1. Context
Coronavirus 2019 (COVID-19) was detected on December 31, 2019 in Wuhan, China, and quickly put the world in a state of crisis and high alert until the World Health Organization on March 11, 2020, identified COVID-19 as a pandemic (1). COVID-19 mainly affects the respiratory and digestive systems, and the most common symptoms are fever, dry cough, shortness of breath, and body pain (2). In response to epidemics, most countries have imposed quarantine, social distancing, restrictions on long-distance travel, closure of schools and universities, and closure of unnecessary jobs (3). The effectiveness of social distancing has been proven to control and reduce virus transmission, but these limitations have numerous negative psychological, familial, and economic consequences for vulnerable groups, such as those with a chronic disease (4).
Studies have shown that the COVID-19 pandemic has a significant impact on the mental health of people chronic diseases (5, 6). Patients with a chronic disease during the COVID-19 pandemic need more psychological support in addition to physical care. Many of these people experience extra stress because they are told they are vulnerable and need further care. Therefore, if they do not receive timely interventions, they might suffer from irreversible depression and anxiety (7). In this regard, one of the chronic diseases that affected COVID-19 is fibromyalgia (8). Fibromyalgia is a common and debilitating syndrome characterized by diffuse and multifaceted musculoskeletal pain, the presence of multiple and unstable points sensitive to pain, sleep disturbance, fatigue, and muscle inflexibility (9). Disseminated pain in the body is a characteristic feature of the disease, which may be described by terms such as sharp and burning, throbbing, shooting, blurred and deep, or tingling and numbness (10). These patients have a lower pain tolerance range than healthy individuals, a non-painful stimulus causing pain and a painful stimulus stimulating too much pain are the common responses in these patients (11).
Pain is the most common complaint in these patients; most patients present with vague, diffuse pain and nonspecific muscle pain. Accompanying symptoms such as morning dryness, fatigue and headache are also common (12). The risk is higher in women than men and increases with age, such that it reaches its maximum at the age of 55 - 79 (13). Studies conducted during the COVID-19 pandemic indicate a higher prevalence of fibromyalgia symptoms in patients (14), and it is expected that in the post-COVID-19 period, we will see a significant growth of this chronic disease worldwide (15, 16). Various studies indicate a high prevalence of mental disorders in patients with fibromyalgia (17, 18). Stress and anxiety are the most common psychological comorbidities in patients with fibromyalgia. Perceived anxiety and stress seem to be one of the triggering factors in this syndrome (19).
High levels of fatigue and anxiety resulting from quarantine conditions significantly increase the need for extreme self-care in fibromyalgia patients, but due to the lack of a definitive treatment for COVID-19, the person might fail to respond to this need (20, 21). In this regard, Salaffi et al. (22), in a study, investigated the effects of the prevalence of COVID-19 on mental health and quality of life of fibromyalgia patients. The results showed that during the COVID-19 pandemic, fibromyalgia patients had high levels of stress, depression, and anxiety. Also, the quality of sleep, quality of life, and the treatment process of patients with fibromyalgia were significantly undermined. In another study, Schweiger et al. (23) examined the psychological consequences of the COVID-19 pandemic in fibromyalgia patients. The results of this study showed that 72.7% of patients had a high level of psychological distress during the outbreak of COVID-19. Also, due to social distancing and COVID-19 pandemic, patients' quality of life was significantly reduced. All of these cases increased the severity of chronic pain in patients. A study by Hruschak et al. (24) also showed that the mental health of patients with chronic pain decreased significantly during the COVID-19 outbreak. Also, economic conditions, gender, marital status, and age were significantly associated with patients' pain intensity. Women and people with low level of education were more anxious and depressed.
Two years after the outbreak of COVID-19, mutations in this deadly virus are still being detected, and the world's most reputable vaccines are also vulnerable to some mutations. Fibromyalgia patients also experience a lot of anxiety, depression, and stress during this period, which reduces their quality of life and leads to the recurrence of the disease (25, 26). For this reason, in addition to physical health, it is necessary to pay attention to the psychological dimensions of these patients to see a reduction in their mental disorders in the coming years.
