1. Background
Cervical cancer is the fourth most common cancer in women worldwide and the second most frequent cancer among Iranian women, following breast cancer (1). Human papillomavirus (HPV) is the main risk factor for cervical dysplasia and cervical cancer (2). More than 200 different HPV types have been recognized, with over 51 types infecting genital areas. However, only certain types, such as HPV16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59, are high-risk and linked with cervical cancer (3). In contrast, low-risk HPV types are asymptomatic or cause benign lesions (4). The high cervical cancer mortality rate in developing countries, including Iran, has been largely attributed to inefficient screening programs (5).
The cervical Papanicolaou (Pap) smear is the best screening method for cervical precancerous lesions. It is preferable to report using a unified system like the Bethesda system. In this system, squamous intraepithelial lesion (SIL) progresses from the precancerous lesions of low-grade SIL (LSIL) to high-grade SIL (HSIL), and finally to squamous cell carcinoma (6). According to the Bethesda system 2001 guidelines (7), atypical squamous cells of undetermined significance (ASCUS) refer to cells that demonstrate more severe changes than inflammatory changes but are not sufficient to diagnose epithelial malignancy (8). The Bethesda system defines ASCUS incidence as less than 5% of all specimens. Additionally, it has been reported that approximately 40 - 50% of ASCUS cases are infected by high-risk HPV. Therefore, ASCUS could indicate a high-risk HPV infection. Conversely, half of the cases with an ASCUS diagnosis are missed for HPV testing (9).
Estimating the distribution of HPV genotypes could alter future preventive strategies. While ASCUS is the most common abnormal finding in a Pap test (10), it is an incompletely defined entity, and the management of these patients remains controversial (11).
2. Objectives
Therefore, the current study aimed to evaluate the prevalence of HPV and genotype distribution in women with minor cervical cytological abnormalities.
3. Methods
This retrospective study involved 160 Iranian women. We selected 80 women with minor cervical cytological abnormalities (WMCA) and 80 age-matched women with normal cervical cytology (WNC) who underwent cervical cancer screening with cytology and HPV testing between November 2020 and January 2023. The participants were selected using a convenient sampling method from women who attended the Central Diagnostic Lab of the Academic Center for Education, Culture, and Research, Mashhad Branch. All the studied women were visited by gynecologists, dermatologists, or urologists, and the HPV test was requested by the specialist. This study was approved by the ethics committee with the code IR.ACECR.JDM.REC.1402.021.
Papanicolaou tests were performed using liquid-based cervical cytology. A sample of cells was collected from the cervix into a liquid-based specimen vial, which was analyzed to identify the presence of HPV viral DNA. All samples were taken by an experienced midwife. The Bethesda system was applied for reporting Pap smear results. Patients with mild dysplasia were included in the study, while women with moderate or severe dysplasia, such as HSIL or cervical cancer, and women with missing data, were excluded from the study.
Human papillomavirus genotyping was performed using a Papilloma Strip test by Operon Company by trained experts. This test is based on reverse hybridization and detects DNA samples qualitatively. The high + low Papilloma Strip kit identifies the following HPV genotypes: High-risk HPV types (HPV16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59), Medium-risk HPV types (HPV26, 53, 66, 67, 68, 69, 70, 73, and 82), and low-risk HPV types (HPV6, 11, 40, 42, 43, 44, 54, 61, 62, 67, 70, 71, 72, 74, 81, 83, 84, and 94). According to the manual of the kit, the sensitivity of the kit was satisfactory for all genotypes. No cross-reaction was detected with bacterial and viral pathogens such as Ureaplasma urealyticum, Mycoplasma genitalium, Candida albicans, herpes simplex, Neisseria gonorrhoeae, and others.
Statistical analyses were performed with SPSS software version 22. Descriptive analyses, including frequencies, percentages, and averages, were used to explain the results. A chi-square test was performed for the qualitative variables. When the P-value was < 0.05, differences were considered statistically significant.
