1. Background
Multiple sclerosis (MS) is the leading cause of non-traumatic neurologic disability to affect young adults in many countries. The global prevalence of 33 per 100,000 for MS was estimated in 2013, while the prevalence was 30 per 100,000 in 2008, suggesting an increasing trend for the disease (1). A meta-analysis in 2019 reported a prevalence rate of 29.3 per 100,000 for MS in Iran (2). Although the clinical spectrum of MS is diverse, the majority of MS cases are classified as relapsing-remitting, where acute attacks or relapses are followed by partial or full periods of recovery (remission) (3).
MS and its complications can jeopardize the mental health of the patients with MS. Therefore, psychological disturbances such as depression, stress, and anxiety in these patients are anticipatable (4, 5). In line with, subjective well-being, as a buffer against mental health problems, has been frequently addressed in patients with chronic conditions such as MS (6, 7). Subjective well-being (SWB) refers to an individual’s evaluation of his/her life. An evaluation of this type is both cognitive and affective. The cognitive component of SWB denotes the global judgment one makes of his/her life (i.e., life satisfaction), while the affective component refers to one’s experience of many pleasant emotions and moods (namely, positive affect) and few unpleasant emotions and moods (namely, negative affect) (8).
A substantial number of patients with MS experience low levels of subjective well-being. MS-related symptoms and signs are considered as contributors to decreased SWB among patients with MS (7). Thus, it is expected that an improvement of self-management skills can lead to an enhanced SWB by enabling patients to better control of these signs and symptoms. It has been shown that self-management training for patients with chronic conditions, including Parkinson’s disease and epilepsy, has led to improved SWB (9, 10).
Self-management is described as the ability of active and responsible individuals to live with the medical, role, and emotional consequences of their chronic condition within their social network in collaboration with healthcare providers (11). Self-management interventions can be categorized into two broad groups: peer-led self-management interventions and nurse-led self-management interventions. In peer-led interventions, the peer leader has conditions similar to those of other patients within a group and is expected to provide relevant and meaningful information, act as a role model, and guide the peers (12, 13). However, in nurse-led self-management interventions, a nurse presents a set of pre-designed educational materials.
Both self-management mentioned above interventions have shown promising results, including increased improved quality of life, decreased depression, and enhanced psychological well-being in patients with chronic conditions (14-16). Nevertheless, there is no research, as yet, to investigate the effects of these two methods on SWB of patients with MS.
2. Objectives
Therefore, the current study was designed with two aims: (1) to examine whether peer-led and nurse-led self-management training can improve SWB of patients with MS and (2) to compare the effect of these two interventions on SWB of patients with MS.
3. Methods
This randomized clinical trial was conducted at the Comprehensive Center for the Treatment of Special Diseases affiliated to Birjand University of Medical Sciences (BUMS) in 2018.
Taking a type I error = 0.05 and a type II error of 0.2, and considering the results of previous research (17) (M1 = 215.77, M2 = 232.57, S1 = 25.55, and S2 = 25.62), the desired sample size was calculated as 37 subjects per group. An attrition rate of 15% was factored, whereby the sample size increased to 42 subjects per group.
Potential patients were approached during their usual clinic visits at the Comprehensive Center for the Treatment of Special Diseases. Patients were eligible if they had the inclusion criteria, i.e., ability to read and write in Persian; willingness to participate in the study; age between 20 to 45 years; a minimum one-year history of MS confirmed by the neurologist; high likelihood of continuing to present MS clinically as remitting-relapsing during the study period based on the neurologist’s opinion; obtaining a score between 0 and 5.5 on the Expanded Disability Status Scale (EDSS); and lack of any acute or chronic physical, mental, and psychiatric disorders that interfere with self-management. Failing to attend more than two sessions, being hospitalized during the intervention, or unwillingness to continue participation were considered as exclusion criteria.
The study was explained to eligible patients, and written informed consent forms were signed by the interested patients.
