1. Context
In late December 2019, a new coronavirus, called COVID-19 (SARS-CoV-2/2019-nCoV), triggered the outbreak of pneumonia from Wuhan (Han’s seafood market) in China, which is now possessing major public health threats to the world (1). The COVID-19 epidemic is spreading around the world and has affected 204 countries, including the USA, Italy, Spain, Germany, France, and Iran since April 3, 2020 (2). According to global statistics, the mortality rate of COVID-19 is 4.3% (3). The symptoms of COVID-19 in the early stages include pneumonia, fever, myalgia, fatigue, diarrhea, and loss of smell and taste (4). Thus far, no vaccine or useful antiviral drug has been clinically confirmed against COVID-19 infection, although a few clinical studies have been completed, and a huge number of trials have begun or are ongoing (5). Therefore, the general public should observe infection prevention and control measures and hygienic principles, such as using safety and protection protocols and equipment, as crucial priorities.
The objective of this review was to describe the epidemiology of COVID-19 in different chronic diseases and understand the pathophysiological mechanisms by which the virus can lead to the progression of these diseases.
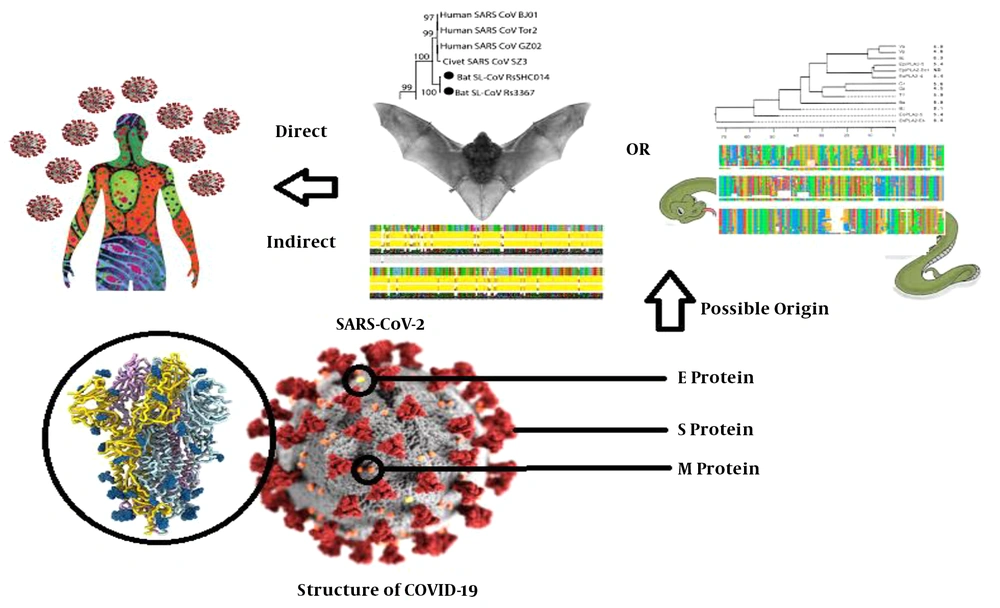
2. Structure and Origin of SARS-CoV-2/2019-nCoV
As known, SARS-CoV-2/2019-nCoV is a non-segmented, positive-sense, single-stranded RNA virus of animal origin with the genome size of about 26 - 36 kb (6). Approximately 30 coronavirus species have been identified in humans, mammals, and birds. Coronaviruses are among the most common viruses, which their antibodies are found in 30% to 60% of the Chinese population (7). Epidemiological studies of primary cases of COVID-19-related pneumonia show that many cases were exposed to the Huanan wholesale seafood market in Wuhan, China (8). Based on a study by Ji et al. (9), SARS-CoV-2 falls between bat coronavirus and coronavirus of unknown origin. A study by Benvenuto et al. (10) showed that SARS-CoV-2 is closely related to the coronavirus isolated from a particular species of Chinese bat. Chan et al. (11) confirmed that SARS-CoV-2 is closely related to SARS-CoV from the bat. Thus, COVID-19 may have originated from the bat, transmitted to humans through an intermediate host (Figure 1).