2. Objectives
The present review study was conducted to investigate the psychological consequences of the COVID-19 pandemic in fibromyalgia patients.
3. Data Sources
The present study was a systematic review that examined the research findings related to the psychological consequences of the COVID-19 pandemic in patients with fibromyalgia through the PRISMA model (27). In the present review study, during August and September, the CINAHL, MEDLINE Complete, Cochrane, EMBASE, PsycINFO, Google Scholar, PubMed, ISI, Scopus, and ScienceDirect databases were searched using the following keyword for articles published during February 2020-July 2021.
4. Study Selection
4.1. Keywords
The combinations of the following MeSH-based keywords were used in the search strategy: (Fibromyalgia) (title/abstract) AND (Chronic disease) (title /abstract). (Coronavirus 2019) OR (COVID-19) (title/abstract) AND (Pandemic) OR (Epidemic) (title/abstract) AND (Anxiety) OR (Depression) OR (Stress) OR (Mental Health) OR (Psychology) (title/abstract).
4.2. Exclusion and Inclusion Criteria
Research articles were purposefully selected based on the exclusion (unavailability of full text of the article, letter to the editor, and no abstract) and inclusion (relevance to the purpose of the research, having a structured research framework, and publication in a valid journal) criteria.
4.3. Quality Assessment
All articles, after being extracted from the databases, were evaluated by three researchers using specialized keywords. In order to further improve the quality of the articles, after removing the articles that were not related to the research objectives and selecting the main articles, the references list of the selected articles was searched. Three researchers separately analyzed the content of each of the 12 articles. Also, Farzin…., Hojjatollah…., and Parviz …..studied each article separately and then entered the data related to each article in the content analysis form. In order to resolve possible disagreements, the inclusion criteria were emphasized in the analysis process. To enter the analysis process, the quality of articles was evaluated using the criteria provided by Gifford et al. (28). Based on the criteria provided for quantitative (6 criteria), qualitative (11 criteria), quasi-experimental (8 criteria), and experimental (7 criteria) studies, the articles were evaluated on a two-point scale (zero and one). The cut-off point was 4 and less for quantitative articles, 6 and less for experimental and quasi-experimental studies, and 8 and less for qualitative studies.
5. Data Extraction
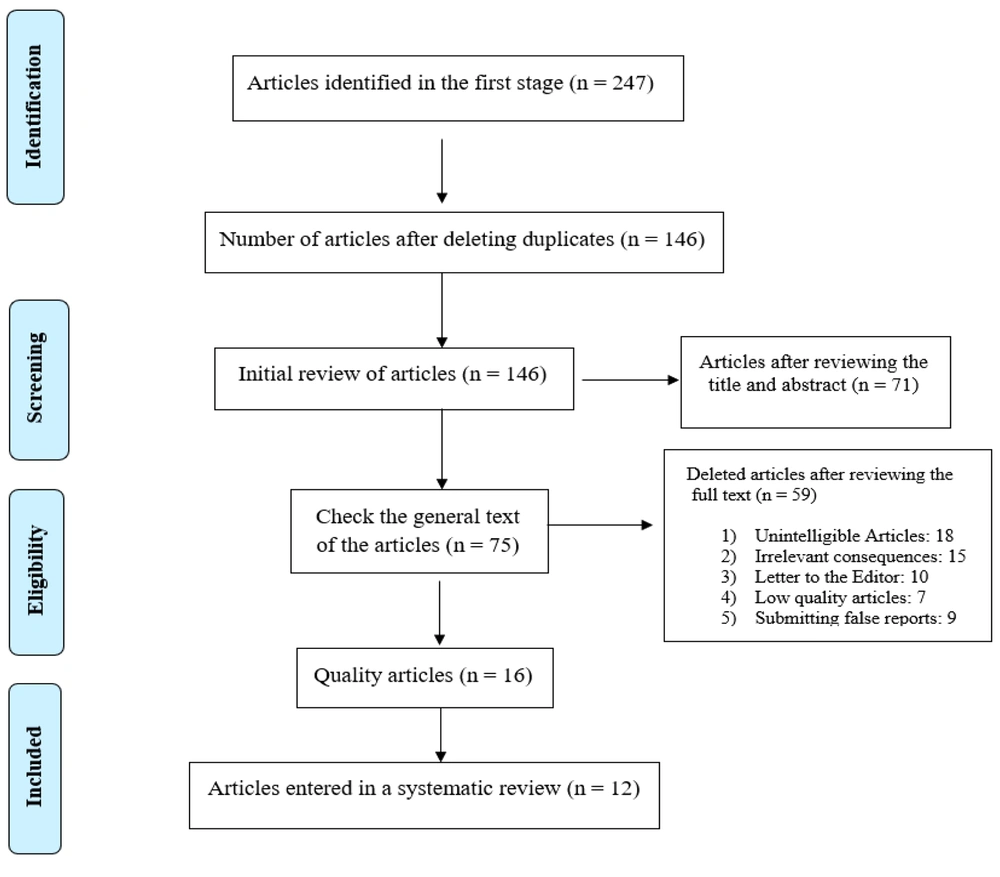
Out of 247 articles related to the psychological consequences of the COVID-19 pandemic in patients with fibromyalgia, after deleting articles that were not related to the objectives of the study, 12 completely related articles were included and thoroughly studied (Figure 1).
6. Results
In this study, 12 eligible English-language articles were reviewed. The following are the findings from peer-reviewed articles on the psychological consequences of the COVID-19 pandemic in patients with fibromyalgia (Table 1).
| Authors | Psychological Problems | Purpose | Sample | Country | Results |
|---|---|---|---|---|---|