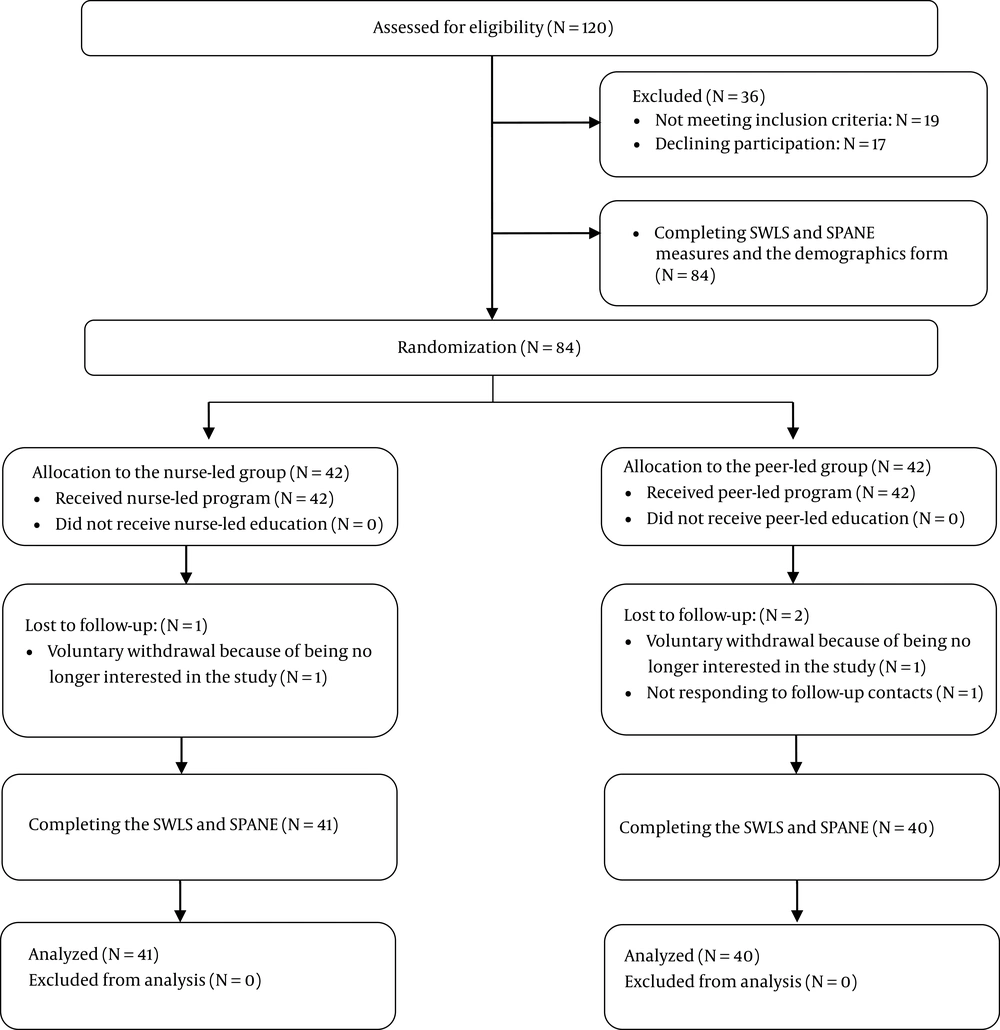
Initially, 120 patients were assessed for eligibility of whom 84 were selected. A demographics form, the Satisfaction with Life Scale (SWLS), and the Scale for Positive and Negative Experience (SPANE) were completed for all the participants by a researcher assistant. The participants were subsequently assigned to the study groups via simple randomization using computer-generated random numbers. For this purpose, 84 selected participants were assigned a number from 1 to 84 of which a list of 42 random numbers was created. The participants with these random numbers were allocated to the peer-led group, and the other participants were assigned to the nurse-led group (Figure 1). Recruitment was performed from March to May 2018.
3.1. Intervention
In the nursing-led group, the patients were divided into two sub-groups of 10 and two sub-groups of 11 members. Afterward, the prepared self-management contents (Table 1) were presented by the same experienced nurse in six sessions, each lasted for about 1.5 hours held every week. The self-management intervention contents were prepared using credible sources, including books (18-20) and a valid website (21), and were subsequently confirmed by two neurologists independently.
| Session | Detail |
|---|---|
| Session 1 | Familiarity of the researchers with the participants and the participants with each other, gaining the trust of the participants, determining the roles and responsibilities of the participants and researchers, overviewing self-management and its techniques |
| Session 2 | Overviewing MS, its course, and therapeutic options; introducing self-management strategies for MS-induced fatigue |
| Session 3 | Providing self-management strategies for establishing a balance between activities and rest |
| Session 4 | Providing self-management strategies for managing ataxia in MS |
| Session 5 | Providing self-management strategies for stress, anxiety, and depression |
| Session 6 | Providing self-management advice on nutrition, summarizing the sessions, clarifying potential ambiguities raised by the participants, completing research instruments |
In the peer-led group, the leader was selected according to the following criteria: willingness to play the assigned tasks, acceptable social communication skills, ability to manage the sessions, a minimum five-year history of MS, and a proper educational level (Bachelor’s degree or above). Considering these criteria and according to the neurologist’s suggestion, a patient from among the MS patients referring to the Comprehensive Center for the Treatment of Special Diseases was appointed as the leader of the group.