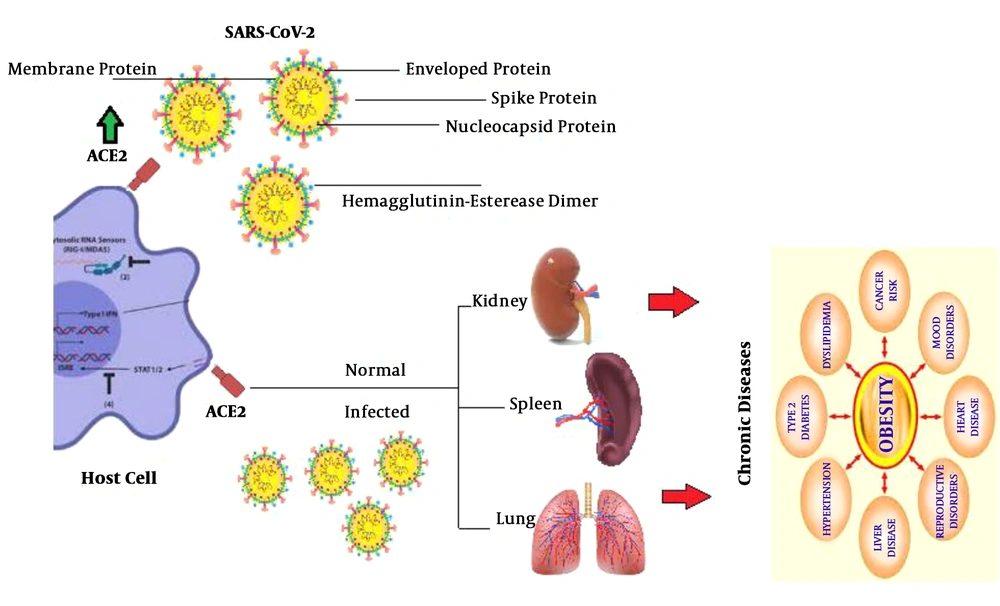
3. SARS-CoV-2/2019-nCoV Pathogenesis Mechanism and Use of Receptors
It is reported that ACE2 is the possible receptor for SARS-CoV-2/2019-nCoV. Two types of this receptor exist in the human lung (12, 13). Asians have higher ACE2 levels in their alveolar cells than white people and Afro-American populations. The binding of SARS-CoV-2/2019-nCoV to ACE2 increases its expression and can lead to alveolar cell damage (14). Damage to alveolar cells can, in turn, cause a series of systemic reactions, leading to a chronic condition in various organs of the human body and even death (Figure 2). The prerequisite for a COVID-19 attack on a host cell is its binding to the host cellular receptor.
4. COVID-19 Related Comorbidities
The studies of patients with COVID-19 infection have shown that people with underlying diseases not only have a higher risk of developing the disease but also are more likely to die from the virus infection (Table 1) (15). Another factor influencing the mortality rate of COVID-19 is the old age, especially over 60. Still, the World Health Organization (WHO) emphasizes that young people are not safe, and they must also follow health principles to prevent the spread of the virus (16). People with diabetes can help control their immune systems by controlling their blood sugar and prevent COVID-19 as much as possible.
| Author/Reference | Disease | Study Design | Number of Confirmed COVID-19 | Target Group | Outcomes | Main Findings |
|---|---|---|---|---|---|---|
| CDC COVID-19 response team (17) | Mixed | Cross-sectional | 571,678 | Adults | Prevalence of underlying health conditions | The most commonly reported conditions were diabetes mellitus, chronic lung disease, and cardiovascular disease |
| He et al. (18) | Mixed | Retrospective | 54 | Adults | Prevalence of underlying health conditions | The most commonly reported conditions were hypertension, diabetes, coronary heart disease, and previous cerebral infarction |
| Rogers et al. (19) | Diabetes | Special communication | - | - | - | Keeping patients safe, functional, and at home during pandemics |
| Chen et al. (20) | Cardiovascular diseases | Cross-sectional | 150 | Adults | Myocardial injury | COVID-19 can lead to myocardial injury |
| Guo et al. (21) | Diabetes | Cross-sectional | 174 | Adults | Symptoms, laboratory findings, chest computed tomography (CT), and treatment | Diabetes should be considered a risk factor for COVID-19 |
| Li et al. (22) | Cardiovascular diseases | Meta-analysis | 1527 | Adults | Association | Previous cardiovascular metabolic diseases lead to a greater risk of COVID-19 |
| Muniyappa and Gubbi (23) | Diabetes | Perspective | - | - | Potential mechanisms by which diabetes interacts with COVID-19 |
Effect of COVID-19 Infection on Underlying Health Conditions
5. Diabetes
High blood sugar levels can damage a person's immune system. The weaker the body’s immune system, the lower the ability to fight infections, such as COVID-19; thus, the virus can cause more damage to the body (24). People living with diabetes, like everyone else in the community, need to take precautions against the COVID-19 disease. They should also be more careful about controlling their blood sugar and avoiding changing their medications without consulting a physician. Some vitamins and minerals play a role in improving the function of the immune system, but the arbitrary and indiscriminate use of supplements containing these micronutrients may cause disorders in the body’s function. Therefore, if a person is not nutrient-deficient, it is better to provide nutrients by food sources and avoid taking supplements without consulting a doctor. Recent studies show that there is no specific way to prevent the immune system from infecting people with the COVID-19, especially people with diabetes (25). In general, relaxation, adequate sleep, and proper nutrition can improve the immune system.