| Serrat et al. (6) | Depression, anxiety, and stress | Efficacy of the FIBROWALK for patients with fibromyalgia during the COVID-19 | 151 patients with fibromyalgia | Spain | Studies have shown that many fibromyalgia patients experience a lot of depression, anxiety, and stress during the outbreak of COVID-19. According to the findings, people who received FIBROWALK treatment were in better mental health than the control group. |
| Iannuccelli et al. (8) | Depression and anxiety | Mental health and well-being fibromyalgia and RA during the COVID-19 | 72 fibromyalgia | Italy | The results showed that the levels of anxiety and depression in patients with fibromyalgia were 36.7% and 50%. Fibromyalgia patients had more problems during the prevalence of COVID-19 than patients with rheumatoid arthritis. |
| Worcester et al. (17) | Depression | Increased depression in fibromyalgia patients during the COVID-19 | 69 patients with fibromyalgia | Australia | The results showed that during the COVID-19 pandemic, the amount of physical activity, mental health, and sleep quality of fibromyalgia patients decreased significantly. Patients' medication intake also increased. 10% of patients suffered from severe depression. |
| Cankurtaran et al. (20) | Anxiety | COVID-19 fear and anxiety on symptom severity, sleep quality, and mood in patients with fibromyalgia | FM patient (31) and control group (31) | Turkey | The results of this study showed that fibromyalgia patients have lower quality of sleep, anxiety, and mood compared to healthy individuals. Fibromyalgia patients were also found to have more chronic pain during the COVID-19 pandemic. |
| Kharko et al. (21) | Anxiety | Anxiety and pain of fibromyalgia patients during the COVID-19 | 58 fibromyalgia | England | The results showed the prevalence of anxiety and chronic pain during the prevalence of COVID-19 in women with fibromyalgia. Many patients experienced high levels of depression and anxiety due to poor financial status, lack of access to a doctor, inability to obtain medication, and social isolation. |
| Salaffi et al. (22) | Stress, depression, and anxiety | Effect of COVID-19 on fibromyalgia | 897 patients with fibromyalgia | Italy | The results showed that during the COVID-19 pandemic, fibromyalgia patients had high stress, depression, and anxiety. Also, the quality of sleep, quality of life, and the process of treatment of people with fibromyalgia were significantly reduced. |
| Schweiger et al. (23) | Psychological distress | Quality of life and psychological assessment in patients with fibromyalgia during COVID-19 | 37 patients with fibromyalgia | Italy | The results of this study showed that 72.7% of patients had a high level of psychological distress during the outbreak of COVID-19. Also, due to social distancing and COVID-19 pandemic, patients' quality of life was significantly reduced. All of these cases increased the severity of chronic pain in patients. The use of effective coping strategies also led to an improvement in patients' quality of life. |
