1. Background
Contrary to popular belief, human diseases are not only physical, and we get sick mentally too. Although physical diseases can be diagnosed easier than mental illnesses, issues such as economic, social, and excessive work pressures, pandemic diseases (e.g., COVID-19), noise/air pollution, crime, and the spread of unaccompanied and substandard social media affect humans and their lives every day.
Generally, stress is a nonspecific response or reaction to the demands made on it or to disturbing events that occur in the environment (1). Stress can cause undesirable disorders (such as anxiety and depression) that lead not only to psychological damages but also to physical damages.
In general, anxiety is a diffuse, ambiguous, and unpleasant feeling, which is a primary symptom in different forms of anxiety disorders and associated with a wide range of behavioral symptoms (such as restlessness, fatigue, irritability, avoidance, cognitive symptoms, and difficulties in concentration) and distraction and physical symptoms (such as sleep disorder and other similar issues) (2).
Extensive sadness/low mood and the loss of interest or pleasure in daily affairs are the main presentations of depression. To be diagnosed as depressed, there is a list of changes in appetite or weight, sleep, and psychomotor function, which individuals must have at least 4 other presentations as follows: (1) low energy; (2) lack of self-worthlessness feeling or having the feeling of guilt; (3) poor concentration or problems in thinking or inability to make a decision; or (4) intrusive thoughts of death/suicidal thoughts or suicide plans/attempts (2).
It is estimated that about 350 million individuals suffer from depression worldwide. It affects the overall functioning of the body, particularly the mind (i.e., how people take care of themselves), which in turn translates into social consequences and burdens for their families. Depression, as a recurring and highly impairing disorder, intervenes with several daily activities at the society or family level. For those who develop depression at young ages, depression has negative consequences at the peak of their most productive years (3).
Depression is ranked by the World Health Organization (WHO) as the single largest contributor to global disability (7.5% of all years lived with disability in 2015); anxiety disorders are ranked sixth (3.4%). Depression is also the major contributor to suicide deaths, approximately 800000 per year (4).
It is argued that the brain is the most complex thing in the known universe, which has been the focus of many of the most alluring proposed enhancements (5).
Based on studies of the brain and observation of brain functions, therapists are increasingly working on brain centralized treatments. Quantitative electroencephalography (EEG) is a developed form of EEG analysis that involves recording digital EEG signals, which are processed, transformed, and analyzed using complex mathematical algorithms. Different behavioral and psychological processes can change the patterns of brain waves. The way of thinking, sleep stages, physical activities, stress, and mental illnesses are among the factors that can affect the patterns of brain waves. The examination of quantitative EEG can help the therapist to diagnose abnormality to recover it. Neurofeedback (NFB) therapy is one of the newest treatments that has been considered by researchers by the end of the 1970s. Such therapies open new ways of psychological treatments to improve science based on biological and physiological principles.
In NFB therapy, an individual learns to change the brain wave patterns by operant conditioning (6). The use of NFB as operant conditioning allows the individual to control the quantitative parameters of the EEG signal, and the person can regulate the rhythms of his brain signal (7).
NFB changes brain waves as a tool to improve a person’s function (8). The effectiveness of NFB is based on the disorder type, relating to a specific area of the brain (9) NFB is used to treat epilepsy, anxiety, depression, hyperactivity, learning disorder, and substance abuse disorder, as well as in improving sports performance (10, 11).
Neuro-linguistic programming (NLP) is an interdisciplinary field with a combination of cognitive psychology, information processing elements, and less psychoanalysis, which was established more than 40 years ago. NLP is a common technique initiated by Grinder, Bendler, and Pochlik in the early 1970s. This method was developed to recuperate the ways of thinking and communicating and individual growth (12).
As a result, imitating the perspectives of well-known therapists (Gestalt therapy by Perls, person-centered counseling by Rogers, Ericksonian hypnotherapy by Bandler and Grinder, cybernetic epistemology by Bateson, behavioral psychology and cybernetics by Ashby, and family therapy by Satir and Siburn) leads to the development of new patterns of thought and behavior, which its function is derived from prior imitated samples during the time.
NLP is based on the association between neurological processes (neuro), language (linguistic), and behavioral patterns that can be applied to adjust views and actions to achieve desired results (programming). In the recent decade, NLP has commercially attracted many psychologists and linguistics. NLP encompasses many areas, for example, job motivational workshops, business development, education, treatment, etc. NLP teaches the individual to adapt, control, and adjust themselves in different situations to achieve the desired result. In this study, the psychotherapist is only looking for the therapeutic aspect, usage of role models, and participants’ treatment techniques.
