1. Background
Coronary artery disease (CAD) is a disease that causes reduced blood flow to the heart due to the narrowing of the inner layers of the heart vessels (1). Heart failure (HF) is the heart's incapability to pump suitably to preserve blood circulation in order to meet the body tissue's metabolic needs (2).
Seasonal variations in the incidence of acute myocardial infarction (MI) (3-5) and sudden death (6) are well known. Ambient temperature contributes to this variation because these events peak in winter. Some of the physiological consequences of hypothermia are thought to increase the risk of coronary heart disease and may also be dangerous in HF. Skin cooling increases systemic vascular resistance (7), heart rate (8), plasma norepinephrine concentration (9), circulating levels of vasoconstrictor peptides (10), and blood pressure (11). By observing these cases, blood pressure is higher in winter (12). Cold can also induce myocardial ischemia (13). All of these effects can clearly lead to worsen the disease. Other seasonal changes such as respiratory infections can also threaten HF stability.
In 2012, cold was the leading cause of death in the world (14). There is limited evidence for population screening, but complications can be prevented and controlled through a healthy diet and medications to control diabetes, cholesterol, and blood pressure. Ischemic heart attacks increase with exposure to cold air. Several articles around the world, along with quarterly studies on CAD, have shown increased mortality in the winter months (15). The mortality rate and hospitalization due to CAD are lower in the warmer months (16). Seasonal variations have been effective both in heart diseases and in all causes of mortality (17). One reason is that during the winter flu season, there is an increase in mortality due to flu and other viral illnesses in patients with heart diseases, and the development of an infectious respiratory phenomenon in individuals with a history of cardiovascular disease causes cardiovascular events (18, 19).
Previous studies have shown that not only daily changes in heart disease mortality are associated with increased mortality on weekends (20), but also rhythmic changes in heart disease are associated with higher mortality in the early morning (21). Regular physical activity has a reducing role in 20% of cases of acute coronary heart disease (22). It has also been reported that the increased risk of heart attacks over the Christmas holiday has been non-climatic and due to food intake (23). A study in 11 different countries showed that cardiovascular diseases occurred more in winter than in summer (24).
HF is a chronic disease that has a negative impact on patients’ lives compared to a healthy population or other chronic diseases with debilitating complications (25). Affected individuals will experience periods of acute exacerbation, which occur under the influence of risk factors and environmental conditions and require emergency care and hospitalization. This disease has a bad prognosis with a mortality rate of 10% and leads to the same hospitalizations, with 20 to 40 % deaths a year after discharge (26). In compensated HF, the increased need for cardiac output in hot weather to increase blood flow to the skin in order to expel heat from the body can cause symptoms of HF and even death, especially in the elderly (27, 28).
It is important to find a pathological relationship between external factors such as climate and the incidence of coronary heart diseases such as MI and congestive HF (29). Most studies have been conducted in cold regions of the world and have focused on the effect of cold weather on coronary heart disease, and no important study has been performed on hot weather (30, 31). One of the important factors influencing the incidence and recurrence of HF symptoms is physical and environmental factors such as air temperature.
2. Objectives
Due to the fact that Ahvaz is located in a tropical region, hot weather and activity at high temperatures are considered as physical and environmental stressors which can be viewed as factors for recurrence or occurrence of heart diseases. Thus, it seems appropriate to conduct research to find the effect of weather in the cold and hot months on heart diseases in this tropical region.
In the present study, we aimed to assess the relation of the incidence of coronary heart disease and HF to the potential changes in the diseases’ type as well as the presence of risk factors during the hot weather and seasonal outcomes of the diseases.
3. Methods
3.1. Study Population and Research Design
The present study was conducted on all patients who were admitted to the coronary care unit (CCU) of Imam Hospital in 2013 and 2014. At first, the total number of medical files of patients was determined. Then, patients with diagnoses of unstable angina (UA), MI, and HF were separated and examined separately by the month of hospitalization.
3.2. Ethical Code
Permission to carry out this research project was issued by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (ethics code: IRAJUMS.REC.1396857).
