1. Background
Crimean-Congo hemorrhagic fever (CCHF) is a hemorrhagic and dangerous disease caused by a virus from the Bunyaviridae family and the genus Nairovirus (1). This virus is transmitted by Hyalomma tick bites (2) or by direct contact with the intestines of newly slaughtered infected animals, blood, secretions of the patient's body, or virus aerosol particles scattered in the air, especially in epidemics and health centers (3). During viremia, the virus is transmitted to a healthy person (4). Congo hemorrhagic fever in livestock has no specific symptoms, and the risk of contagion is very high in the early stages of the disease. The viral load, route of transmission, and source of infection are three important factors that determine the incubation period of the disease (5). The incubation period after a tick bite is 1 to 5 days and a maximum of 9 days, but the incubation period after contact with contamination is 5 to 7 days and a maximum of 13 days. The lowest viral load for disease transmission is between one and ten organisms (6). After a short incubation period, it develops into a fever, chills, myalgia (7), headache, and digestive symptoms (8). As the disease progresses, serious symptoms start to appear, including petechiae, bruising, epistaxis, bleeding gums, and vomiting (9). Approximately 5 days after the onset of the disease, it suddenly enters the bleeding phase and causes severe bleeding (10), symptoms of disseminated intravascular coagulation (DIC) (11), shock occurs, and patients die with these symptoms (12). Diagnosis of the disease is possible based on clinical symptoms, serology, virus culture, and blood PCR to find the virus that causes the disease (13).
This disease was first observed clinically in the 1940s when Russian troops occupied the Crimea Peninsula (14). Congo hemorrhagic fever has been detected in more than 50 countries in Africa, Asia, Eastern Europe, and the Middle East (3). Due to health and economic problems, Iran is also considered an endemic country for CCHF (15). Crimean-Congo hemorrhagic fever is endemic in the North Khorasan province, Sistan and Baluchestan, Isfahan, Fars, Tehran, and Khuzestan provinces of Iran (16). The CCHFV in Iran was first identified in livestock serum and tick studies in the 1970s. The first human infection was diagnosed in 1999 (17). Because warm and dry weather is more favorable for ticks, increasing temperature and decreasing rainfall provide a suitable environment for the growth and reproduction of ticks (18). Therefore, people in tropical areas, such as Ahvaz, have a high chance of contracting this disease.
2. Objectives
The aim of this study was to investigate the epidemiological and clinical pathological factors in suspected Crimean-Congo fever patients referred to hospitals where a significant number of CCHF patients had been cared for.
3. Methods
This cross-sectional study was carried out on 96 patients admitted to Razi, Golestan, and Imam Khomeini Hospitals, which are referral hospitals for infectious diseases in Ahvaz, from 2011 to 2023. To investigate epidemiological information (i.e., age, gender, educational status, occupation, and time of infection) and any exposure to risk factors (such as a history of contact with livestock), a questionnaire was filled out for each participant that could be associated with this infection.
Based on standard case definitions from World Health Organization resources, all of the suspected and confirmed CCHF medical records' pertinent data were extracted and studied (19). Suspicious cases were defined as those presenting with bleeding, fever, and muscle pain, especially in epidemiological CCHF regions and among those in contact with livestock.
In probable cases, the fever incubation period of this disease is 1 to 7 days, with leukopenia, thrombocytopenia, and leukocytosis manifesting, and hemorrhagic symptoms are diagnosed. In CCHF-confirmed cases, the presence of IgG or IgM serum viral antibodies by enzyme-linked immunosorbent assay (ELISA) was positive (13).
The recorded data were analyzed with SPSS software, and P-values < 0.05 were considered significant. Values are expressed as mean ± SD. Word software was used to draw the figure.