Three training sessions were held for the leader, comprising of the following issues: an introduction to the objectives and nature of the peer education sessions, essential points to communicate with group members, useful strategies to help keep the discussion focused on the presented topics, and a brief review of the prepared contents. These sessions were held in the presence of the two researchers under the supervision of the neurologist.
In the next step, the participants in the peer-led group also were divided into two sub-groups of 10 and two sub-groups of 11 members. The prepared self-management contents (Table 1) were presented by the peer leader for each group through six weekly-held sessions, each lasting for approximately 1.5 hours.
In both the nurse-led and peer-led groups, participants were assigned into sub-groups to have maximum homogeneity in terms of educational level. Also, one of the researchers was present as a supervisor in both groups. Both interventions were conducted over a period of 6 weeks during the months from July to August 2018.
From the second week up to two months after the intervention completed, a weekly telephone follow-up was conducted on the implementation of the self-management practice. At the end of the sessions, the provided contents were available to all of the patients.
Patients registered at the Comprehensive Center for the Treatment of Special Diseases usually attended the center individually. In order to reduce the contact between participants and minimize the potential contamination effects, the peer-led intervention was conducted in the morning on Saturdays through Tuesdays. For participants in the four nurse-led groups, the intervention was implemented on the same days, yet in the evening. Thus, contamination effects can be assumed to be negligible.
The study scales were completed for the participants in the two groups both immediately and two months after the intervention by the same researcher assistant who completed the scales at baseline.
3.2. Study Measurements
The participants’ demographic characteristics, including age, gender, marital status, educational status, occupation, insurance type, and MS duration, were collected using a demographics form.
The EDSS was completed by the neurologist to evaluate the degree of the participants’ disability. This instrument is on an ordinal scale ranging from 0 indicating normal neurological status to 10, indicating death due to MS. It provides a final score, which reflects the eight functional system scores (i.e., pyramidal, cerebellar, brain stem, sensory, bowel/bladder, visual, cerebral and others) (22).
The cognitive component of SWB (i.e., life satisfaction) was assessed using the SWLS, a five-item self-report measure that assesses one’s satisfaction with life and accomplishments of essential goals in life. The participants were asked to respond to items on a 7-point Likert scale ranging from 1 = strongly disagree to 7 = strongly agree. The total score of SWLS ranges from 5 to 35 (23). Previous research on patients with MS has reported a desirable reliability coefficient for the SWLS, with a Cronbach’s alpha of 0.84 (7). In Iran, several studies have shown good reliability coefficients for this scale (24). In the present study, the alpha coefficient for the SWLS was 0.82.
The affective component of SWB was measured by SPANE. This scale is divided into two subscales. One sub-scale assesses positive feelings (SPANE-P), and the other assesses negative feelings (SPANE-N). Each sub-scale contains six items that are scored on a five-point scale ranging from 1 (very rarely or never) to 5 (very often or always). The SPANE-P and SPANE-N scores are the sum of the scores given to their respective six items, and the scores can range from 6 to 30. This study used the Persian version of SPANE, which is available on the official website of Dr. Diener, the original developer of this tool. In previous research, this scale had acceptable reliability (25). Regarding reliability, the Cronbach’s alpha coefficients were 0.8 and 0.9 for the SPANE-P and SPANE-N sub-scales, respectively.
3.3. Ethical Consideration
The present study was approved by the Ethics Committee of Birjand University of Medical Sciences (BUMS) (code: Ir.bums.REC.1397.190). Also, the researchers obtained permission from BUMS and received a clinical trial code (IRCT20190305042926N1) before the eligibility of the patients with MS registered in the center was assessed.
3.4. Data Analysis
The collected data were analyzed with SPSS v.16 software (IBM Company, New York, USA). The descriptive statistics, including mean, standard deviation, and frequency, were used to describe the participants’ demographic characteristics and their responses on study measures.