In a study on 50 cases with claustrophobia, Bigley and colleagues (2010) applied magnetic resonance investigation to demonstrate that NLP sessions using the fast phobia cure could reduce the anxiety scores (13). Wake et al. (2013) provided an evidence-based argument for the clinical effectiveness of NLP-based methods to treat phobia anxiety, posttraumatic stress disorder (PTSD), depression, and addictions, as well as a supporting commentary of other therapeutic applications (14). Transcranial direct current stimulation (tDCS) is a non-invasive method that directs mild electrical current into the brain; in this method, the anode pole raises cortical incitement, and cathode poles decrease cortical incitement (15). Hence, it is an inexpensive, safe, and painless method to modulate brain activity, which does not increase the risk of seizures (16). This method is a less invasive way to stimulate certain areas of the brain and can stimulate or restrain special parts of the brain selectively (16, 17).
Therefore, non-invasive brain stimulation, such as tDCS, as a vigorous and convenient method to moderate brain activity, is now available to manage several psychological problems, including obsessive-compulsive disorder (18-21), depression (22), and schizophrenia (23). The tDCS method is used to treat different anxiety-related disorders (e.g., generalized anxiety disorders (GADs) (24), social anxiety disorders (25), and anorexia nervosa (26). Further, tDCS is a convenient and low-cost method that uses 2 electrodes applied to a scalp. While the cathode (negative) intends to hyperpolarize the neuronal membrane threshold, the anode (positive) depolarizes it (27, 28). In a study on GAD patients and using a quasi-experimental design, Sadeghi Movahed et al. (2018) compared the effectiveness of tDCS, sham-tDCS, and pharmacological treatments to manage anxiety, depression, and worry. They reported that tDCS is a promising option to treat GAD, particularly for those with depressive and worry symptoms (29).
2. Objectives
The current study aimed to compare the effects of tDCS, NFB, and NLP on reducing depression, anxiety, and stress in patients.
3. Methods
The research design selected for this study was a quasi-experimental method consisting of pretest and posttest given to 3 experimental groups [i.e., NFB (n = 15), tDCS (n = 15), and NLP (n = 15) groups] and 1 control group (n = 15). In the present study, 3 intervention groups and 1 control group were measured twice (i.e., before and after treatment).
The statistical population of this study included patients with depression, anxiety, and stress referred to mental health experts at health service centers for required examination and treatment in 2019 - 2020. The patients, after being identified in the system and consulted by mental health experts, had been voluntarily referring to the clinic and a treatment team, including neurologist, neuropsychologist, clinical psychologist, and counselor.
The sample consisted of 90 patients with depression, anxiety, and stress disorders, among which 68 patients were randomly selected by taking into account the loss (60 main samples and 8 alternatives by the random number method using a random number generator). Disorders were diagnosed by a psychiatrist based on the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) according to inclusion criteria after a Structured Clinical Interview for DSM-5 (SCID-5). Out of 68, 45 subjects were selected to be divided into 3 experimental groups (i.e., NLP, NFB, and tDCS), and 15 subjects were selected for 1 control group (2 subjects were considered as alternatives for each group in case of avoiding cooperation; data of other patients could be replaced). In this study, to have an NFB therapy protocol, quantitative EEG was performed separately for each patient; then, the patient’s treatment protocol based on quantitative EEG was written by a neuropsychologist and a psychiatrist.
The number of treatment sessions was determined according to the psychiatrist’s recommendation and the patient’s recovery status (or review of NFB reports). The sessions were run in approximately 12 sessions during 6 weeks (2 sessions per week). Also, to have a tDCS treatment protocol, similar to the NFB treatment protocol, quantitative EEG was performed separately for each patient; then, the patient’s treatment protocol based on quantitative EEG was written by a neuropsychologist and a psychiatrist. To determine the targeted areas of the treatment and brain parts with non-standard functions, 2 electrodes with positive and negative poles were placed on the head using a sponge pad that was soaked by conductive solution. This method is less invasive to stimulate certain areas of the brain and can stimulate or restrain selectively special parts of the brain (16, 17). The number of treatment sessions was determined according to the psychiatrist’s recommendation and the patient’s recovery status (or review of NFB reports). The sessions were run in approximately 12 sessions during 6 weeks (2 sessions per week). The third group was treated with NLP in 1 session for therapeutic goals by a psychiatrist and a clinical psychologist. The patient’s checklists were collected, and NLP interventions were used to achieve these goals. The interventions were performed once a week for 8 consecutive weeks, and each session was conducted for 40 to 60 minutes. Interventions were trained in groups, and only in specific situations, it was possible to be trained in person.