4. Results
Human papillomavirus genotyping was conducted for 80 WMCA and 80 WNC. The WMCA group included 59 women with ASCUS and 21 women with LSIL. The mean age of participants was 33.9 ± 9.1 years (range: 18 - 63 years). There was no statistical difference in age between the two studied groups (WMCA and WNC). Overall, 55.6% of all participants were HPV positive. The HPV DNA was detected in 71.3% of the WMCA group (66.1% in those with ASCUS and 85.7% in those with LSIL) and 40% of the WNC group (Table 1).
| Cervical Cytology Findings | HPV | Total | |
|---|---|---|---|
| Negative | Positive | ||
| Normal (NILM) | 48 (60) | 32 (40) | 80 (50) |
| Abnormal | 23 (28.75) | 57 (71.25) | 80 (50) |
| ASCUS | 20 (33.9) | 39 (66.1) | |
| LSIL | 3 (14.3) | 18 (85.7) | |
| Total | 71 (44.4) | 89 (55.6) | 160 (100) |
| P-value | < 0.001 | ||
Prevalence of Human Papillomavirus by Different Cervical Cytology Findings a
The maximum percentage of HPV-positive women was in the age range of 26 - 35 years, accounting for 63.3% of the cases. However, the differences among age groups were statistically insignificant, as shown in Table 2.
| Variables | Age Groups | Total | P-Value | |||
|---|---|---|---|---|---|---|
| ≤ 25 | 26 - 35 | 36 - 45 | ≥ 46 | |||
| HPV | 0.21 | |||||
| Negative | 12 (40) | 22 (36.7) | 27 (50) | 10 (62.5) | 71 (44.4) | |
| Positive | 18 (60) | 38 (63.3) | 27 (50) | 6 (37.5) | 89 (55.6) | |
| Total | 30 (18.8) | 60 (37.5) | 54 (33.8) | 16 (10) | 160 (100) | |
Distribution of Human Papillomavirus Infection According to Women's Age a
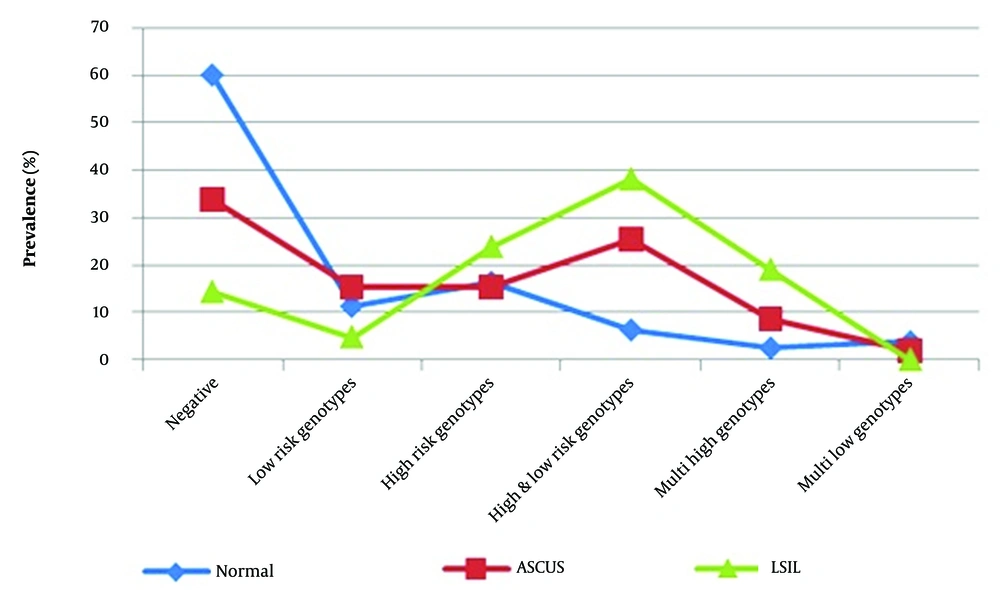
The most common type of HPV infection in women with abnormal cytology was a multi-infection of high- and low-risk genotypes (Figure 1). In women with abnormal cervical cytology, 57.5% were positive for the high-risk HPV genotype, and 28.7% showed multi-infection of high- and low-risk genotypes (Table 3).
| Variables | Cervical Cytology Findings | Total | P-Value | |
|---|---|---|---|---|
| Normal (NILM) | Abnormal (ASCUS - LSIL) | |||
| HPV test results | < 0.001 | |||
| Negative | 48 (60) | 23 (28.7) | 71 (44.4) | |
| Low-risk genotype | 9 (11.3) | 10 (12.5) | 19 (11.9) | |
| High-risk genotype | 13 (16.3) | 14 (17.5) | 27 (16.9) | |
| Multi-infection of high & low-risk genotypes | 5 (6.3) | 23 (28.7) | 28 (17.5) | |
| Multi-infection of high genotypes | 2 (2.5) | 9 (11.3) | 11 (6.9) | |
| Multi-infection of low genotypes | 3 (3.8) | 1 (1.3) | 4 (2.5) | |
| Total | 80 (100) | 80 (100) | 160 (100) | |
Cervical Cytology Findings According to Human Papillomavirus Test Results a
The most prevalent HPV genotypes among all participants were as follows: HPV6 (13%), HPV16 and HPV39 (9.4%), and HPV52 (6.9%). Among women with abnormal cytology (ASCUS and LSIL), the most widespread HPV genotypes were HPV6 (25%), HPV39 (18.8%), HPV16 (16.3%), and both HPV35 and HPV56 (10%). In the ASCUS group, the most common HPV genotypes were HPV6 and HPV39 (16.9%), followed by HPV56 (10.2%). Among patients with LSIL cytology results, the most frequent HPV genotypes were HPV6 and HPV16 (28.6%), HPV39 (23.8%), and HPV52, 73, 67, and 91 (14.3%). The most prevalent HPV genotypes in women with normal cytology were HPV6 and HPV52 (6.3%), and HPV53 (5%).