| Hruschak et al. (24) | Mental health | Psychosocial and pain-related variables among patients with chronic pain during COVID-19 | 150 patients with fibromyalgia, chronic spine, and postsurgical pain | U.S. A | Studies have shown that the mental health of patients with chronic pain during the prevalence of COVID-19 was significantly reduced. Fibromyalgia patients experienced more pain. Also, economic conditions, gender, marital status, and age were significantly associated with patients' pain intensity. Women and people with low education were more anxious and depressed. |
| Gheita et al. (25) | Anxiety and depression | Psychological dimensions of COVID-19 in fibromyalgia patients | 3 females fibromyalgia | Egypt | The findings showed the prevalence of anxiety, depression, headache, muscle aches, and poor sleep quality during the COVID-19 pandemic in fibromyalgia patients. Due to the stress, they had, the patients became physically fit, which made them afraid of developing COVID-19. |
| Ursini et al. (26) | Anxiety and fear | Consequences of COVID-19in fibromyalgia patients | 616 | ||
| FM patient | Italy | Studies have shown that patients with fibromyalgia are at high risk for COVID-19. This fact increased their anxiety and fear. Overweight and gender also affect the risk of developing fibromyalgia in patients with fibromyalgia. | |||
| Colas et al. (29) | Depression | Experiences of fibromyalgia patients during COVID-19 | 19 patients with fibromyalgia | France | The COVID-19 pandemic exacerbated the disease in people with fibromyalgia. Also, 68% of patients reported a decrease in physical activity, which reduced their quality of life. Social distancing also increased patients' feelings of loneliness and depression. |
| Serrano‐Ibanez et al. (30) | Anxiety and stress | Chronic pain in the time of COVID‐19 | 362 fibromyalgia, chronic widespread pain, low back pain | Spain | The results showed an increase in the severity of the disease and pain during the outbreak of COVID-19 in people with chronic pain. Factors such as old age, difficult access to a doctor and medication, lack of social support, and being a woman were also associated with anxiety and stress. |
Out of 247 articles related to the psychological consequences of the COVID-19 pandemic in patients with fibromyalgia, 12 articles were reviewed, and a population of 2496 people were selected and reviewed based on the inclusion and exclusion criteria. Italy, England, the USA, Egypt, France, Spain, Australia, and Turkey were also present at the systematic review. The studies showed that patients with fibromyalgia had high levels of depression, anxiety, stress, and fear during the COVID-19 pandemic. Factors such as age, female gender, low level of education, poor sleep quality, marital status, financial status, and loneliness were associated with psychological distress and the exacerbation of symptoms in fibromyalgia patients. In contrast, social support and the use of effective coping strategies led to improved quality of life and mental health of patients. According to the results of studies, many patients with chronic pain, including fibromyalgia patients, had poor mental health, quality of life, social relationships, and sleep quality during the COVID-19 pandemic, which caused the recurrence of the disease and increased anxiety and depression in them. In this regard, to increase the psychological health of fibromyalgia patients, studies have suggested the use of FIBROWALK and tele-mental health treatment programs during the outbreak of pandemic diseases.