3.1. Inclusion Criteria
Subjects aged 18 - 50 years, definitively diagnosed with depression, anxiety, and stress disorders by a psychiatrist, and filled out a consent form were enrolled in this study.
3.2. Exclusion Criteria
Pregnant women and subjects with a history of tDCS or NFB therapy for any disorder, epilepsy and seizures, substance abuse, intra-skull implants, and any other metal objects located in the head and mouth, as well as being under medical treatment and psychotherapy in the same time, were excluded from this study.
3.3. Tools Used in the Study
The Fars Ravan software package, SPSS version 23 (SPSS Inc, Chicago, Ill, USA), Depression Anxiety Stress Scales-21 (DASS-21) questionnaire, and SCID-5, as well as quantitative EEG, NFB, and tDCS devices, were used in this study.
3.3.1. Fars Ravan Software Package and Depression Anxiety Stress Scales-21 Questionnaire
Fars Ravan is a comprehensive software package designed for psychological tests; now, it includes more than 130 tests and questionnaires in different domains, used from the DASS-21 questionnaire in the present study. The most important advantage of this software package (in the context of the COVID-19 epidemic) is that the test results can be calculated and printed out instantaneously; also, the questionnaire can be sent online.
3.3.2. Quantitative Electroencephalography Device
In this study, 21 channels of an EEGA electroencephalography device (Medicam Company, Russia) were used; this device is used in EEG/quantitative EEG for studies, diagnosis, and treatment. In addition, The Neuroguide software package was used as one of the best and most complete medical software packages in the field of brain mapping and EEG/quantitative EEG analysis and evaluation.
3.3.3. Neurofeedback Device
The NFB device used in this study includes 2 pieces of ProComp hardware and a biograph software package (Thought Technology Company, Canada).
3.3.4. Transcranial Direct Current Stimulation Device
The ActivaDose device (ActivaTek Company, USA) was used in this study for tDCS.
3.3.5. Depression Anxiety Stress Scales-21 Questionnaire
DASS-21 is a standard questionnaire including 21 questions. In 1995, Lavibon designed and validated 21 items to assess the community’s anxiety rate, as well as to determine the level of stress, anxiety, and depression. The stability and validity of the Persian version were confirmed according to the Iranian population (30). The validity of the Persian version of the DASS-21 questionnaire was confirmed [Cronbach α = 0.91; intraclass correlation coefficient (ICC) = 0.74]. The questionnaire consists of 3 components; each component includes 7 questions, which the final result will be obtained through the sum of the scores of questions. To score the 4-part Likert Response Scale, each question was considered with the scale points of 0 (not at all to me) to 3 (quite true of me).
3.4. Data Analysis
Data analyses were performed by the multivariate analysis of covariance (MANCOVA) method using SPSS version 23.
4. Results
In this section, the descriptive data of subjects are first presented, and then the results of MANCOVA are shown to examine the effect of treatment intervention on the depression, anxiety, and stress of referred patients with psychological disorders to health centers.
4.1. Research Question
Is there a significant difference in the depression scores for tDCS, NFB, NLP, and control groups while controlling for their pretest scores on the test?
To respond to this question, MANCOVA was performed, and the results are presented in Table 1. It was noted that before performing the MANCOVA test, its assumptions (such as homogeneity of variances) using Leven’s test showed a higher significance level than 0.05, and Box’s test of equality of covariance matrices was evaluated (F1, 81 = 1.321; P = 0.163); thus, the assumption of homogeneity of variances was confirmed. The normal distribution assumption was therefore met, and it was possible to use MANCOVA.
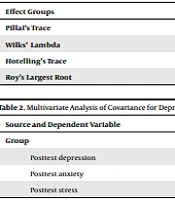
| Effect Groups | Value | F | Df1 | Df2 | P value | η2 |
|---|---|---|---|---|---|---|
| Pillai’s Trace | 1.564 | 19.252 | 9 | 159 | 0.0001 | 0.521 |
| Wilks’ Lambda | 0.040 | 38.194 | 9 | 124.27 | 0.0001 | 0.659 |
| Hotelling’s Trace | 10.198 | 56.276 | 9 | 149 | 0.0001 | 0.773 |
| Roy’s Largest Root | 8.751 | 154.610 | 3 | 53 | 0.0001 | 0.897 |
The results of MANCOVA tests in Table 1 show that the 4 groups (3 groups received treatment and a control group) were significantly different in at least 2 dependent variables (Wilks’ Lambda = 0.04; F9, 124 = 38.194; P = 0.01; η2 = 0.659) after controlling for pretests. To evaluate this difference, the tests of between-subjects effects of multivariable ANCOVA were used, and the results are presented in Table 2.