Multiple HPV infections were found in 26.9% of all participants. Specifically, 41.3% of women with abnormal cytology and 12.6% of women with normal cytology had multiple infections. The highest prevalence of ASCUS among HPV-positive women was in the age group of 26 - 35 (53.8%), while the highest prevalence of LSIL among HPV-positive women was in the age group of 36 - 45 (50%).
5. Discussion
Our results show a high prevalence of HPV infection (71.3%) in WMCA, including ASC-US and LSIL, with a significant increase in HPV infection prevalence from negative for squamous intraepithelial lesion or malignancy (NILM) to LSIL. In line with our findings, a meta-analysis study in the Eastern Mediterranean region revealed that HPV prevalence increased from ASCUS to LSIL and more severe cytology (12). In the current study, the prevalence of high-risk HPV genotypes is high in WMCA. Among all participants, the most prevalent HPV genotype was HPV6, followed by HPV16 and HPV39. Another study from our region reported HPV6, 11, 51, and 16 as the most frequent HPV genotypes in women referred to medical laboratories (13).
Furthermore, our results demonstrated that HPV6 was a more frequent genotype in women with both normal and abnormal cervical cytology. In women with normal cervical cytology, HPV6 was followed by HPV52 and HPV53; in ASCUS cases, it was followed by HPV39 and HPV56; and in LSIL cases, it was followed by HPV16 and HPV39. Research in Mashhad in 2018 revealed high-risk HPV infection in 36% of women with normal cervical cytology, 32% of ASCUS cases, and 32% of patients with LSIL (14). The results of another study in Karaj demonstrated that the overall HPV prevalence among Iranian women was 39.96%, with 7.2% having both HR-HPV and LR-HPV genotypes. Furthermore, it showed that 41.3% of individuals with HR-HPV positive had normal cytology (15). Another study in northern Iran found HPV6, 11, 16, 51, 58, and 59 as the most common genotypes in women with ASCUS (16). The most frequent HPV genotype in another study from southern Iran in women with abnormal cytology was HPV6, followed by HPV39, 66, 31, 18, 45, and 51 (17). A meta-analysis study in China revealed that the most common genotypes in cervical intraepithelial neoplasia were HPV16, HPV52, and HPV58 (18). Research in the United States revealed that the most common high-risk genotype in women with ASCUS was HPV52 (3.3%), and the most prevalent high-risk genotypes in LSIL cases were HPV51 (10.5%) and HPV39 (9.1%) (19). A study on Canadian women with ASCUS or more severe cytology showed that HPV16, 31, 18, and 51 were the most common genotypes (20).
Our results showed that multiple high-risk HPV genotype infections increased from NILM 2.5% to LSIL 19%. These results are consistent with another study that revealed that women with more severe cytology were more likely to carry multiple HPV genotypes (19). The detection technique in this study was based on reverse hybridization, and different studies have demonstrated varying sensitivity and specificity of techniques. For example, one study revealed that reverse hybridization has a higher rate of hr-HPV type identification compared to next-generation sequencing (NGS) (21).
The results of the present study show that HPV is more prevalent in younger people, possibly due to more sexual opportunities, and the consumption of alcohol and tobacco (22). Additionally, younger adolescents generally tend to have lower awareness compared to older ones (23).
5.1. Conclusions
According to the detection of high-risk HPV genotypes in both WMCA and WNC groups in the current study, it seems that the HPV test should be conducted alongside the Pap test for cervical cancer screening. This combined approach is essential to detect HPV-positive women with normal cervical cytology or minor cervical cytological abnormalities that could potentially lead to cervical cancer, especially in women with high-risk HPV genotypes.
5.2. Limitations
The limitations of our study include the small sample size. More research with a larger sample size in a specific population with abnormal cervical cytology is needed to validate these findings.