1. Context
Nowadays, the rates of morbidity and mortality due to problems in cardiovascular and respiratory systems are increasing because of the increases in air pollutant emissions by vehicles, industries, economic development, and dust storms (1-4). Major sources of pollutants that are harmful to the environment and human health include industries, transportation systems, power plants, and population growth (5-8). A major policy worldwide is to decrease air pollutants because of their different health effects on citizens (9-13). In the world (United States, Europe, and Asia), several studies have reported the effects of air pollution on human health. The results of these studies showed that higher concentrations of PM10, O3, NO2, SO2, metals, and polyaromatic hydrocarbons (PAHs) can increase the risk of morbidity and mortality due to respiratory infections, chronic obstructive pulmonary disease, asthma attacks, coughing, reduced lung function, eye irritation, cardiovascular disease, stroke, respiratory and cardiovascular death) (14-20).
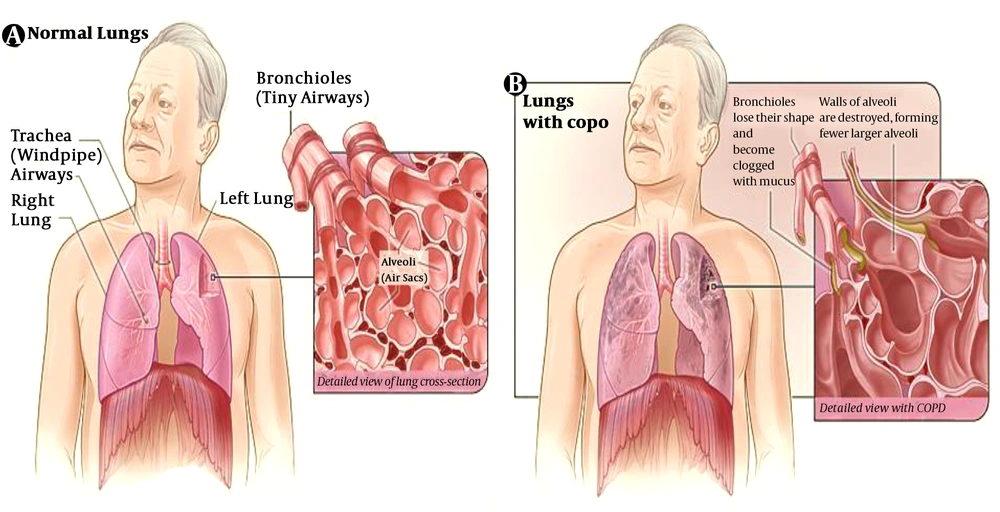
Based on several reported, epidemiological human systems that are sensitive in exposure to air pollutants are nervous, cardiovascular, and respiratory systems. The main organs whose functions are impaired due to short and long-term exposure to air pollutants are the heart, lung, brain, and eyes (19, 21-23). Poor airflow and long-term breathing problems due to disrupted lung tissue are defined as Chronic Obstructive Pulmonary Disease (COPD) (8). It is a disease that makes breathing, walking, or getting dressed become difficult (24, 25). Nowadays, COPD is one of the commonest respiratory diseases worldwide (26). Tobacco smoking, air pollution, and genetic factors are the important factors causing COPD (27). This disease can be prevented by reducing cigarette smoking and improving the air quality (28). Lung function tests by measuring the airflow is a way to diagnose COPD (29). Inhaled bronchodilators, respiratory rehabilitation, vaccination, and smoking cessation are the best ways for COPD treatment (30).
Chronic obstructive pulmonary disease, bronchitis, asthma, repository disease, and lung cancer are the main health effects of air pollution on the repository system (26). This narrative review aimed to evaluate the link between the development and progression of COPD and air pollutants. Moreover, we focused on the current state of knowledge of the association between COPD and air pollution.
2. Evidence Acquisition
In this narrative review study, we used available studies in various databases, including Google Scholar, Science Direct, Web of Science, Springer, PubMed, NCBI, and BMJ (Table 1). The year of publication (1978–2020) and the English language were the main criteria for search limitation.
| Term | Google Scholar | Web of Science | Springer | Science Direct | PubMed | BMJ | Unique results |
|---|---|---|---|---|---|---|---|
| Chronic obstructive pulmonary disease | 302 | 137 | 51 | 87 | 96 | 36 | 295 |
| Respiratory systems | 230 | 121 | 46 | 70 | 75 | 21 | 173 |
| Respiratory diseases | 136 | 81 | 51 | 53 | 63 | 13 | 142 |
| Air pollution and lung | 97 | 52 | 31 | 57 | 50 | 9 | 130 |
| Air pollution and respiratory systems | 81 | 39 | 17 | 31 | 46 | 6 | 94 |
| Total | 846 | 430 | 196 | 298 | 330 | 85 | 834 |
Search Terms and Query Results
2.1. Data Gathering
‘Chronic obstructive pulmonary disease’, ‘respiratory systems’, ‘respiratory diseases’, ‘air pollution and lung’, and air pollution and respiratory systems. Overall, 62 relevant original and review papers were reviewed to establish the possible link between cardiovascular and respiratory diseases with exposure to air pollution... Duplicate articles from different searches were removed before starting the screening process.