4. Results
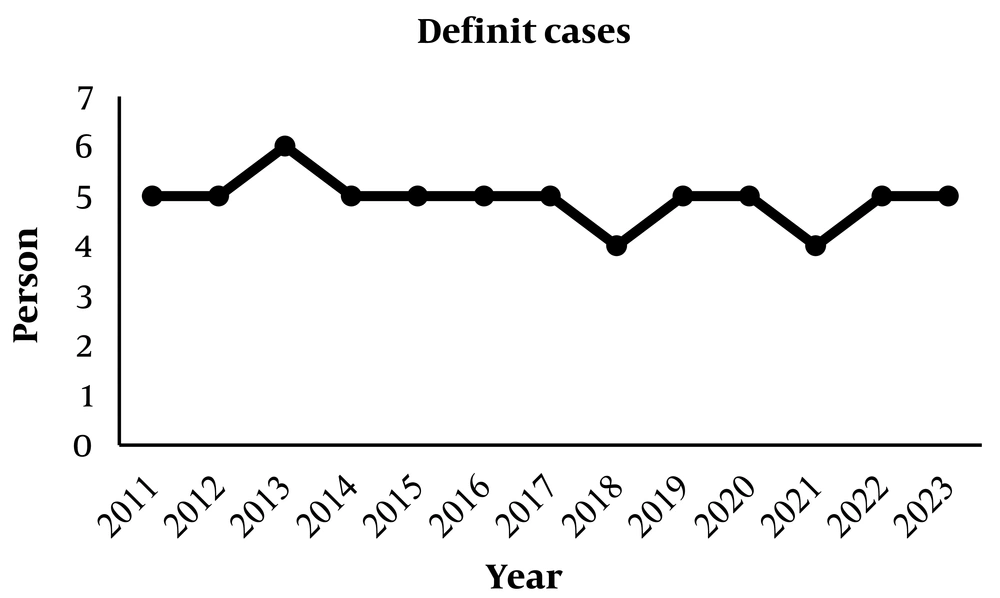
A total of 96 people were included in this study, 24 of whom were men and 72 were women; the overall male-to-female ratio was 1: 3. Thus, a female preponderance was seen in this study and was statistically significant (P < 0.001). Of these, 32 were suspected of having the disease (6 men and 26 women), and 64 definitely had the disease (18 men and 46 women). The mean age of the studied subjects was 46 years (range, 16 - 76 years). The mean age of females and males was 39.5 ± 6.11 and 31.50 ± 2.90 years, respectively (Figure 1).
The occupational distribution of the patients participating in the study was 36 housewives (37.5%), 12 self-employed (12.5%), 4 cattle farmers (4.2%), 6 shepherds (6.2%), 6 slaughterhouse workers (6.2%), 8 butchers (8.4%), 10 nurses (10.5%), and 14 employees (14.5%).
In terms of season, 36 people were infected in spring (37.5%), 54 in summer (56.25%), and 6 in autumn (6.25%).
In the study of participants, 74 people (77%) had a sudden onset of symptoms, 90 people (93.75%) had a fever, and 54 (56.25%) participants had bleeding. Eighty-six people (89.5%) had muscle pain, and bleeding was observed in 56.25% of the patients, with epistaxis and hematuria being the most common forms of bleeding. Bleeding in patients was reported as 39% from the nose, 9.2% from the mouth, 29.6% from hematuria, 11.1% from vomiting blood, and 11.1% from the eyes.
In terms of the history of contact with animals, 66 patients (68.75%) had a history of contact with animals, and 30 patients (31.25%) had no history of contact with animals. Among those who had contact with animals, 30 people (45.5%) had a history of contact with live animals, 12 people (18%) had contact with meat and other animal body parts, 16 people (24.5%) had a history of animal slaughter, and 8 people (12%) had a history of contact with fresh animal carcasses and secretions.
About 84 serum samples were sent to the laboratory of Ahvaz Province, and 42 of these cases were positive for CCHF by ELISA test. Of these, 30 (36.5%) were (IgG−, IgM+), and 12 (14.5%) had (IgG+, IgM−).