3.3. Method
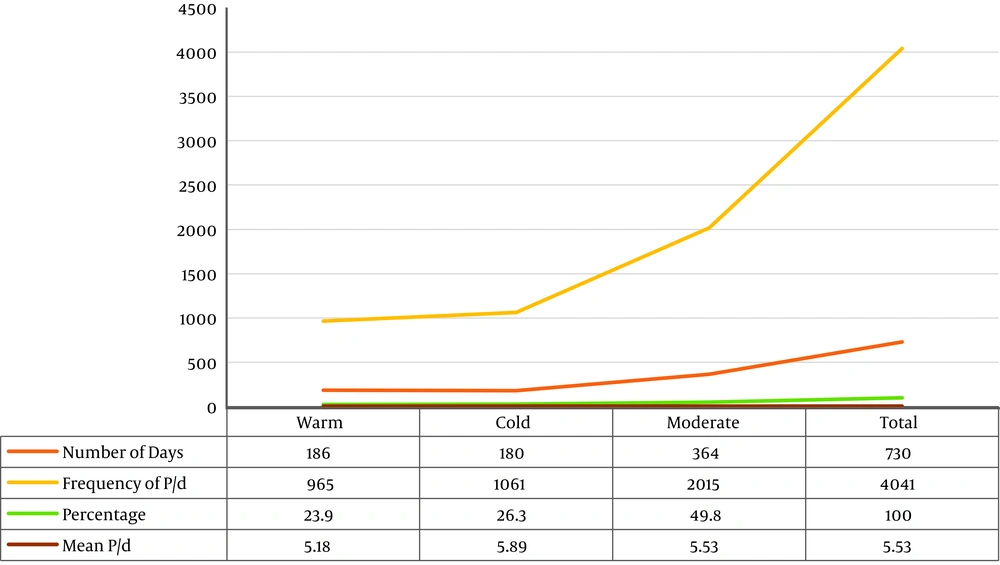
In this retrospective descriptive-analytical study, the medical files of patients referred to Imam Hospital, a university medical center in Ahvaz located in Khuzestan province, were studied from 20 March 2013 to 20 March 2014. To use the medical files of patients in the archive department of Imam Hospital, first, the necessary permission was obtained. Then, by examining the patients’ files, according to the desired diagnosis, necessary data were collected as follows: (1) file number; (2) diagnosis of MI according to the previous history; (3) electrocardiogram changes; (4) troponin and creatine phosphokinase (CPK) tests; (5) cardiac UA in accordance with the previous history; (6) electrocardiogram changes without an obvious increase in biomarkers; (7) HF in accordance with previous history and physical exam; (8) cardiac ejection fraction recorded on echocardiography; (9) pulmonary edema and other evidence of fluid accumulation; (10) age; (11) gender; and (12) closure date. Also, the patient’s discharge date was entered into the checklist. Then, the obtained data were analyzed and interpreted according to the aims and hypotheses of the study. Based on the data obtained from the General Weather Bureau of Khuzestan, the months of the year were divided into 3 groups: (1) cold months, (2) warm months, and (3) moderate months. According to the definition of the weather bureau, if the average air temperature in a month (total minimum and maximum temperatures in a day divided by 2) is equal to or less than 18.35 degrees Celsius (°C), that month is considered cold, and those months with average air temperatures equal to or higher than 35.80°C are considered warm. The average temperatures of Ahvaz in 2013 and 2014 were 25.8°C and 26.6°C, respectively, and other months of the year were considered moderate. Also, according to the statistics of the General Weather Bureau of Khuzestan, in 2013, July and August were the warm months of the year, and December, January, and February were the cold months of the year. In 2014, June, July, August, and September were the warm months of the year, and December, January, and February were the cold months of the year in Ahvaz. Other months of the year were considered moderate. According to this classification, during the two years under study, 186 days were in the warm season, 180 days were in the cold season, and 364 days were in the moderate season. In this study, in order to homogenize the data for comparison according to the differences in the number of days of the seasons, the criterion of the average number of patients admitted per day was used, which was the result of dividing the number of patients referred to the hospital in each season by the number of days in that season, so that the prevalence of referrals was comparable to the number of patients per day (P/d). The present study hypothesized that, like similar studies on seasonal variations and the incidence of diseases, factors such as non-use of drugs, smoking, and the emergence of new non-infectious diseases are not affected by seasonal variations.
3.3.1. Data Collection Tool
Data were collected by referring to medical files and completing patients’ checklists. Data including patients’ age, gender, hospitalization date, discharge date, and final diagnosis were extracted from the files and were analyzed.
