vit-D insufficiency (Table 3).
| Parameter and Criteria | Normal Vit-D | Vit-D Deficiency | P-Value |
|---|---|---|---|
| LVEF | 0.420 | ||
| Normal | 19 (70.4) | 37 (78.7) | |
| Abnormal | 8 (29.6) | 10 (21.3) | |
| LVEDVi | 0.100 | ||
| Normal | 24 (88.9) | 46 (97.9) | |
| Abnormal | 3 (11.1) | 1 (2.1) | |
| LVESVi | 0.340 | ||
| Normal | 22 (81.5) | 42 (89.4) | |
| Abnormal | 5 (18.5) | 5 (10.6) | |
| LA diameter | 33.7 ± 3.4 | 34.7 ± 5.9 | 0.433 |
| LA volume | 46 ± 13 | 49 ± 21 | 0.550 |
| DT (M) | 216 ± 46 | 211 ± 59 | 0.739 |
| A (M) | 16.24 ± 3.76 | 7.79 ± 1.74 | 0.473 |
| E (M) | 9.31 ± 2.42 | 12.02 ± 2.38 | 0.988 |
| Septal A' (M) | 8 ± 2 | 8 ± 2 | 0.425 |
| Septal E' (M) | 7 ± 2 | 8 ± 3 | 0.065 |
| Septum | 8 ± 1 | 8 ± 1 | 0.399 |
| Posterior | 8 ± 1 | 8 ± 1 | 0.912 |
Left Ventricular Systolic Function Parameters Based on the Vitamin D Level
| Parameter a and Criteria | Normal Vit-D | Vit-D Deficiency | P-Value |
|---|---|---|---|
| E/A | 0.646 | ||
| No diastolic dysfunction | 15 (55.6) | 21 (44.7) | |
| Impaired-relaxation | 5 (18.5) | 12 (25.5) | |
| Pseudo-normal | 7 (25.9) | 14 (29.8) | |
| Restricted relaxation | 0 (0.0) | 0 (0.0) | |
| E/E´ | 0.914 | ||
| > 6 | 10 (37) | 18 (38.3) | |
| < 6 | 17 (63) | 29 (61.7) |
Right Ventricular Systolic Function Parameters Based on the Vitamin D Level
5. Discussion
This research contributes to the growing body of evidence on the role of Vit-D in cardiovascular health. The findings of this investigation revealed that there is no significant difference in ventricular function measured by echocardiographic parameters between the groups in general. In other words, in normal coronary patients, there was no significant association between ventricular systolic dysfunction and Vit-D status.
This result is noteworthy as it challenges the commonly held belief that Vit-D status might influence heart function, particularly ventricular systolic function. Some studies have reported a potential link between Vit-D deficiency and impaired cardiac function in congestive heart failure patients. These results suggest that Vit-D deficiency may impair both systolic and diastolic functions of the left ventricle (LV), leading to increased cardiac workload, chamber dilatation, and hypertrophy. In our study, no difference was observed between the groups regarding left ventricular systolic function in normal coronary patients. Our findings are consistent with those of previous studies that have failed to establish a clear link between Vit-D levels and various echocardiographic parameters, such as LVEF, LVEDV, LVESV, LVM, LAV, E/A ratio, E/e’ ratio, and DT. For instance, Vit-D status did not significantly affect LVEF or wall velocity (S) in individuals studied by Macedo et al. (18). The findings of Pandit et al. (19), which also found no Vit-D status dependence of left ventricular diastolic function parameters, such as diastolic E/E' and E/A, Left Ventricular Muscle Mass Index (LVMi), Left Atrial Volume Index (LAVi), and mitral valve DT, are similar to the findings of the current study. Similarly, Akhavan-Khaleghi et al. studied patients without significant CAD and found no difference in LA function, as evaluated by 2DSTE, between subjects with and without Vit-D deficiency after adjustment for the confounding factors (20). This aligns with the recommendations released by the U.S. Preventive Services Task Force, which cited insufficient evidence to recommend adults take Vit-D or any other supplement to prevent cardiovascular disease (21).