The data concerning gender, marital status, educational level, occupation, and insurance type were compared between the two groups using the chi-square test or Fisher’s exact test. The independent t-test was applied to analyze the difference between the two groups in terms of age and the duration of MS. The EDSS scores were compared using the Mann-Whitney U test.
There was a non-normal distribution of life satisfaction mean scores in the peer-led group before the intervention and in the nurse-led group immediately after the intervention. In the nurse-led group, also, the negative experience mean scores before the intervention, and two months after the intervention were non-normally distributed (Shapiro-Wilk test, P < 0.05). The main variables in other time points were normally distributed.
In both groups, life satisfaction mean scores over time were evaluated using the Friedman test with post hoc Wilcoxon signed-rank test. The Mann-Whitney test was employed to do between-group comparisons.
Positive experience mean scores were compared between the two groups over time using repeated-measures ANOVA followed by post hoc Bonferroni correction.
In the nurse-led group, the mean score of negative experience over time was assessed using the Friedman test with post hoc Wilcoxon signed-rank test. In the peer-led group, a repeated-measures ANOVA followed by post hoc Bonferroni correction was used to compare within-group changes of negative experience over time. Finally, between-group comparisons were performed with the independent t-test or Mann-Whitney test.
4. Results
A total of 81 patients with MS participated in this study. The age means of the patients in the peer-led, and nurse-led self-management education groups were 37.7 (95% CI: 34.89 - 39.51) and 35.61 (95% CI: 32.71 - 38.51) years, respectively. There was no significant difference in the mean age between the two groups (P = 0.39). The EDSS mean scores of the peer-led and nurse-led groups were 2.35 (95% CI: 1.99 - 2.7) and 2.36 (95% CI: 1.98 - 2.75), respectively, with no significant difference according to the Mann-Whitney U test (P = 0.95). As shown in Table 2, the differences between the two groups did not reach statistical significance concerning other demographic characteristics.
| Characteristic | Peer-Led Group (N = 40) | Nurse-Led Group (N = 41) | P Value |
|---|---|---|---|
| Gender (%) | 0.82a | ||
| Male | 8 (20) | 9 (21.95) | |
| Female | 32 (80) | 32 (78.05) | |
| Marital status (%) | 0.08a | ||
| Single | 4 (10) | 10 (24.4) | |
| Married | 36 (90) | 31 (75.6) | |
| Educational status (%) | 0.6a | ||
| Primary and secondary school | 11 (27.5) | 9 (22) | |
| High school | 12 (30) | 10 (24.4) | |
| University | 17 (42.5) | 22 (53.7) | |
| Occupation (%) | 0.24b | ||
| Housewife | 23 (57.5) | 16 (39) | |
| Retired | 1 (2.5) | 2 (4.9) | |
| Unemployed | 5 (12.5) | 9 (22) | |
| Self-employed | 0 (0) | 3 (7.3) | |
| Employee | 11 (27.5) | 11 (26.8) | |
| Duration of MS (years) | 5.67 (95% CI: 4.54 - 6.8) | 6.75 (95% CI: 5.3 - 8.2) | 0.24c |
| Insurance type (%) | 0.15b | ||
| Social welfare | 17 (42.5) | 25 (61) | |
| Armed forces | 4 (10) | 1 (2.4) | |
| Health and medical service | 19 (47.5) | 15 (36.6) |
aThe chi-square test
bThe Fisher’s exact test
cThe independent t test
Before the intervention, there was no significant difference in the mean scores of life satisfaction, positive experience, and negative experience between the two groups (P > 0.05) (Table 3).
