1. Context
The Coronavirus Disease 2019 (COVID-19) epidemic is known as a global health crisis that has caused huge mental and health challenges in the world (1). Initially, COVID-19 was reported in China in late 2019 and then spread to 13 countries by January 24, 2020 (2). This disease that occurred first in Wuhan is an emerging infectious disease (3). In Iran, there was a growing trend of the disease showing that until March 1, 2020, there were 987 infected people and 54 deaths (4). By mid-May, the prevalence rate raised to 112,725 infected cases and 6,783 deaths. Turkey is another Islamic country with the highest rate of COVID-19-infected cases, reporting 143,114 infected people, and 3,925 deaths (5) In addition to endangering human health, COVID-19 imposes irreversible psychological impacts on human societies. Among these influences, we can mention the effects of quarantine and lockdown, the fear of infection, the anxiety of losing loved ones, and depression arising after losing friends and family members (6).
In the current global situation that the number of COVID-19 deaths is updated and published daily, spirituality can be a good sedative in societies facing the outbreak (7). Several religions, despite all their limitations, create positive emotions in people. Spirituality and religion can help humans in bereavement and times of crisis (8). Although, for a long time, epidemiologists have been trying to answer this question that whether spirituality and religion are associated with mortality and health (9), the majority of the internal medicine specialists have positive attitudes towards spirituality (10). The study of dialogues between religion and psychology is difficult because experts in psychology often lack a strong understanding of religious traditions, and it requires to understand basic problems and materials to connect religion with psychology (11). Various longitudinal and cross-sectional studies carried out around the world support the theory of the correlation between spirituality and better physical and mental health (12-14). Religions have positive impacts on human mental health through conducting health measures, providing social support, and enhancing self-efficacy and cohesion (15). As an instance, “If you hear that plague or any other dangerous infectious disease has broken out in a land, do not go to it; but if it breaks out in a land where you are living, stay at home in your city”, said the Prophet of Islam nearly 1,400 years ago (16). “Cleanliness is half of the faith and faith leads a man to heaven”, said the Prophet of Islam in another part (17). Furthermore, ablution (wudhu’) is one of the Islamic washing rituals performed before each prayer, five times a day, by doing which a person washes his hands, forearms, mouth, nose, ears, face, hair, ankles, and feet, three times each (17). Thus, it includes all of the most effective ways of dealing with COVID-19. Islam is the main religion in Iran (18) that allowed Iranian families to pray together and spend more time to read the Holy Quran during the COVID pandemic. Research has shown that religious practices are associated with many health consequences (19, 20). Spirituality and religion can be useful sedatives for humankind in the current status quo. Accordingly, the present study was conducted to review the benefits of religion and spirituality in times of crisis.
2. Evidence Acquisition
The present study is a review of the literature published from 1978 to 2019. The search was done in electronic databases and reputable websites including PubMed, Medline, Springer, Elsevier, Science Direct, Scopus, and SID for both English and non-English language articles using the following keywords: “spirituality”, “prayer”, “and “some religious advice were assessed in times of crisis”.
3. Results
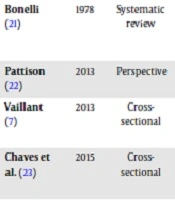
A total of 11 articles were selected for review (Table 1).
| Author (Reference) | Year | Study Design | Outcomes |
|---|---|---|---|
| Bonelli (21) | 1978 | Systematic review | In more than 70% of the studies, there was a strong relationship between religious involvement and better mental health |
| Pattison (22) | 2013 | Perspective | Religion was an essential requirement for health care institutions |
| Vaillant (7) | 2013 | Cross-sectional | Spirituality, including emotions and social interactions, depended on the limbic system |
| Chaves et al. (23) | 2015 | Cross-sectional | The strategy of spirituality was a practical and appropriate solution to resolve university students’ anxiety |
| Ahmadi et al. (24) | 2015 | Review | Spirituality and religion are useful in the palliative treatment of patients with cancer. |
| Jakovljevic (19) | 2017 | Perspective | Psychiatry and religion could creatively help improve the world in the current global crisis |
| Chen and VanderWeele (13) | 2018 | Longitudinal | In a large-scale longitudinal study that examined the impact of religious training on psychological health, health behaviors, and physical health of a group of adolescents for 14 years until the subjects’ adulthood, the authors figured out that young adults who attended religious ceremonies had higher levels of life satisfaction and were less likely to drink alcohol and have out-of-marriage relationships compared to their counterparts |
| Renz et al. (25) | 2018 | Cross-sectional | Spirituality could facilitate the process of death |
| Cramer et al. (26) | 2018 | Cross-sectional | Yoga was an effective intervention for people suffering from high levels of anxiety |
| Fidianingsih et al. (27) | 2018 | Cross-sectional | In a study investigating the effect of fasting, one of the obligatory practices of Islam, fasting showed to reduce anxiety in the elderly |
| Sharma and Singh (28) | 2019 | Cross-sectional | There were significant relationships between gratitude, spirituality, forgiveness, altruism, and well-being. |
4. Conclusions
When most people were worried about environmental disasters leading to an unknown future, the outbreak of COVID-19 shocked them by killing thousands of people. The depth of this tragedy has been such that people have to stay at home in quarantine, constantly listening to the news of the death toll. Whereas most professionals around the world are trying to prevent further spread of COVID-19, spirituality, and prayer, which have received little attention, can calm people down. One of the most important sources of human character and identity is religion, which has not been considered deeply in clinics (29). It is believed that religions caused some problems during the COVID-19 pandemic (30), but Muslims have done valuable protective activities to combat the spread of this disease, such as canceling the Friday prayer and congregational prayer (31). When the Ebola disease broke out in Nigeria, the federal government advised taking the counsel of Prophet Mohammad, who urged Muslims to cleanliness and wash their hands frequently (17). Cultural and religious faiths mainly influence patients’ lives (32). Moreover, religiosity increases longevity (15). In the last century, views of religious experts and psychologists about the question of life meaning have changed (11). Religions can play roles as facilitators, friends, and even critics for special healthcare (22). The fact that religions are among social factors determining health is a general compromise among experts (20). Countless religions in the world can be learned like languages and create positive emotions in humans, and these positive states help us to survive in the unknown future (7). In the current global situation that humans live in anxiety and stress, and numerous studies have supported the positive effects of spirituality on people’s mental health, especially in times of crisis and acute diseases, virtual worships and spiritual podcasts can be the perfect solutions to create mental relaxation and spirituality in people. It has been suggested that medical staff in hospitals pay more attention to the spiritual and religious beliefs of COVID-19-infected patients to improve their calmness and well-being. More importantly, various Islamic advice such as cleanliness and forbidding eating wild birds (Haram) like bats, known as the main reason for the transition of COVID-19, can protect humans against infectious disease pandemics.