| Source and Dependent Variable | Type III Sum of Squares | Df | Mean Square | F | Sig. | η2 |
|---|---|---|---|---|---|---|
| Group | ||||||
| Posttest depression | 1059.501 | 3 | 353.167 | 59.182 | 0.0001 | 0.770 |
| Posttest anxiety | 953.168 | 3 | 317.723 | 123.278 | 0.0001 | 0.875 |
| Posttest stress | 918.226 | 3 | 306.075 | 110.570 | 0.0001 | 0.862 |
Table 2 shows that regarding pretest scores, intervention treatments resulted in a significant difference between the 3 experimental groups and the control group in terms of depression (F = 59.182; P < 0.01; η2 = 0.77). As η2 shows, the effect of treatment intervention was 77% and explained the posttest variance for depression scores. There was a significant difference between the 3 experimental groups and the control group concerning anxiety (F = 123.278; P < 0.01; η2 = 0.875). As η2 shows, the effect of treatment intervention was 87.5% and explained the posttest variance for anxiety scores, and eventually, there was a significant difference between the 3 experimental groups and the control group concerning stress (F = 110.57; P < 0.01; η2 = 0.862). As η2 shows, the effect of treatment intervention was 82.6% and explained the posttest variance for stress scores.
5. Discussion
In other words, the findings of this study illustrate that it is required a skilled psychiatrist and treatment team to make the methods effective in any condition. NFB requires proper training for the patient because the effect of the treatment method depends on the treatment protocol and its training. Further, to apply the NLP method, the psychologist and counselor should be able to have a quite good understanding of the situations, interventions, and NLP techniques. The psychologist should select patients with teamwork and collaborative effort for the NLP treatment method to have a remarkable and significant effect. Therefore, the patient should work closely with the counseling team and the therapist to use the techniques in the right situations with proper knowledge.
These results showed the effectiveness of tDCS on reducing depression, which were consistent with the results of Narimani et al. (2017), Csifcsak et al. (2018), da Silva et al. (2013), and Arul-Anandam and Loo (2009) (31-34). Moradi Kelardeh et al. (2016) concluded that tDCS therapy on the dorsolateral prefrontal cortex is the reason for reducing stress (35). In another study, Hashemi Nosratabad et al. (2016) concluded that stress declined when electrical stimulation increased the activity of the dorsal prefrontal cortex (36). Furthermore, they reported that tDCS reduced anxiety (36). Shiozawa et al. (2014) also concluded that direct current stimulation upon the skull reduced GAD (37). Moreover, in another study, Batista et al. (2015) reported that stimulation of the right or left prefrontal cortex reduced anxiety (38). Learning NLP techniques helps patients to overcome negative emotions in sensitive situations and control the situation.
Applying NFB therapy allows a person to control the quantitative parameters of EEG signal in operant conditioning, and in this way, a person can regulate the rhythms of his brain signal. During a process, a person learns how to control his brain signals, and it will be done with brain signal patterns. NFB is not a new process in the brain but is a natural biological process that can be controlled in this way (7). In addition, Gapen et al. (2016) showed that NFB is effective on PTSD (39). In this regard, Luctkar-Flude et al. (2019) showed that NFB affected psychological injuries, such as depression, anxiety, fatigue, stress, sleep problems, and pain in cancer patients (40).
Mennella et al. (2017) also found that NFB training on frontal lobe alpha wave asymmetry had an effect on reducing anxiety and negative affection (depression) in women (41). The results of Khoshsorour’s study (2018) showed that NFB had an effect on reducing anxiety and severity of symptoms in patients with irritable bowel syndrome (IBS) (42). Thus, no side effects have been reported by neuropsychology specialists after applying NFB and tDCS methods. Therefore, this method is recommended to psychology specialists of different fields, education professionals, school counselors, and parents. Considering researchers’ perspective, the improvement of NFB skills is not possible except by repetition and practice, and it is better to be replaced with drugs in many cognitive cases. Also, the present study has no follow-up period, and it is suggested that the follow-up period be repeated in 3 or 6 months in future studies.
5.1. Conclusion
Based on the findings, there was a significant difference between patients who were under treatment with NFB, NLP, and tDCS in terms of reduced stress, anxiety, and depression among both pretest and posttest groups. It seems that NLP, tDCS, and NFB methods are effective in reducing anxiety, stress, and depression. Considering the importance of the findings, non-pharmacological methods in the treatment of depression, anxiety, and stress could be effective.