3.3.2. Statistical Analysis
To analyze the data, the mean and standard deviation were used in quantitative variables, and frequency and percentage were also used in qualitative variables. Then, in order to measure the relationship between variables, the chi-square test, Fisher's exact test, and independent t or its non-parametric equivalent, i.e., Mann-Whitney, were used. Finally, P-value ≤ of 0.05 was considered significantly correlated. All analyses were performed using IBM SPSS Statistics version 22.0 (Chicago, Illinois, USA).
4. Results
This study investigated seasonal variations in HF and acute coronary syndrome (ACS) in 2013 and 2014, by reviewing the medical files of 4,041 patients.
According to the General Weather Bureau of Khuzestan, in 2013, the minimum temperature of Khuzestan was 12°C, and its maximum temperature was 50.4°C, with the mean temperature of 25.806°C and a standard deviation of 9.2476°C. In 2014, the minimum temperature of Khuzestan was 4°C, and its maximum temperature was 50.6°C, with the mean temperature of 26.6°C and a standard deviation of 9.124°C.
The subjects’ mean age was 62.5 ± 14 years (with a minimum of 27 and a maximum of 92 years). According to the results, patients under 40 years of age had the lowest, and 50 - 59-year-old patients had the highest frequency. Of 4,041 studied patients, 625 were diagnosed with HF, 2410 were diagnosed with UA, and 1006 were diagnosed with MI. The majority of patients (57%) were male, indicating statistical significance (P = 0.03) and a high prevalence of heart diseases in males (Table 1).
| Variables | No. (%) |
|---|---|
| Age range (y) | |
| > 40 | 197 (4.9) |
| 40 - 49 | 573 (14.3) |
| 50 - 59 | 1175 (29) |
| 60 - 69 | 1087 (26.9) |
| 70 - 79 | 684 (16.9) |
| < 80 | 325 (8) |
| Gender | |
| Male | 2303 (57) |
| Female | 1738 (43) |
| Diagnosis | |
| HF | 625 (15.5) |
| UA | 2410 (59.6) |
| MI | 1006 (24.9) |
The number of patients referred to the hospital in the cold season of the year was more than in other seasons. In this study, there was a significant difference between the P/d ratio in the cold season and that in the moderate and warm seasons (P = 0.014 and 0.006, respectively), and also between the moderate and warm seasons (P = 0.023). The number of days of each season of the year and the frequency of patients in terms of cold, hot, and moderate seasons are shown in Figure 1.
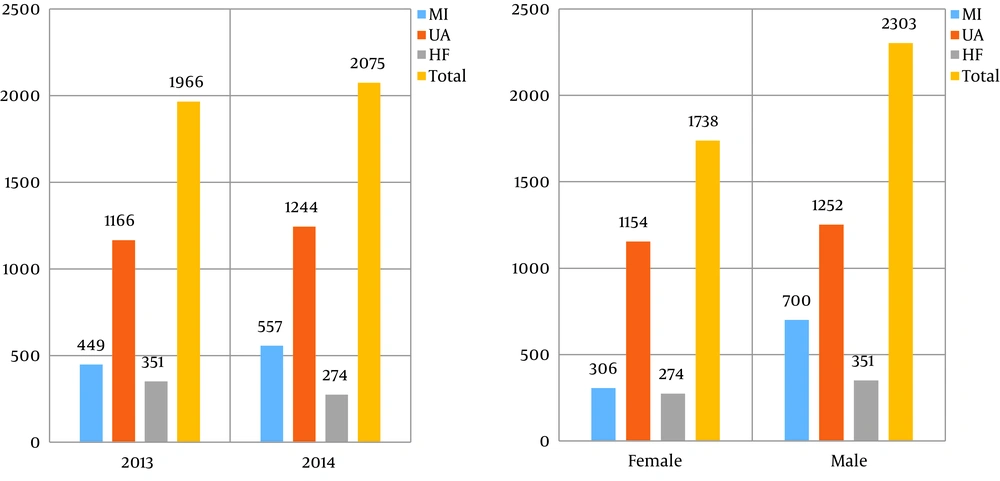
According to the results, the frequency of patients in 2014 was higher than in 2013. The UA patients had the highest, and the HF patients had the lowest frequency in 2014. There was a significant difference between gender and the overall prevalence of heart diseases which was higher in males (P-value = 0.03) (Figure 2).
