1. Background
In Iran, 25,000 open heart surgeries are performed annually, of which about 50 - 60% are coronary artery bypass graft (CABG) (1). Despite recent advances in angioplasty, CABG is still the most common treatment and blood supply to the heart muscles (2). This surgical method is an efficient method to reduce or completely eliminate the symptoms of angina pectoris (3). Patients undergoing CABG will face serious problems in terms of their physical activity, nutrition pattern, degree of independence in daily life, immobility issues, respiratory complications, insufficient sleep, fatigue, and psychological problems such as anxiety and depression (4). Therefore, the ultimate goal in CABG surgery is the proper control of the disease by both the care team and the patient himself, as well as prevention of complications. The patient’s active participation in this process is necessary to create physical and mental adaptation in the patient (5).
Nurses, as important members of the treatment team, have an indisputable role to play not only in the processes of diagnosis, care, and rehabilitation but also in adapting the patients to the new situation and reducing their stress (6). The issue that should be considered in this regard is that achieving health in chronic diseases is possible by establishing adaptation in different dimensions of the patient. One of the practical and effective models in nursing specifically addressing this issue is Roy’s adaptation model (RAM) (7).
RAM extensively and deeply addresses the issue of physical adaptation in chronic diseases. According to this model, the goal of nursing is the individual’s adaptation in four modes (physiological, self-concept, role function, and independence-interdependence), and all nursing activities aimed at the development of the individual’s adaptation determine their health and illness (6). Application of this model has been reported to be effective in terms of psychological adaptation in chronic diseases such as diabetes mellitus (DM) (8) and chronic obstructive pulmonary disease (COPD) (9), as well as the quality of life (QOL) in patients with heart failure (10). The results of a study by Mansouri et al. showed that self-care trainings based on RAM facilitate adaptation in patients with heart failure in the four mentioned dimensions and improves their QOL (6).
The cardiology intensive care unit (ICU) is the locus of various physiological and psychological stimuli, and these stimuli are of paramount importance when it comes to CABG patients admitted to the ICU. Thus, the application of RAM can play an effective role in promoting the QOL of these patients (11). Despite the plethora of studies on patients undergoing CABG, few, if any, have adopted the RAM to achieve adaptive behavior in these patients with respect to their conditions and environment based on all dimensions of humans. Hence, there is a gap in the literature with respect to RAM (12). In addition, nursing care aimed at the adaptation of patients after CABG surgery is performed in all Iranian hospitals without following any specific framework. Given the prevalence of heart disease and the increase in the number of patients who are candidates for CABG surgery and considering the key elements in this model, it is important to take some measurements. This includes understanding the issues and problems of patients, becoming aware of the environment and systems around them, choosing a strategy appropriate to the patient adaptation, creating and developing a transformation program tailored to the client’s needs, and recognizing the key role of nursing training in this adaptation.
2. Objectives
This study was performed to determine the effect of care program based on RAM on the adaptation of patients undergoing CABG in ICU wards of Golestan and Imam Khomeini university hospitals in Ahvaz, southwest of Iran, in 2020.
3. Methods
3.1. Design
This was a quasi-experimental study conducted in 2020.
3.2. Sample
The study population included patients admitted to the ICUs of cardiology wards of Imam Khomeini Hospital and Golestan Hospital of Ahvaz, Iran, between September 1, 2020, and March 30, 2020. The sample size was determined using Med-calc statistical software with 95% power and a 5% error rate. Considering the 10% attrition rate, a total of 60 individuals were considered as the study subjects. Using the simple randomization method, the participants were divided into two equal groups of intervention and control (n = 30 each).
α = 0.05 →
The inclusion criteria were literate patients aged 40 - 65 years; no previous history of heart surgery; ability to participate in training sessions; and living in Ahvaz. Patients were excluded from the study if they had uncontrolled blood pressure or mental disorder, or if they did not participate in more than one training session during the intervention.
The study participants involved 60 patients admitted to the ICUs of the cardiology departments. To recruit the patients, a list of all eligible individuals was prepared, and then the researcher assigned a number from 1 to 60 to each participant. Afterward, using the simple randomization method, they were allocated into the intervention and control groups.