| Variable | Peer-Led Group (N = 40) | Nurse-Led Group (N = 41) | z or t Values | P Value |
|---|---|---|---|---|
| Life satisfaction [Mean (95% CI)] | ||||
| Before intervention | 18.55 (16.83 - 20.26) | 16.87 (14.87 - 18.88) | -1.5 | 0.13a |
| Immediately after intervention | 21.2 (18.88 - 23.51) | 18.58 (17.05 - 20.12) | -1.89 | 0.06a |
| Two months after intervention | 22.22 (20.1 - 24.34) | 19.85 (18.48 - 21.22) | 1.9 | 0.06b |
| Positive experience [Mean (95% CI)] | ||||
| Before intervention | 16.5 (14.96 - 18.03) | 14.75 (13.82 - 15.68) | 1.96 | 0.54b |
| Immediately after intervention | 19.82 (18.37 - 21.27) | 15.8 (14.87 - 16.7) | 4.72 | <0.001b |
| Two months after intervention | 19.77 (18.54 - 21.00) | 16.36 (15.54 - 17.19) | 4.64 | <0.001b |
| Negative experience [Mean (95% CI)] | ||||
| Before intervention | 17.05 (15.79 - 18.3) | 16.68 (15.55 - 17.8) | -0.13 | 0.89a |
| Immediately after intervention | 15.1(13.88 - 16.31) | 15.04 (14.04 - 16.05) | 0.06 | 0.94b |
| Two months after intervention | 14.2 (13.1 - 15.29) | 13.8 (12.89 - 14.71) | -0.3 | 0.75a |
aMann-Whitney U test
bIndependent t-test
As expressed in Table 4, the Friedman test revealed a significant increase in the scores of life satisfaction in both groups in the course of time (P < 0.001). The Wilcoxon signed-rank test showed that in both groups, life satisfaction increased significantly over time from before intervention to two months after intervention (P < 0.05). However, between-group comparisons showed no significant differences between the two groups in terms of life satisfaction mean scores at the three-time points (P > 0.05).
| Time | Peer-led Group, (N = 40), Mean (95% CI) | Nurse-Led Group, (N = 41), Mean (95% CI) | Test Resultsa |
|---|---|---|---|
| Before intervention | 18.55 (16.83 - 20.26) | 16.87 (14.87 - 18.88) | 0.13a |
| Immediately after intervention | 21.2 (18.88 - 23.51) | 18.58 (17.05 - 20.12) | 0.06a |
| Two months after intervention | 22.22 (20.1 - 24.34) | 19.85 (18.48 - 21.22) | 0.06b |
| Test resultsc | χ2 = 39.96; P < 0.001 | χ2 = 23.52; P < 0.001 | - |
aMann-Whitney U test
bIndependent t-test
cFriedman test
A repeated-measures ANOVA showed that positive experience mean scores were different between groups (F = 3.33, P < 0.001) and within groups at different time points (F = 3.24, P < 0.001). Furthermore, a significant time × group interaction was found (P = 0.01), indicating that increases in positive experience over time in the peer-led group were significantly greater than those for the nurse-led group (Table 5). In both groups, the participants reported a significantly higher positive experience immediately and two months after the intervention compared to before intervention (P < 0.05). Also, positive experience in the two groups increased from immediately after the intervention to two months after the intervention; however, the change was not significant (P > 0.05).
| Variable | Source | F Value | P Value |
|---|---|---|---|
| Positive experience | Group | 3.33 | < 0.001 |
| Time | 33.24 | < 0.001 | |
| Group × Time | 0.69 | 0.01 |
A significant decrease was found in the mean score of negative experience in the nurse-led group over time (χ2 = 44.27; P < 0.001). The Wilcoxon signed-rank test indicated that negative experience decreased significantly from before the intervention to two months after intervention (P < 0.05). The repeated measures ANOVA determined that the mean score of negative experience in the peer-led group also decreased significantly over time (F (2, 78) = 30.85, P < 0.001). Post hoc tests using the Bonferroni correction revealed a significant decrease in negative experience from before intervention to immediately after the intervention as well as from before the intervention to two months after the intervention (P < 0.001). A reduction was also found in negative experience from immediately after the intervention to two months after the intervention; however, it was not significant (P = 0.06).
The results of between-group comparisons with respect to negative experience revealed no significant differences before the intervention, immediately after the intervention, and two months after the intervention (P > 0.05).
5. Discussion
The purpose of the current study was to compare the effect of a peer-led versus a nurse-led self-management intervention on SWB in patients with MS.
In this study, both peer-led and nurse-led self-management interventions resulted in a significant improvement of the cognitive component of subjective well-being, i.e., life satisfaction. Previous studies have proved the effect of self-management on the participants’ life satisfaction. Sahar et al. (26), for example, reported that implementation of a 12-week self-help intervention for a sample of older people in Jakarta led to significantly higher life satisfaction in the intervention group than the control group (27). In other research, 60 Iranian patients with epilepsy participated in a four-session self-management training program. One month after the intervention, the mean scores of life satisfaction and its dimensions (including mental health, social functioning, worry about seizures, energy-fatigue, cognitive functioning, and medication effects) in the intervention group were significantly higher than in the control group (11). However, in Abbasi et al. (27) study, a self-management education program consisting of three sessions and a three-month follow-up for 60 people with chronic heart failure (CHF) did not result in a significant difference in the life satisfaction of intervention and control groups (28). These findings collectively suggest that the impact of self-management interventions on an individuals’ life satisfaction may be informed by factors such as the disease nature and disease-related difficulties. In this line, in Ryan et al. (7) study, disease severity was a predictor for life satisfaction in patients with MS (8).