2.2. Ethical Approval
Ethical approval of the present study was acquired from the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Code of ethics: IR.AJUMS.REC.1399.700). According to the national guidelines, studies such as the current one do not require individual consent.
3. Results
The results of the narrative review study included six categories: Functional structure and biochemically active compounds for the lung, major airborne pollutants harmful to the lung, the pathophysiology of COPD, and action mechanisms of PM, VOCs, metals, and PAHs on the human respiratory system and air pollution, COPD, and clinical manifestations of the effect of air pollutants on COPD.
3.1. Functional Structure and Biochemically Active Compounds for the Lung
The primary organs of the respiratory system are the lungs, including two lungs. The main role of the lungs is to extract oxygen from the atmosphere, release carbon dioxide from the bloodstream, and provide airflow that makes vocal sounds (31). The respiratory system includes an upper respiratory system (nose and nasal passages, sinuses, and pharynx) and a lower respiratory system (larynx, trachea, bronchi, and bronchioles) (32). The respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli can be included in the lower respiratory tract (33).
3.2. Major Airborne Pollutants Harmful to the Lung
Gender, age, and exposure duration are the most important factors affecting human health and lung condition, and air toxicants exert harmful effects (34). In the atmosphere, Particulate Matters (PMs) form a complex of small particles and liquid droplets (35). Soil, dust, metals, acids, and organic chemicals are the major sources of PMs (36). Particulate matters are among the most serious air pollutants in Europe (37).
Toxic gaseous pollutants include Volatile Organic Compounds (VOCs), CO2, CO, NO2, SO2, and ground-level ozone. Besides, BTEX (benzene, toluene, and xylene) are important compounds, which play a crucial role in the formation of ground-level ozone. Among metals, lead, cadmium, chromium, nickel, and zinc are the most frequent airborne pollutants (38). There are reports on the considerable toxicity of airborne metals to the lung (39). Polycyclic Aromatic Hydrocarbons (PAHs) are a group of hydrocarbons that are composed of multiple aromatic rings (16). Human exposure to PAHs can cause different health effects (15, 16).
Polycyclic aromatic hydrocarbons that occur in air dust have highly bioaccumulative properties and can bind to cell macromolecules. Air pollutants can induce chronic human health effects and have been recognized as extremely toxic to the lung (40). In fact, contaminated air can contain over 2,000 different chemicals and compounds that can strongly influence the development of serious lung pathologies (41).
3.3. Pathophysiology Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease is caused by poor airflow and long-term breathing problems due to disrupted lung tissue (42). Bullous emphysema is defined as damage to large focal lung pneumatosis that replaces lung tissue (43, 44). Macrophages and neutrophil granulocytes, two types of white blood cells, are the main inflammatory cells (45). The most important processes that can cusses lung damage are free radicals in tobacco smoke and oxidative stress. (46-49). The most common complications of chronic obstructive pulmonary disease and poor lung function (destruction of lung tissue) are poor airflow, emphysema, poor absorption, and release of respiratory gases (Figure 1) (46-49).
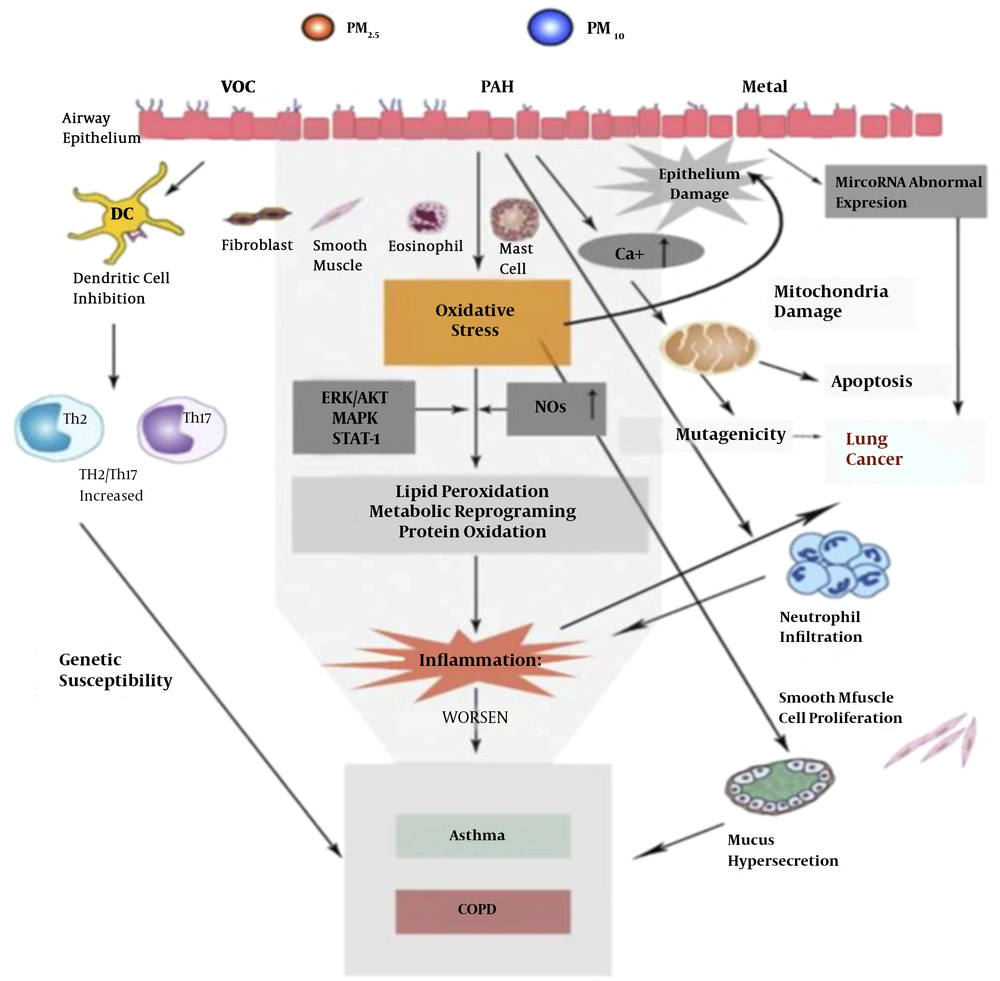
3.4. Action Mechanism of PM, VOCs, Metals, and PAHs on Human Respiratory System
The effects of ambient PM, VOCs, metals, and PAHs on mortality have been investigated for decades (50). Several epidemiological studies have reported a robust correlation between PM, VOCs, metals, and PAH pollutants and cardiovascular and respiratory diseases (51-56). There are several proposed mechanisms for the impact of PM, VOCs, metals, and PAHs on human respiratory physiology (50). Chronic inflammation due to the effects of air pollutants exposure on respiratory systems, including the binding of pathogenic antibodies to pro-inflammatory cell receptors, is presented in Figure 2.