3.3. Instruments
In this study, the data collection tool was a questionnaire that included demographic characteristics and a RAM-based evaluation form (self-made). The demographic information questionnaire was a researcher-made questionnaire containing questions related to age, sex, weight, level of education, family history of heart disease, monthly income, marital status, duration of illness, ethnicity, and occupation. The RAM-based evaluation form is designed to examine the four dimensions of physiological, self-concept, role function, and independence, and interdependence. The physiological dimension includes eight subscales: respiration, nutrition, defecation, activity, excretion, rest, endocrine status, and liquids and electrolytes (25 questions). The scores range from 25 to 125, and higher scores indicate a better adaptation. The self-concept dimension includes three subscales: person, well-being of self, acknowledging the disease, sense of despair, guilt, and helplessness (13 questions). The scores range from 13 to 65, and higher scores indicate a better adaptation. The role function dimension includes spousal, social, parental roles, as well as sexual problems along with emotional and affective behaviors (10 questions). The scores range from 10 to 50, and higher scores indicate a better adaptation. For the independence and interdependence dimension, eight questions about daily and personal tasks independently, social support, and keeping relations with others and friends and relatives were investigated. The scores range from 8 to 40, and higher scores indicate a better adaptation. Each question was scored on a Likert scale from 1 to 5 (not at all = 1, rarely = 2, sometimes = 3, often = 4, always = 5). The score 5 represents the best situation, while the score 1 indicates the worst situation.
For validity, this questionnaire was provided to 10 professors at the faculty of nursing and midwifery at the authors’ institution, and their modifying ideas were applied in the questionnaire. In the present study, the reliability of the tool was measured as 0.85 (Cronbach’s α coefficient).
3.4. Intervention
After obtaining the necessary approval from the Ethics Committee and the Vice Chancellor for Research of Ahvaz University of Medical Sciences (Ref. ID: IR.AJUMS.REC.1399.611), the main researcher (AZ) attended the research environment, i.e., the cardiology ICUs of Imam Khomeini Hospital and Golestan Hospital. She introduced herself to the hospital officials by presenting a letter of introduction and provided a complete and accurate explanation of the research objectives. Before any intervention, the demographic information questionnaire and RAM-based evaluation form were completed by control and intervention groups. Then, for each member of the intervention group, four training sessions were held separately for one month, with each session lasting 60 minutes. Because the hospitalized patients were admitted to the ward for only ten days and were available there only in this period, the first two sessions of training were held in the hospital, while the other two sessions were conducted by telephone. The training program was conducted by one of the researchers holding an MSc in nursing. The first session of the training program involved training in relation to maladaptive behaviors and behavioral stimuli in the physiological dimension. This included understanding the nature of heart failure disease, its etiology, diagnosis, and treatment, understanding the side effects and consequences of medication in cardiovascular bypass disease, the introduction of food groups and cardiovascular diets, fluid intake, tobacco and alcohol consumption, weight gain, interpretation of daily weight in cardiovascular bypass, type of physical activity and its effect on heart failure, and symptom management. In the second session held one week later, the dimension of self-concept was discussed. This included topics such as methods to reduce and manage stress, control anger, and have regular sleep patterns, as well as methods to boost self-confidence and self-awareness. The third session involved training in relation to maladaptive behaviors and the stimuli of each behavior in terms of the role function dimension. This session was held through telephone and included spouse education, parent roles, sexual problems, and psychological stress, and how to cope with them. The fourth session involved training in relation to maladaptive behaviors and stimuli of each behavior in terms of the interdependence dimension. This involved encouraging patients to do their daily and personal activities independently, such as remembering the date of their visit to the doctor, seeing a doctor for checkups, knowing the time, dose, and method of the medications they use, and knowing what foods are harmful to them. The educational booklet entitled "Living with CABG" was prepared by the researcher and given to the intervention group. At the end of the training intervention, the questionnaires were again distributed among the subjects in both groups to examine whether the trainings were effective or not. In order to observe ethical considerations in this research, after the final evaluation, the training packages prepared by the research team were given to the patients in the control group.
3.5. Data Analysis
Data analysis was performed using SPSS ver. 22, descriptive statistics (mean, standard deviation, frequency, and percentage), independent t-test, paired t-test, and chi-square test. Also, the normality of the data was evaluated using the Kolmogorov-Smirnov test, and the significance level was considered P < 0.05.
4. Results
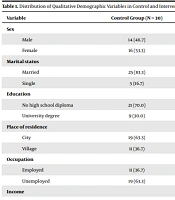
Data were collected and analyzed from 60 patients undergoing CABG surgery. The mean age of the participants was 65.68 ± 11.05 years. Nearly all patients (96.7%) reported a 1-to-2-year history of heart disease and a family history of heart disease. The results showed that the two groups were homogeneous in terms of quantitative and qualitative demographic variables, and there was no statistically significant difference between them (P < 0.05), except for the variable of having a family history (P = 0.023) (Tables 1 and 2). Also, the results of paired t-test (Table 3) showed that the mean score of the four dimensions of RAM in the intervention group significantly increased after the intervention (P < 0.05). Also, according to the results of the independent t-test, a significant difference was observed between the two groups after intervention in terms of the mean score of the four dimensions of RAM (P < 0.05).