6. Cardiovascular Diseases
Infectious diseases, including viral infections such as COVID-19, are one of the leading causes of cardiovascular disease, which can lead to heart failure with pericarditis, myocarditis, and cardiac conduction (26). It seems that viral diseases, including COVID-19, are responsible for about 5% of the cases of acute heart failure. In addition to new cases of heart disease, COVID-19 infection in patients with a history of cardiovascular problems can change the course of the underlying disease and increase mortality in the patients (27). Patients with cardiovascular disease and over the age of 60, with a history of high blood pressure, obesity with a BMI above 25, and a history of smoking are at a higher risk of COVID-19 infection. Researchers at the Wuhan University of China found that of 416 patients admitted to the hospital, about 20% had severe muscle heart damage due to a severe COVID-19 infection, of whom more than half died (28). The findings show that patients with heart damage have a very high risk of death. One of the researchers' hypotheses is that the immune system reacts to the COVID-19 infection, which, if not controlled, can cause a condition called “cytokine storm” and damage organs (29, 30). Another possibility is that in people with cardiovascular disease, the overall stress caused by the infection can damage the heart muscle. Finally, COVID-19 may attack the heart directly. According to research, the virus binds very strongly to angiotensin converter enzyme 2 (ACE2) receptors. These receptors are expressed not only in the lungs but also in other parts of the body, such as the heart and digestive tract (31). Some hypotheses suggest that common blood pressure medications, such as ACE inhibitors and angiotensin receptor blockers, can be very harmful to people with COVID-19 infection (32). However, another study claimed that RAS inhibitors might be a good therapeutic choice in patients with COVID-19 infection (33). Therefore, it is highly recommended that cardiovascular patients adhere to the principles of prevention, personal hygiene, isolation, social distancing, and regular use of cardiac drugs. Researchers emphasize the importance of preventive measures in the current situation and suggest that people with cardiovascular disease and a history of stroke consider themselves to be at high risk. These patients should not stop taking any of their medications without consulting a doctor.
7. Gastrointestinal Diseases
Dysfunction of other organs is seen in severely ill people but it can also occur in any other serious infection. This damage to organs is not always directly caused by an infection, but can be caused by the body’s reaction to the infection. Epidemiological studies have shown less common symptoms of COVID-19 such as sputum production, headache, bleeding, and some gastrointestinal symptoms (34). Some people with COVID-19 have reported gastrointestinal symptoms such as nausea or diarrhea, although these symptoms are much less common than lung problems. As COVID-19 appears to enter the body more easily through the lungs, they can also enter the intestine. In the past, SARS and MERS were detected in intestinal and fecal samples. New studies have also shown that fecal samples from some people with COVID-19 contain the virus. Research is ongoing on the possibility of transmitting the virus from feces (35-37). Other studies have reported an association between COVID-19 and inflammatory bowel disease (IBD). Turner et al. (38) surveyed 102 PIBD centers using an electronic reporting system of pediatric patients with IBD infected with COVID-19, and reported only eight cases of IBD with COVID-19 infection globally. Other studies revealed that patients with IBD may have no increased risk of COVID-19 infection, which is possibly due to using cytokine blockers to treat these patients (39). Therefore, the possibility of fecal-oral transmission should be considered in COVID-19 infection. According to previous and recent studies, COVID-19 may be associated with gut microbiota through the ACE2 receptor; thus, we speculate that COVID-19 may be related to gut microbiota (40). Therefore, targeting the gut microbiome may be a new potential treatment option for treating COVID-19-related pneumonia. Surprisingly, recent cellular data from two independent groups showed the significant enrichment of ACE2 expression in cholangiocytes (59.7% of cells) instead of liver cells (2.6% of cells), indicating that COVID-19 may cause direct damage to the intrahepatic ducts (41). Overall, we have to work hard to be aware of the early signs of COVID-19 for detection, separation, and intervention in the early stages of the disease. Finally, more attention should be paid to hand hygiene and disinfection and the control of vomiting, feces, etc. We can overcome COVID-19 infection soon with joint efforts and excellent support.
