1. Background
Today, we encounter a warning increase in the incidence of psychiatric disorders (1) as the most important health problems in the world (2). Currently, around 20-30% of people in societies are affected by psychiatric disorders (3). Among these disorders, schizophrenia, bipolar, and major depressive disorders are the most common and severe ones. In Iran, more than 25% of people in the community suffer from psychiatric disorders, of whom about 1% are schizophrenic, 6% are bipolar, and 6-13% are depressed (4). These psychiatric disorders have negative effects on the quality of life, interpersonal relationships, and social function of patients (5).
The negative effects of severe psychiatric disorders are not limited to the person with the illness but extend to the family members. Providing care to family members suffering from prolonged illness challenges the well-being of the family caregivers, and they suffer from heavy physical and psychological burdens (6). However, in our country, the mental health of the family and the challenges of families with psychiatric patients are neglected by health care providers.
As the presence of a patient with psychiatric illness is considered a major stressor for the family, it seems that this factor can affect the components of the family structure, especially the hierarchy of power and dynamic of cohesion (7). "Power" in the family is defined as the ability to influence other family members (8). The power affects the development of personality, socialization, and satisfaction of family members. When power is clearly distributed between family members, they will have the opportunity to grow individually and increase self-esteem in the family (9). Evidence suggests that the presence of a psychiatric patient can change the structure of power in the family. In a study conducted in Brazil, the results show that the presence of a chronic mental patient affected the hierarchy of power in the family members (10). "Cohesion" indicates emotional relationships between parents and children. Cohesion reflects the level of emotional relationships of family members (11). According to research findings, family cohesion is an important factor in emotional independence (12) and plays a protective role against depression (13). On the contrary, negative relationships between family members can cause psychological problems in the family climate (14).
In Iran and even other countries, there is limited evidence on the effects of the presence of psychiatric patients on the family structure (12, 15). For example, the results of a longitudinal study have shown that the presence of a patient with bipolar disorder reduces family cohesion (16). Also, family power and cohesion have often been investigated in studies evaluating non-psychiatric patients (17). In addition, to assess the family structure, most of the studies have used questionnaires with a large number of questions, which are not suitable for psychiatric patients.
2. Objectives
This study aimed to compare the power, cohesion, and structure of healthy families and families with psychiatric patients.
3. Methods
3.1. Design, Setting, and Participants
This cross-sectional study was conducted in Shiraz. The participants included patients with schizophrenia, Bipolar Disorder (BD), Major Depressive Disorder (MDD), and a member of healthy families. The inclusion criteria for patients were age over six years, the family size of at least five persons, a known case of schizophrenia, BD, or MDD, intension to cooperate, parents not separated, and family members living together. The exclusion criteria included patients in acute or aggressive status, patients with recent electroconvulsive therapy, and patients not willing to continue participating in the study. The inclusion criteria for healthy participants were the same, except for not having a psychiatric illness. They were excluded from the study if they refused to continue participating in the study. All participants were selected using convenience sampling. The psychiatric patients were recruited from the Ibn-Sina and Hafez psychiatric hospitals in Shiraz, and healthy participants were recruited from the staff working in organizations. Each evaluation took 5-10 minutes.
Before the main study, a pilot study was conducted, which disclosed β = 0.2 and α = 0.05. According to the sample size formula:
corrected by
(k: number of comparing groups), the minimum sample size was 60 participants in each group. Accordingly, a total of 322 participants were included in this study.
3.2. Data Collection
Data were collected using the Family System Test (FAST) from September to November 2018. The FAST was designed by Gehring and Willer in 1986. This clinically-derived figure placement technique has been designed to evaluate cohesion and power in the family. The FAST consists of a 45×45 cm monochromatic chessboard, with 81 squares of 5×5 cm that form a total of 9×9 squares. Schematic figures in male and female shapes and cylindrical blocks in sizes of 1.5, 3, and 4.5 cm were placed under the schematic figure, showing the power of hierarchy (Figure 1). The power is calculated through the height of the blocks used to elevate the figures, with growing differences indicating increasingly marked power. The evaluation of family power is based on the height difference between the less elevated parent figure and the most elevated childe figure. Low power is when the difference in parent-child height is less than one small block. The medium power is when the parent-child height difference is one or two small or middle-sized blocks. High power is when the difference in height between parent and child is a large block or more.