Route of the destruction of the human respiratory system after air pollutants exposure. MAPK: mitogen-activated protein kinase; ERK: extracellular regulated protein kinases; STAT-1: Signal transducers and activators of transcription-1 (50)
3.5. Air Pollution and Chronic Obstructive Pulmonary Disease
Improved indoor and outdoor air quality may prevent COPD (57). Personal involvement, cultural changes, and public policy changes have the most important efforts on the decreased rate of the incidence of chronic obstructive pulmonary disease (47, 58). One of the best activities that developed countries have successfully done for decreasing health outcomes is the development of regulations regarding air quality (57). Those with COPD may experience fewer symptoms if they stay indoors on days when outdoor air quality is poor (47). Good ventilation at home and better stoves are the keys to decreasing smoke emissions from cooking and heating fuels (47, 58). Based on the results of different studies, improved stoves can improve indoor air quality. Using alternative energy sources such as solar cooking and electrical heating is also effective. Using fuels such as kerosene or coal might be less harmful than traditional biomass such as wood or dung (57). Coal mining, construction, and stonemasonry are the major industries whose workers are at increased risk of COPD due to exposure to pollutants emitted from these industries (57). One of the ways that can reduce COPD and further lung damage in workers is to change their role in the workplace (59).
3.6. Clinical Manifestations of the Effect of Air Pollutants on Chronic Obstructive Pulmonary Disease
Hazardous air pollutants induce destructive effects on the lung and result in chronic obstructive pulmonary disease (37). The permanent production of ROS under the exposure of the lung to air toxins causes the secretion of cytokines and cellular dysfunction. Consequently, the breakdown of the lung is observed, and some abnormal conditions such as chronic obstructive pulmonary disease, inhalation, bronchitis, and lung cancer can be initiated (29, 45).
3.7. Future Research About COPD in Iran
Based on the projection of the World Health Organization (WHO) about chronic obstructive pulmonary disease, this disease will become the third leading cause of death by 2030. Nowadays, one of the most important public health problems in Iran that have an increasing trend is COPD. Demonstrating that prevention and early detection chronic obstructive pulmonary disease should be considered, especially in the age group of 15 to 70 years.
4. Conclusions
The findings of this study can have wide applications for the health effects of air pollution. There is a large and growing body of epidemiological evidence associating the emissions of air pollutants with increased COPD worldwide. Chronic obstructive pulmonary disease is a critical public health issue in Iran and the world. It has had an increasing trend in recent years. The lung as a vital organ of the human body stays in direct and continuous contact with the environment and its pollution. Lung pathologies not only result from internal disturbances in body metabolism and processes. There is considerable evidence that air pollution increases oxidative stress in repository system cells.
Defining policies for decreasing air pollution by using green fuels such as solar and electrical energy, actions to reduce emissions to air in industries and source of dust in neighboring countries, implementing appropriate health measures, and developing green spaces can be effective in reducing chronic obstructive pulmonary disease. Therefore, government authorities at various levels should put legislative frameworks for protecting the residents against the high health risks and other effects of air pollution.