8. Respiratory System Disease
Like other respiratory disease-inducing viruses, such as SARS, MERS, and community-acquired pneumonia (CAP), COVID-19 usually first affects the lungs. Early symptoms include fever, cough, and shortness of breath. These symptoms can appear within two days or up to 14 days after contact with the virus. The COVID-19 severity varies from mild or asymptomatic to severe or sometimes fatal. Older people and those with chronic diseases appear to be at a higher risk of serious symptoms. This variability is also seen in the effect of COVID-19 on the lungs. Some people may have only mild respiratory symptoms while others may develop pneumonia, which does not threaten a person’s life. Some people also suffer from severe lung damage. According to research, what we often see in people who are severely infected with COVID-19 is respiratory distress syndrome (42, 43). These conditions are not caused by the virus alone and can be triggered by a variety of events, including infections, trauma, sepsis, and anemia. These conditions damage the lungs, leading to fluid leakage from small blood vessels in the lungs. While there is a lack of information about the type of damage caused by COVID-19 in the lungs, a new report has shown that similar damage can occur with SARS and MERS (44). A new study of 138 patients admitted to the hospital for COVID-19 found that, on average, people had difficulty in breathing five days after the onset of symptoms. Respiratory distress syndrome also began, on average, eight days after the onset of symptoms (45). The treatment for respiratory distress syndrome involves the use of oxygen and mechanical respiration to absorb more oxygen into the blood. There is no specific treatment for respiratory distress syndrome and medical staff must do their best to support the patient during this process so that the body recovers and the immune system takes care of underlying events.
9. Liver and Kidneys
When liver cells are inflamed or damaged, they can secrete excessive amounts of enzymes into the bloodstream. An increase in liver enzymes is not always a sign of a serious problem, but this laboratory finding has been seen in people with SARS or MERS. New reports showed the signs of liver damage in patients with COVID-19, but it was not clear if the virus or the used drugs to treat the patients induced the damage (46-48). Some people with COVID-19 hospitalization have also had acute kidney damage, which sometimes requires kidney transplantation. The same thing happened with SARS or MERS. However, according to the World Health Organization (WHO), there is little evidence that the virus directly causes kidney damage. Accordingly, kidney damage may be caused by other changes that occur during COVID-19 infection. When a person has pneumonia, less oxygen circulates through the body, which can damage the kidneys.
10. Immune System Disorders
With any infection, the immune system reacts by attacking the virus or external bacteria. While this immune response can help eliminate infection, it can sometimes cause side effects in the body. It can occur in the form of a severe inflammatory reaction, sometimes called the “cytokine storm” (49, 50). Immune cells produce cytokines to fight inflammation, but if too many of them are released, these conditions can cause problems in the body. Many of the damages caused by COVID-19 in the body are caused by a condition called sepsis syndrome, which results from complex immune responses (51). The infection itself can cause an acute inflammatory reaction in the body, and such conditions can affect the functioning of various organs. Another thing about the immune system is that so far there have been almost no cases of COVID-19 in children under nine years of age. Researchers are not sure if children get the infection or if they have mild symptoms that no one notices. In other types of infections, including measles and pneumococcal infections, children experience less severe symptoms than adults do. This may be because children have a direct immune response while older people can sometimes experience an over-immune response (52, 53). An over-immune reaction may cause some damage during infections. This was evidenced during the outbreak of SARS, which may be true of COVID-19 infection.
11. Conclusions
The prevalence of COVID-19 infection has become a clinical threat to the general population and healthcare staff around the world. However, knowledge about this new virus is limited. Effective antiviral therapy and vaccination are currently being evaluated and under-development. What we can do now is the aggressive implementation of infection control measures to prevent the human-human transmission of SARS-CoV-2. Public health services should also monitor the situation. The more the knowledge about this new virus and its prevalence, the better the ability of us to deal with it. It is hoped that we will overcome COVID-19 soon with the discovery of effective vaccines, drugs, and treatments.