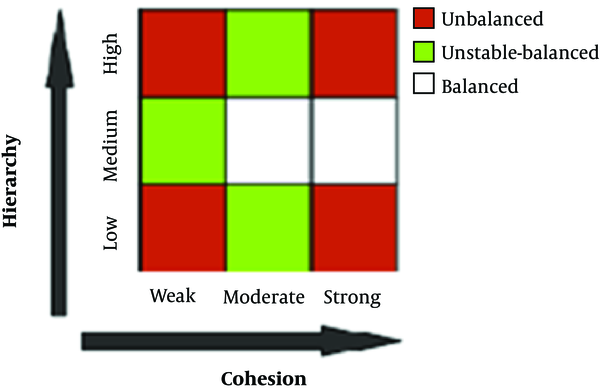
Cohesion scores are obtained from distances between the figures. The distance between figures is scored 1 on adjacent squares and 1.4 on diagonally adjacent squares. The maximum dyadic distance score is 11.3. To generate the cohesion score, each of the distance scores is subtracted from 12. Cohesion scores, thus, range from 0.7 to 11, with the higher scores indicating increased cohesiveness. According to the power and cohesion of the family, there are three types of family structure (Figure 2). A balanced structure indicates a moderate to high cohesive and medium power. A labile-balanced structure indicates a family with moderate cohesion and low or high power, or low cohesion and moderate power. Finally, an unbalanced structure is when both dimensions of cohesion and power are low or high (18). The validity and reliability of the tools were evaluated and reported in a previous study (17). In this study, the reliability of tools was evaluated by the test-retest method, and the correlation coefficients for power and cohesion were 0.86 and 0.94, respectively.
3.3. Ethical Consideration
This study was approved by the Research Ethics Committee of Bushehr University of Medical Sciences (IR.BPUMS.REC.1396-15). Participation in the study was voluntary, and written informed consent was obtained from all participants.
Data were analyzed using SPSS version 19 (Chicago, IL, USA). Descriptive statistics (frequency, mean, and standard deviation) were utilized to describe the data. The chi-square, Mann Whitney U, and Kruskal Wallis H (post hoc: Dunnett’s) tests were used for inferential statistics. The significant level was set at α = 0.05.
4. Results
The mean age of the participants was 32.12 ± 9.21 years. Besides, 63.3% were males, 40.15% were unemployed, and 85.2% were living in urban areas (Table 1). There was no difference in real and ideal power between the healthy families and families of depressive patients, healthy families and families of bipolar patients, and the healthy families and families of schizophrenic patients (P > 0.05) (Table 2). The results showed a significant difference in terms of real cohesion between the healthy families and families of depressive patients (P = 0.01). Hence, the mean score of real cohesion was higher in healthy families than in families of MDD patients. No significant difference was observed between these two families in ideal cohesion scores (Table 2).
| Variable | Healthy | MDD | Bipolar | Schizophrenia | No. |
|---|---|---|---|---|---|
| Age (mean ± SD) | 26.82 ± 5.78 | 33.4 ± 9.84 | 33 ± 11.47 | 35.17 ± 9.77 | 322 |
| Frequency (%) | 105 (32.6) | 65 (20.2) | 71 (22) | 81 (25.2) | 322 |
| Gender | |||||
| Male | 55 (52.4) | 36 (55.4) | 41 (57.7) | 71 (87.7) | 203 |
| Female | 49 (47.7) | 28 (44.6) | 29 (42.3) | 10 (12.3) | 116 |
| Job | |||||
| Employed | 62 (59.0) | 39 (60.0) | 46 (64.8) | 45 (55.6) | 192 |
| Unemployed/Retired | 43 (41.0) | 26 (40.0) | 25 (35.2) | 36 (44.4) | 130 |
| Education | |||||
| Academic | 75 (71.4) | 15 (23.1) | 14 (19.8) | 17 (21.0) | 121 |
| Non-academic | 30 (28.6) | 50 (76.9) | 57 (80.2) | 64 (79.0) | 201 |
| Father job | |||||
| Employed | 78 (74.3) | 45 (69.2) | 55 (77.5) | 64 (79.0) | 242 |
| Unemployed/Retired | 27 (25.7) | 20 (30.8) | 16 (22.5) | 17 (21.0) | 80 |
| Mother job | |||||
| Employed | 9 (8.6) | 8 (12.3) | 6 (8.4) | 4 (4.9) | 27 |
| Housewife/Retired | 96 (91.4) | 57 (87.7) | 65 (91.6) | 77 (95.1) | 295 |
| Father education | |||||
| Academic | 17 (16.2) | 7 (10.7) | 3 (4.3) | 3 (3.7) | 30 |
| Non-academic | 88 (83.8) | 58 (89.3) | 68 (95.7) | 78 (96.3) | 292 |
| Mother education | |||||
| Academic | 4 (3.8) | 5 (7.7) | 2 (2.8) | 3 (3.7) | 14 |
| Non-academic | 101 (96.2) | 60 (92.3) | 69 (97.2) | 78 (96.3) | 308 |
Description of Participants
| Variable | Real | P Valuea | Ideal | P Valuea |
|---|---|---|---|---|
| Power | ||||
| Healthy | -0.19 ± 1.78 | 1.07 ± 0.92 | ||
| MDD | 0.02 ± 1.8 | 0.27 | 0.85 ± 0.99 | 0.08 |
| BD | -0.31 ± 1.91 | 0.99 | 1.07 ± 0.98 | 0.94 |
| Schizophrenia | -0.04 ± 1.81 | 0.57 | 1.00 ± 0.91 | 0.61 |
| Cohesion | ||||
| Healthy | 9.65 ± 1.58 | 10.51 ± 0.46 | ||
| MDD | 8.57 ± 2.21 | 0.01 | 10.62 ± 0.18 | 0.06 |
| BD | 8.83 ± 2.33 | 0.32 | 10.58 ± 0.31 | 0.14 |
| Schizophrenia | 9.17 ± 2.08 | 0.94 | 10.50 ± 0.57 | 0.47 |
Comparison of Power and Cohesion in Real and Ideal Conditions Between Healthy and Psychiatric Patients' Families
The findings revealed a significant difference between the family structures of the four groups (P = 0.008). Accordingly, there was a significant difference between the healthy and depressive groups (P = 0.016), healthy and bipolar groups (P = 0.016), and healthy and schizophrenia groups (P = 0.005) in terms of family structure (Table 3).