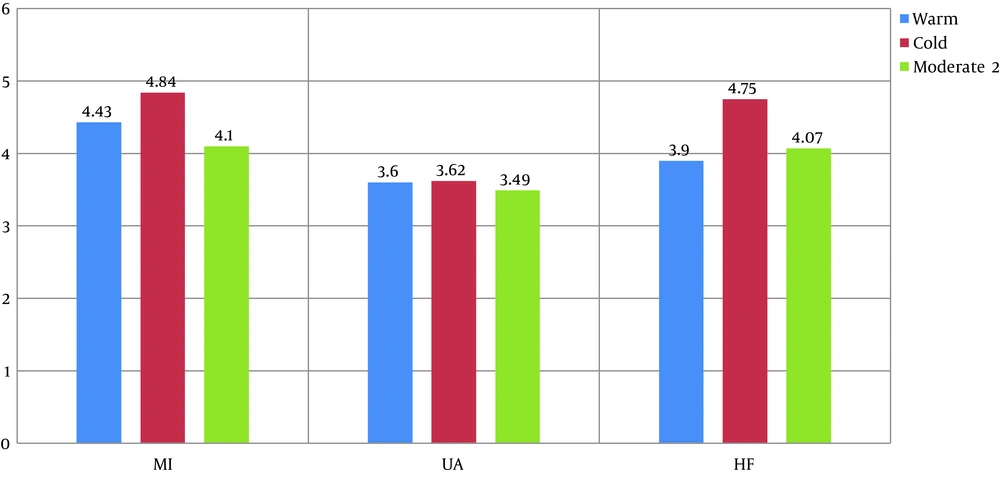
Most referrals in all seasons were related to patients with UA. There was a statistically significant difference in the total number of patients referred to hospital in different seasons (P = 0.001). However, in the next analysis to examine the number of referrals based on diagnosis and season according to the P/d ratio, a statistically significant difference was observed in the case of MI, which was more in the cold season than other seasons (P = 0.002). The longest hospitalization stay was observed in patients with MI in cold seasons (4.84 days), and the shortest hospitalization stay was related to patients with UA in moderate seasons (3.49 days). The mean hospitalization stay of MI and HF patients in the cold season was longer than other seasons, and this difference was statistically significant (P = 0.035 and 0.021, respectively) (Figure 3 and Table 2).
| Seasons | MI | UA | HF | P-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | P/d | Mean hospitalization days | No. | P/d | Mean hospitalization days | No. | P/d | Mean hospitalization days | ||
| Warm | 205 | 1.10 | 4.43 | 620 | 3.44 | 3.60 | 140 | 0.75 | 3.9 | 0.001* |
| Cold a | 299 | 1.66 | 4.84 | 584 | 3.24 | 3.62 | 178 | 0.98 | 4.75 | |
| Moderate | 502 | 1.137 | 4.1 | 1206 | 3.31 | 3.49 | 307 | 0.84 | 4.07 | |
| P-value | 0.002 | 0.035 | 0.035 | 0.47 | 0.36 | 0.021 | ||||
Abbreviation: MI, myocardial infarction; UA, unstable angina; HF, heart failure; P/d, patients per day.
a Comparing warm and cold seasons.
Table 2 shows the distribution of patients and the mean hospitalization days in hot, cold, and moderate seasons by diagnosis.
The highest number of patients referred to the hospital was in October, December, and January, respectively. In 2013, the most common diagnosis of patients was UA, and the largest number of patients with this diagnosis was admitted in August. Also, in 2014, the most common diagnosis of patients was UA, and the largest number of patients with this diagnosis was admitted in November and October.
As can be seen, there is no significant relationship between gender and referral seasons in patients with MI, HF, and UA (P = 0.194, P = 0.121, and P = 0.339, respectively) (Table 3).
| Type of diseases | Seasons | Total | P-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Warm | Cold | Moderate | |||||||||
| Male | Female | Sum | Male | Female | Sum | Male | Female | Sum | |||
| MI | 151 (73.2) | 54 (26.3) | 205 | 212 (70.9) | 87 (29.1) | 299 | 337 (67.1) | 165 (32.9) | 502 | 1006 | 0.194 |
| HF | 78 (57.7) | 62 (44.3) | 140 | 111 (62.4) | 67 (37.6) | 178 | 162 (52.8) | 145 (47.2) | 307 | 625 | 0.121 |
| UA | 322 (51.9) | 298 (48.1) | 620 | 318 (54.5) | 266 (45.5) | 584 | 612 (50.7) | 594 (49.3) | 1206 | 2410 | 0.339 |
| Total | 551 | 414 | 965 | 641 | 420 | 1061 | 1111 | 904 | 2015 | 4041 | |
a Values are expressed as No. (%) unless otherwise indicated.