All patients had mild leukopenia, lymphopenia, neutropenia, and thrombocytopenia; mean hemoglobin levels were 10.11 ± 2.6 g/dL. We observed that patients had slightly high ALT (128 ± 67.2 U/L), meaning approximately 88 U/L more than normal, and AST (165 ± 116 U/L), meaning approximately 125 U/L more than normal, and ALP (298 ± 57.5 U/L), meaning approximately 158 U/L more than normal in the laboratory findings. However, average increases in erythrocyte sedimentation rate (ESR) level (76.5 ± 8.6 mm/hr) were seen. Additionally, kidney evaluation of patients showed normal Cr (0.8 ± 0.1 mg/dL) and BUN (15.7 ± 1.2 mg/dL) levels (Table 1). One of the patients died, and the rest have recovered.
| Variables | Values |
|---|---|
| ALP (U/L) | 298 ± 57.5 |
| ALT (U/L) | 128 ± 67.2 |
| AST (U/L) | 165 ± 116 |
| INR (s) | 1.2 ± 0.19 |
| PT (s) | 12.46 ± 2.6 |
| PTT (s) | 33.92 ± 11.6 |
| PLT (103/µL) | 111.8 ± 10.2 |
| Hb (g/dL) | 10.11 ± 2.6 |
| ESR (mm/h) | 76.5 ± 8.6 |
| CT (min) | 4.27 ± 0.12 |
| Bill (µmol/L) | 1.04 ± 0.1 |
| FBS (mg/dL) | 116 ± 36.2 |
| BUN (mg/dL) | 15.7 ± 1.2 |
| Cr (mg/dL) | 0.8 ± 0.1 |
| K (mmol/L) | 4 ± 0.21 |
| Na (mmol/L) | 137 ± 32.1 |
| WBC (103/µL) | 1164 ± 2.3 |
a Values are expressed as mean ± SD.
5. Discussion
Since there are many reports about the prevalence of CCHF in Iran (17, 20), it is essential to investigate the incidence and symptoms of the disease in provinces with high infection rates, such as Khuzestan Province. On the other hand, Khuzestan's ecological parameters are ideal for tick life cycles to be successfully completed (8). Also, according to epidemiological research, CCHF is more prevalent in areas with warm climates (21). According to a survey done in Iraq in 2022, half of the cases were related to Tighar Province in the southeast of Iraq, while the rest of the cases were reported in 12 different provinces (22). Thus, it is simple to see the significance of being on the border with a disease-prone country, given that Khuzestan is close to the southeast of Iraq, and animal movement occurs on the other side of the boundaries.
The goal of this study was to characterize the epidemiological and clinical pathological traits of CCHF discovered in Iran (the region of Khuzestan) between 2011 and 2023.
Most Iranian studies that have been published indicate that more men are infected than women, as in the cases below. The results of a study of 24 patients from Zabul and Zahedan cities showed that 70.8% of men and 29.2% of women were infected with this disease (23). SharifiFard et al. also reported in a study conducted from 1995 to 2015 in Khuzestan that the most at-risk occupational groups were farmers and housewives, with frequencies of 28.6% and 26%, respectively (24).
Interestingly, in this study, 72 patients were women and 24 were men, and they were in the age range of 16 - 76 years. This ratio may show that women in the Khuzestan district labor more frequently in risky jobs and are, hence, more susceptible to contracting this disease. As well, according to the findings of our study, it can be seen that the second largest number of infected people were housewives; they may be at risk due to contact with animal blood during cooking and lack of protective methods.