These discrepancies may be due to differences in study design, sample size, population characteristics, Vit-D measurement methods, echocardiographic techniques, confounding factors, and the multifactorial nature of ventricular dysfunction, which can be influenced by various factors such as genetics, lifestyle, and comorbidities. Moreover, the causal relationship between Vit-D and cardiac function remains unclear, as observational studies cannot rule out reverse causation or residual confounding. Therefore, randomized controlled trials are needed to determine whether Vit-D supplementation can improve cardiac function and prevent cardiovascular events (22). It is possible that Vit-D alone does not have a direct impact on ventricular function but rather interacts with other factors (such as DBP) to contribute to cardiac health (23). The study found that patients with Vit-D deficiency had higher DBP levels compared to those with sufficient Vit-D levels. Observational data have demonstrated that poor Vit-D status is associated with an increased risk of hypertension (21). This is important in IHD, as high blood pressure is a major risk factor for the development of the disease. This suggests a potential link between Vit-D status and blood pressure regulation.
Jorge et al. (24) investigated individuals with suspected heart failure but normal EF and found that, while LVEF did not change, the wall velocity (S) was considerably lower in the Vit-D deficient group, indicating systolic dysfunction. Macedo et al. (18) found no significant difference in left ventricular end-diastolic diameter and volume (LVEDD and LVEDV), but they did detect a significant difference in left atrial diameter and volume (LAD and LAV) in the Vit-D deficient group. They determined that the discrepancy could be attributed to Vit-D insufficiency, but the variances were minor, and the data should be corrected for BSA before comparing. They discovered that the difference in LADi was not statistically significant for either group, and that the difference in LAVi remained significant (14).
Jorge et al. (24) discovered that the E/E' ratio was much greater in the Vit-D deficient group, although E' was significantly lower. This shows that the Vit-D deficient group has more severe left ventricular diastolic dysfunction. Akin et al. (25) found that diastolic function parameters (including LAD, IVRT, and E/E' ratio) were significantly greater in the Vit-D deficient group; however, these differences were not statistically significant. Some research has found a link between Vit-D levels and left and right ventricular systolic function; nevertheless, the claimed discrepancies across functional parameters were not clinically or pathophysiologically plausible. For example, Abdel Rahman et al. studied individuals with systolic heart failure and discovered that, while left ventricular systolic function was poorer in the Vit-D deficient group, diastolic function was better (13).
The strengths of our study include the use of a reliable method for measuring Vit-D levels and a comprehensive echocardiographic examination. This study has limitations, such as a small sample size and other confounding variables. Another consideration is the potential impact of confounding variables. It is possible that unmeasured variables influenced the results. For example, lifestyle factors such as diet and physical activity, which are known to affect both Vit-D levels and cardiovascular health, may have influenced the findings. Future studies should aim to address these confounding variables to provide a clearer understanding of the relationship between Vit-D and ventricular function.
It is worth noting that the study sample in the current study consisted of a specific population group. Further research involving a larger and more diverse sample is warranted to validate these findings in different demographic groups. Also, the echocardiographic parameters used in this study provided only a snapshot of ventricular function and may not capture subtle changes over time. Invasive procedures can accurately quantify ventricular function parameters, but due to their inability in everyday medicine, alternative methods are required. Echocardiographic measures are currently employed to assess ventricular systolic and diastolic performance (26). Furthermore, although invasive technologies can correctly assess ventricular function parameters, due to the inability of executing them in routine practice, echocardiography measurements are utilized to evaluate ventricular systolic and diastolic function, according to current standards. Additionally, the Vit-D status of our participants was determined at a single time point, which may not accurately reflect their long-term Vit-D status. It is suggested that in the future, multicenter studies with larger sample sizes and long-term follow-up periods should be conducted.
5.1. Conclusions
The results of this study showed that, in general, there was no significant difference between ventricular function and Vit-D deficiency as determined by echocardiographic parameters. Although this study did not show a significant relationship between Vit-D levels and ventricular function, it is important to consider the study's limitations and interpret the findings alongside other existing research on this topic. More research is needed to fully understand the potential association between Vit-D and ventricular systolic and diastolic dysfunction. It is possible that different populations or specific subgroups show stronger associations. In addition, examining other echocardiographic parameters or considering other indicators of ventricular function can provide a better understanding of the issue.