5. Discussion
The present study was performed on 4,041 patients admitted to the CCU with a focus on three common diseases, including UA, MI, and HF. In a study conducted by Hinton et al., the most commonly diagnosed heart diseases were MI, UA, and atrial fibrillation, respectively (32). In another study by Benjamin et al., the prevalence of coronary heart disease was more than HF (33). These results are similar to the results of our study.
The difference in the prevalence of diseases in different studies is probably due to the geographical and demographic conditions of different regions. Ahvaz is a tropical region with a maximum temperature of about 50.4°C in the warm season and a minimum temperature of about 4°C in the cold season. In this study, 2303 patients (57%) were male, and 1738 (43%) were female, indicating a higher prevalence of heart disease in males. In a study conducted by Panagiotakos et al., the frequency of ACS in male patients was found to be higher than in female patients (34). Han et al. showed that the frequency of ischemic diseases in males was higher than in females (35). Therefore, the results of the present study are in line with previous studies and show a high prevalence of heart diseases in males. Based on the results of previous research and the present study, male gender is an effective risk factor for heart disease anywhere.
The present study revealed the highest frequency of patients diagnosed with MI (28%) and HF (17%) in the cold season and the highest frequency of patients with UA (64%) in the warm season. It means that hot weather, similar to cold weather, may be harmful to patients with CAD. In this regard, Piergentili et al. showed that the highest frequency of cardiovascular diseases was in the cold season, and the lowest was in the summer (20), similar to patients with MI and HF in our study. On the other hand, in their study, Ebi et al., showed that the hospitalization rate of cardiovascular patients increased by 6 - 13% (36) following variations and increases in temperature, which is consistent with our results of UA patients. In the study by Panagiotakos et al., the hospitalization rate of patients with ACS increased after increasing humidity and air temperature (34), which is also consistent with the results of patients with UA in our study. The results of the present study show a high incidence of heart diseases in the cold and hot seasons of the year. The difference in the prevalence of diseases in different studies is probably due to the geographical and demographic conditions of different regions.
Considering Ahvaz as the most polluted city in the world in November 2013, according to Etemad et al.’s study, more than one thousand residents with severe respiratory symptoms referred to the health centers (37).
According to the present study, the mean age of patients was 62.5 ± 14 years and the lowest frequency was observed in patients under 40 years of age, increasing with age. In Eskandari et al.'s study, the mean age of patients with HF was about 58 years, and the frequency of this group was higher (25). On the other hand, according to Nayha et al.’s study, most patients with ACS were 65 years old, which is almost similar to the results of our study (38).
In this context, our findings showed that patients’ mean hospitalization days in different seasons differed from the diagnosis. The highest mean hospitalization day in cold seasons was associated with MI (4.8 days), and the lowest mean hospitalization day in the moderate season was associated with UA (about 3.5 days).
People with coronary heart disease often develop angina when having a cold. In addition to cold temperatures, strong winds, snow, and rain can also reduce body heat. Cold weather can endanger people’s health, especially in patients with cardiovascular diseases. Thus, winter can affect the heart and blood circulation, but there are ways to avoid the danger of frostbite (31). The body sweats when exposed to hot weather, and this condition may cause it to lose more water than normal, leading to a drop in blood pressure. The extreme heat may not be a problem for most people, but it can put extra strain on the heart and circulation of patients with coronary heart disease. It means these patients can be at a greater risk if they have a heart condition. People over the age of 50 with heart disease or overweight patients should take precautions against heat (29).
5.1. Study Limitations
A limitation of this study was lack of access to the files of patients who were hospitalized with an initial diagnosis other than MI, ACS, and HF, but in addition to the main problem, they had mild symptoms of these diseases.
Population movements at the beginning of the school holidays in June, accompanied by a significant decrease in the number of people referring to all medical centers and offices, both private and public, and the related increase at the beginning of October and reopening of schools may affect our statistics and results; however, due to the lack of any statistics, it is not accurate to judge in this regard.
5.2. Conclusion
According to the results of this study, the average number of patients with MI and HF in the cold season and UA in the warm season has increased. There are longer hospitalizations in the cold season that can, of course, increase the burden on the country's health care system. This study clearly demonstrates the need for preventive measures against cardiovascular diseases, not only in winter, but also in the hot months of summer in countries with high temperatures and humidity.