Lack of vector control, living in poor conditions, close proximity to animals, and managing sick patients improperly—these factors could all contribute to an increase in cases (19). The World Health Organization adds that direct contact with patients' blood, saliva, organs, or other bodily fluids can result in human-to-human transmission in medical facilities (19). In addition, several reports have been published so far that butchers, animal handlers, employees of slaughterhouses, people working in agriculture and animal husbandry, and employees of healthcare centers are high-risk groups for developing CCHF (23, 24). Even things like the typical practices of slaughterhouse butchers, such as eating raw liver and holding a knife in the mouth, might exacerbate the prevalence (25). Therefore, the prevention of CCHF can be achieved by adhering to health standards and displaying healthy behaviors (26). Moreover, it should be mentioned that having more information about CCHF and raising knowledge among the general public, particularly among the local medical personnel, can significantly contribute to its prevention and improvement (27).
Our study shows that summer had the highest occurrence of CCHF, followed by spring and autumn, and that winter had no cases of this condition. In this regard, many studies have stated that cases of CCHF occur more during the summer months (28, 29). According to research thus far, CCHF symptoms commonly include headache, high fever, bleeding, back discomfort, vomiting, and muscle pain. 20% of the patients showed no signs of bleeding, and the nose was the organ that bled the most frequently (19).
Among the mentioned symptoms, fever (93.75%), bleeding (56.25%), and muscle pain (89.5%) were considered in the statistical analysis. In this regard, 77% of the patients experienced a quick onset of symptoms, whereas 23% did not. Also, the history of animal contact was looked into in the current study because it is a significant factor in CCHF (30, 31). Based on the findings of our study, 66.78% of the patients had previously experienced exposure to animals in one form or another, and the majority of these were connected to people who had previously had contact with live animals.
Investigations of IgG and IgM antibodies are frequently conducted as two distinct markers of Crimean-Congo hemorrhagic fever virus (CCHFV) in human sera (32). In this study, cases positive for CCHF by ELISA were reported to be 36.5% (IgG−, IgM+), and 14.5% (IgG+, IgM−).
According to our research, the affected patients had elevated levels of ALT and AST enzymes but normal levels of the ALP enzyme. Crimean-Congo hemorrhagic fever virus has the potential to induce significant liver damage in humans, although the mechanism(s) responsible for this harm are not well understood (33). The findings of this study were also confirmed by the biochemical parameters of the liver from Fatma and Turan Aktaş's research (34). Investigation of a separate case of human CCHF in Central Uganda in 2015 also confirmed the findings of our study (35). Prognostic variables for CCHF mortality include PLT, PT, PTT, and INR (36). All the parameters expressed in this study were within the usual range. People IgM+ are reported to be in the acute stage of the disease, while people IgG+ are in the chronic stage (37); therefore, the lack of change in the prognostic variables is well justified given the higher number of IgM+.
Hemoglobin levels are debatable in the diagnosis of early significant bleeding (38). In the present study, the hemoglobin levels decreased, which can indicate the beginning of anemia caused by bleeding.
Erythrocyte sedimentation rate confirms that there is inflammation in the body, and it typically rises in response to particular biological situations such as infectious diseases (39). Our study showed that ESR levels in CCHF patients were significantly higher than the normal range. In line with our findings, various studies have pointed to the increase in ESR levels in Crimean fever patients (40, 41). CT calculates the time required for thrombin to drive the reaction between fibrinogen and fibrin (42). The results of the present study show that the values of this factor were normal. FBS, Bil, Na, and WBC levels increased in CCHF patients. The examinations revealed that the cases noted in other studies had similarly increased (28, 40). However, it should be emphasized that the levels of these variables may vary in studies that focus on the chronic stage of this condition, such as the quantity of WBC, which was found to be lower in one study in contrast to our findings (40).
Other parameters, such as urea, chromium, and potassium, did not change significantly. Finally, given that housewives in this study were the group most at risk of contracting CCHF, it makes sense for them to receive specialized training in the transmission, prevention, symptoms, and treatment of CCHF. Veterinary groups should conduct thorough examinations in these regions to reduce the incidence of CCHF.
5.1. Conclusions
In conclusion, there is a need for increased awareness and monitoring of this issue. It seems that the prevention, management, and control of CCHF in Khuzestan strongly depend on strategies to increase awareness among all sections of society.