| Family | Balanced | Labile-Balanced | Imbalanced | χ2(2) | P Value |
|---|---|---|---|---|---|
| Healthy | 61 (58.1) | 23 (20) | 21 (21.9) | 17.40 | 0.016 |
| MDD | 23 (35.4) | 21 (32.3) | 21 (32.3) | ||
| Healthy | 61 (58.1) | 23 (20) | 21 (21.9) | 8.33 | 0.016 |
| BD | 27 (38) | 15 (21.1) | 29 (40.8) | ||
| Healthy | 61 (58.1) | 23 (20) | 21 (21.9) | 10.79 | 0.005 |
| Schizophrenia | 28 (34.6) | 21 (25.9) | 32 (39.5) |
Comparison of Family Structure Between Healthy Families and Families with Psychiatric Patients
5. Discussion
The results showed that there was no significant difference between healthy families and families of psychiatric patients in terms of power. Consistently, the results of a study showed that there was no difference between the families of disabled and healthy individuals in terms of power (17). Inconsistent with our study, Brazilian researchers who conducted a study on the families of psychiatric patients found that the presence of a chronic mental patient affected the hierarchy of power in the family (10). Also, there was evidence that the family system of patients with schizophrenia was characterized by an uneven distribution of power and the existence of parent-offspring coalitions. Researchers argued that the uneven distribution of power in these families might be related to the premorbid period and was not necessarily related to the onset of the disease (19). Further studies are needed in this area.
The results of our study showed that cohesion was significantly lower in the family of patients with MDD than in healthy families. Consistent with this study, the results of a study showed that the family had revers cohesion with the degree of depression in cancer patients (15). The results of another study showed that depression had a predictive role in family cohesion (20). Researchers believe that several factors contribute to family adaptation during the illness of family members, and one of the most important of these factors is family cohesion (21). Contrary to these results, the findings of a study showed that in the actual situation, the highest cohesion was among healthy families, but in the ideal situation, the highest cohesion was observed in families with chronic patients (22). Also, the results of a study revealed that family cohesion of children with autism was at a higher level than that of the general population. It suggests that family members of children with autism were more emotionally linked with each other. Researchers concluded that philosophy and cultural beliefs emphasize individual growth and inspire individuals to strive for getting along with others in harmony posterior to encountering difficulty, which may encourage family caregivers to deal with their problems effectively and promote family bonding (23). For all that, families with chronic patients constantly engage their minds with patient problems. They ignore their physical and mental well-being that might result in psychiatric illness. Some families feel ashamed of having such psychiatric patients and attempt to limit their relationships with other people. In this challenging and anxious environment, family cohesion is affected, and thus, it can be concluded that families with healthy members have more cohesion than have families with ill members (17).
The results also indicated that the structure of the families of healthy people is more balanced than that of the families of patients with psychiatric disorders. In this regard, Nuovo and Azzara showed that families with chronic patients had a high degree of unbalanced structures (24). As far as we know, the physical and mental health of the family members depends on the family structure stability, and the presence of a psychiatric patient in the family often causes irreparable damages to the family (10). Evidence reveals that in the families of patients with schizophrenia and depression, illness-related factors are the main sources of stressors for the family caregiver (25). In other words, when a family has to deal with a disabled member, the family experiences severe stress due to the need for providing prolonged special care that can endanger the physical and mental health of the family members (26).
5.1. Strengths and Limitations
According to our knowledge, this is the first time that the FAST tool is used to assess the family structure of psychiatric patients in Iran. The limitation of this study was the assessment of the hierarchy of power and cohesion from the perspective of only one family member.
5.2. Conclusions
The results indicated that the unbalanced structure of families with psychiatric patients seems to be due to a series of stressors that are not present in healthy families. Family structure is one of the most important domains in the evaluation of psychiatric patients, and it is known that there is a bidirectional interaction between patients and their families. The presence of a psychiatric patient interferes with many aspects of family dynamics and creates a need for support and counseling. Therefore, FAST is a valuable tool to evaluate the family structure and dynamics of the psychiatric patient's family to understand the psychological and emotional needs of these families.