| Variables | Control Group (N = 30) | Intervention Group (N = 30) | Total | Statistic | P-Value |
|---|---|---|---|---|---|
| Sex | 0.067 | 0.796 | |||
| Male | 14 (46.7) | 15 (50.0) | 29 (48.3) | ||
| Female | 16 (53.3) | 15 (50.0) | 31 (51.7) | ||
| Marital status | 0.13 | 0.718 | |||
| Married | 25 (83.3) | 26 (86.7) | 51 (85.0) | ||
| Single | 5 (16.7) | 4 (13.3) | 9 (15.0) | ||
| Education | 0.30 | 0.785 | |||
| No high school diploma | 21 (70.0) | 19 (63.3) | 40 (66.7) | ||
| University degree | 9 (30.0) | 11 (36.7) | 20 (33.3) | ||
| Place of residence | 0.30 | 0.785 | |||
| City | 19 (63.3) | 21 (70.0) | 40 (66.7) | ||
| Village | 11 (36.7) | 9 (30.0) | 20 (33.3) | ||
| Occupation | 0.07 | 0.791 | |||
| Employed | 11 (36.7) | 12 (40.0) | 23 (38.3) | ||
| Unemployed | 19 (63.3) | 18 (60.0) | 37 (61.7) | ||
| Income | 0.27 | 0.602 | |||
| < 2 | 14 (46.7) | 12 (40.0) | 26 (43.3) | ||
| > 2 | 16 (53.3) | 18 (60.0) | 34 (56.7) | ||
| Medical history | 2.96 | 0.195 | |||
| < 1 | 5 (16.7) | 1 (3.3) | 6 (10.0) | ||
| 1 - 2 | 25 (83.3) | 29 (96.7) | 54 (90.0) | ||
| Medical insurance | 1.07 | 0.313 | |||
| Yes | 29 (96.7) | 30 (100.0) | 59 (98.3) | ||
| No | 1 (3.3) | 0 (0.0) | 1 (1.7) | ||
| Family history | 5.19 | 0.023 | |||
| Yes | 23 (76.7) | 29 (96.7) | 52 (86.7) | ||
| No | 7 (23.3) | 1 (3.3) | 8 (13.3) | ||
| Seeking information | 3.16 | 0.076 | |||
| Yes | 27 (90.0) | 30 (100.0) | 57 (95.0) | ||
| No | 3 (10.0) | 0 (0.0) | 3 (3.0) | ||
| Sources of information | 3.68 | 0.575 | |||
| Health personnel | 2 (7.1) | 0 (0.0) | 2 (3.4) | ||
| People around | 7 (25.0) | 10 (33.3) | 17 (29.3) | ||
| Media | 10 (35.7) | 10 (33.3) | 20 (34.5) | ||
| Personal study | 8 (28.6) | 10 (33.3) | 18 (31.0) | ||
| Other | 1 (3.6) | 0 (0.0) | 1 (1.7) | ||
| Other diseases | 0.373 | 0.542 | |||
| Yes | 24 (80.0) | 22 (73.3) | 46 (76.7) | ||
| No | 6 (20.0) | 8 (26.7) | 14 (23.3) |
Distribution of Qualitative Demographic Variables in Control and Intervention Groups
| Group | Mean ± Standard Deviation | Statistics | P-Value |
|---|---|---|---|
| Age | -0.47 | 0.636 | |
| Control (N = 30) | 65.00 ± 11.98 | ||
| Intervention (N = 30) | 66.37 ± 10.18 | ||
| Total | 65.68 ± 11.05 | ||
| Weight | -0.67 | 0.506 | |
| Control (N = 30) | 70.97 ± 7.88 | ||
| Intervention (N = 30) | 72.17 ± 5.87 | ||
| Total | 71.57 ± 6.92 | ||
| Number of family members | -1.26 | 0.214 | |
| Control (N = 30) | 2.63 ± 1.87 | ||
| Intervention (N = 30) | 3.23 ± 1.83 | ||
| Total | 2.93 ± 1.85 | ||
| History of disease | -0.44 | 0.663 | |
| Control (N = 30) | 3.00 ± 1.80 | ||
| Intervention (N = 30) | 3.16 ± 1.05 | ||
| Total | 3.08 ± 1.46 |
Difference Between the Control and Intervention Groups in Terms of the Quantitative Demographic Variables
| Roy’s Adaptive Modes | Control | Intervention | Statistics | P-Value |
|---|---|---|---|---|
| Physiologic | ||||
| Before intervention | 50.13 ± 9.00 | 48.76 ± 6.36 | 0.68 | 0.500 |
| After intervention | 48.16 ± 4.00 | 101.26 ± 5.23 | -44.12 | 0.001 |
| Self-concept | ||||
| Before intervention | 28.46 ± 7.60 | 23.76 ± 4.10 | 2.98 | 0.005 |
| After intervention | 24.37 ± 4.06 | 50.80 ± 3.82 | -25.96 | 0.001 |
| Role function | ||||
| Before intervention | 23.36 ± 4.21 | 19.60 ± 2.93 | 4.02 | 0.001 |
| After intervention | 19.46 ± 2.94 | 39.10 ± 4.15 | -21.14 | 0.001 |
| Interdependence | ||||
| Before intervention | 25.33 ± 3.47 | 25.60 ± 3.54 | -0.29 | 0.769 |
| After intervention | 23.40 ± 2.89 | 25.47 ± 3.99 | -2.29 | 0.025 |
| Total adaptation | ||||
| Before intervention | 127.30 ± 19.00 | 117.73 ± 12.00 | 2.33 | 0.023 |
| After intervention | 115.40 ± 7.55 | 216.63 ± 7.88 | -50.77 | 0.001 |
Comparison of the Difference Between the Mean Scores of the Four Adaptive Modes of RAM and the Total Adaptation Score in Control and Intervention Groups Before and After the Intervention Based on RAM a
5. Discussion
The aim of this study was to determine the effect of a training program based on Roy’s nursing model on the level of adaptation of patients undergoing CABG in cardiology ICUs. There was no significant difference between the two groups of intervention and control in terms of demographic information, including gender, age, marital status, education, monthly income, previous history of the disease, and family history of heart disease. However, there was a significant difference between the two groups in the family history variable (P = 0.023). Therefore, it can be stated that the intervention was effective.