The impact of the self-management interventions in enhancing life satisfaction may be partially attributed to the potential of these interventions in improving patients’ capacity to manage MS signs and symptoms more appropriately, which could have led to an improved feeling of health. Such feeling, in turn, can lead to higher life satisfaction. The Common-Sense Model of Self-Regulation (29) can help explain this finding. According to this model, when people face threats to their health, they create mental representations (beliefs) of illness threats. An individual’s beliefs concerning illness threats include issues such as the disease identity, cause, controllability, duration/timeline, and consequences. Patients’ beliefs about these five dimensions influence their bio-psycho-social adjustment (29, 30). In a meta-analysis of studies adopting the Common-Sense Model of Self-Regulation, Hagger et al. (28) found that illness presentations had a direct effect on disease outcomes such as patient’s well-being (29).
The results of this study showed that there was no significant difference between the two groups over time, despite the improvement in life satisfaction. The two interventions may have in-built advantages of one over the other. For example, the possible empathy created among the participants of the peer-led group cab be an advantage (31, 32). The nurse-led intervention, on the other hand, is characterized by a more robust and structured education. Nevertheless, these advantages did not result in a significant difference between the two groups with respect to life satisfaction.
The results also indicated that the affective component of subjective well-being, i.e., positive experience and negative experience, improved significantly over time in both groups. Alongside this, Benzo et al. (32) reported a significant positive correlation between self-management ability and positive affect and a significantly negative relationship between self-management ability and negative affect in patients with chronic obstructive pulmonary disease (COPD) (33). Based on the Common-Sense Model of Self-Regulation, researchers deduce that in patients with chronic diseases, factors such as a stronger illness identity and the perception that MS has substantial adverse effects on an individual’s emotions are key predictors of psychological distress. Conversely, the more a patient feels that she/he understands the illness and can take actions to control it, the lower her/his distress will be.
In this study, positive experience in the peer-led group improved better than in the nurse-led group over time. This finding may be related to the peer-led group’s benefits, such as the sense of empathy created between the peer leader and the members and, hence, the more intimate relationship established with him/her (31, 32). This can lead to a stronger social network and thus provide more effective social support, including more emotional support among peer-group members compared with the nurse-led group.
Notably, in the two groups, positive experience increased from immediately to two months after the intervention; however, it was not significant. In the peer-led group, also, the improvement of negative experience from immediately to two months after the intervention was not significant. Therefore, there is a need for measures to strengthen the long-term impact of the intervention. One potential way may be to extend the intervention period. To sustain the changes, it may also be helpful to hold monthly booster meetings after the six weekly training sessions.
To the best of our knowledge, this is the first study to examine the effect of peer-led versus nurse-led self-management on SWB of patients with MS. In the current research, interventions were delivered in a real-world setting by a usual provider or lay peer educator. Furthermore, as evidenced by the low rate of attrition and the high rate of session attendance, the interventions were acceptable and meaningful to patients. Thus, despite the relatively small changes in the mean scores of the main variables from baseline to the follow-up phase, these changes can be assumed as clinically beneficial.
This study has some implications for patients with MS, health care providers, and clinical managers. First of all, the importance of self-management should be emphasized to patients with relapsing-remitting MS. Also, if healthcare providers are to improve the SWB of these patients, the self-management intervention led by peers can be a useful tool. Finally, clinical managers need to support healthcare professionals who are interested in peer-led self-management interventions.
However, the study has a few limitations that pose caution in generalizing the results to other MS populations. First, the participants comprised only of patients with MS of the relapsing-remitting type. Secondly, the sample was selected from a single treatment center. Future studies can be designed to examine the impact of these two self-management approaches on other psychological factors such as psychological well-being and the level of hope in patients with MS.
5.1. Conclusion
Peer-led and nurse-led self-management training are feasible tools to enhance the cognitive component of SWB, i.e., life satisfaction. Considering the affective component of SWB, positive experience in the peer-led group improved better than in the nurse-led group over time. Therefore, the application of the peer-led self-management program to improve SWB in patients with relapsing-remitting MS is more effective than the nurse-led approach.