The first objective of the present study was to compare the physiological adaptation in the intervention and control groups before and after the intervention (Table 3). The results showed that there was no statistically significant difference between the two groups in terms of physiological adaptation before the intervention. However, after the intervention, there was a significant difference between the two groups in terms of physiological adaptation. In line with this finding, Mansouri et al. showed that training based on RAM could improve physiological symptoms in patients with heart failure (6). Also, the results of Akyil and Ergüney showed that teaching breathing control and relaxation techniques based on RAM could have a positive effect on the physiologic adaptation of patients with COPD (9). The results of another study showed that the implementation of training programs based on the RAM is effective on the psychological adaptation of patients with heart failure (13), which is consistent with the results of the present study.
Also, before the intervention, there was no statistically significant difference between the two groups in terms of their self-concept adaptation, but after the intervention, a significant difference was observed between the two groups in terms of this adaptive dimension. The results of Mansouri et al. showed that training based on RAM brings about self-concept adaptation in patients with heart failure (6). The results of Akyil and Ergüney also showed that stress management, relaxation training, and psychological support in the intervention group based on RAM had a positive and significant effect on self-concept adaptation in patients with COPD (9), which is consistent with the results of the present study. Given the fact that self-concept adaptation focuses on the psychological aspects of the individual and involves all the beliefs, feelings, and thoughts of the patient, using this model in nursing care is an effective step to improve the mental state of patients undergoing surgery.
The findings of the present study showed that before the intervention, there was no statistically significant difference between the two groups in terms of role function adaptation, but after the intervention, there was a significant difference between the two groups in terms of this dimension. This was in line with the results of Mansouri et al., which reported the positive effect of training based on RAM on the role function adaptation of heart patients (6). Afrasiabifar et al. investigated the same effect among patients undergoing hemodialysis and found a significant improvement in the role function adaptation in the intervention group after training (14).
Regarding interdependence adaptation, the results of this study showed that before the intervention, there was no statistically significant difference between the two groups, but after the intervention, a statistically significant difference was observed between the two groups. In this line of research, Larsen and Pedersen studied the effectiveness of individual rehabilitation in patients with heart failure. They found that conducting a rehabilitation program in the intervention group and their follow-up for 12 weeks increased the mean score of social functioning (15). Also, Abdollahi et al. reported that a care program designed based on RAM to increase the ability to perform daily activities in patients with heart failure was useful and beneficial (16), which is consistent with the results of the present study. Therefore, the RAM is recommended as a low-cost, non-invasive, and effective method in providing nursing care to enhance patients’ interdependence in performing daily activities.
The main limitations of this study were the small sample size and conducting the intervention in only two hospitals, which may affect the generalizability of our findings. Therefore, similar studies with larger sample sizes and in different hospitals are recommended.
5.1. Conclusions
Given the results of the present study and those of the most studies conducted on RAM, it should be stated that this model can provide a suitable framework for examining, caring for, and performing surgical interventions on those suffering from chronic diseases and controlling their disease. The application of training programs based on this model can increase the level of adaptation of patients with coronary artery disease undergoing bypass surgery and subsequently improve their QOL.