7. Discussion
This review study aimed to investigate the psychological consequences of the COVID-19 pandemic in patients with fibromyalgia. The results showed that patients with fibromyalgia had high levels of depression, anxiety, stress, and fear during the COVID-19 pandemic. Factors such as age, female gender, low education, poor sleep quality, marital status, financial status, and loneliness were associated with psychological distress and the exacerbation of symptoms in fibromyalgia patients. In contrast, social support and the use of effective coping strategies led to improved quality of life and mental health of patients (22-25).
It can be stated that patients with fibromyalgia are known to be vulnerable to COVID-19 because they have a weaker immune system (20). This has caused many patients to suffer from severe fear and anxiety about COVID-19 and limit their social interactions (8). These patients had poor quality of life, social relationships, and quality of sleep, which caused a recurrence of the disease and increased anxiety and depression in them (22). In this regard, Colas et al. (29) examined the experiences of fibromyalgia patients during the COVID-19 pandemic. Their results showed that the COVID-19 pandemic exacerbated the disease in people with fibromyalgia. Also, 68% of patients reported a diminution in physical activity, which reduced their quality of life. Social distancing also intensified patients' feelings of loneliness and depression.
Since one of the main causes of fibromyalgia is psychological factors (15), during the COVID-19 pandemic, fibromyalgia patients showed a significant increase in pain intensity due to increased anxiety and stress (23). Pain is the most characteristic symptom of fibromyalgia and affects many aspects of a person's life and is associated with disruption of daily and normal activities, changes in the ability to work, inhibition of adequate sleep, and dissatisfaction with life (12). Pain and a feeling of uncontrollability, when accompanied by catastrophic thoughts, cause depression, and the more depressed the patient's mood, the lower the pain tolerance threshold (20-23). Various studies indicate the high prevalence of mental disorders in patients with fibromyalgia, and depression is one of the most common psychological comorbidities in such patients (11). Living with chronic pain exerts considerable emotional pressure, such that patients' emotional abilities are reduced and ultimately lead to helplessness and depression (19). During the COVID-19 pandemic, the pain and physical disability caused by fibromyalgia disrupted personal activities and dysfunction in many patients, which reduced their mental health and quality of life (21). In the same study, Serrano‐Ibanez et al. (30) studied the chronic pain of fibromyalgia patients during the COVID-19 pandemic. The results showed an increase in the severity of the disease and pain during the outbreak of COVID-19 in those with chronic pain. Factors such as old age, difficult access to a doctor and medications, lack of social support, and female gender were also associated with anxiety and stress.
During the COVID-19 pandemic, in addition to fibromyalgia, a variety of secondary factors such as age, female gender, low level of education, poor sleep quality, marital status, financial status, and loneliness affected patients’ mental health (17-25). For this reason, in addition to the mental health of fibromyalgia patients, it is necessary to pay further attention to the individual differences and lifestyle of these patients to promote the psychological health of fibromyalgia patients during the COVID-19 pandemic (14-16).
One of the limitations of the present review study is the unavailability of the full text of some articles, which led to the exclusion of these articles in the review process. Also, due to the filtering of some scientific databases, researchers could not access them. In addition, some studies were descriptive and cautious should be exercised in generalizing their results. In this regard, it is suggested that descriptive studies be conducted on the psychological consequences of the prevalence of COVID-19 in fibromyalgia patients in Iran to identify the significant role of these factors in improving the physical and psychological functions of fibromyalgia patients in Iran.
7.1. Conclusions
Overall, studies have shown that patients with fibromyalgia suffer from depression, anxiety, stress, fear, poor sleep quality, and loneliness during the COVID-19 pandemic, which affects their mental health and quality of life. Since the beginning of the COVID-19 pandemic, it was announced that people with chronic diseases are among the groups vulnerable to COVID-19. Hence, many patients experienced severe depression and anxiety during the pandemic. This psychological pressure has affected the treatment process of many chronic diseases, including fibromyalgia. During this period, efforts of all countries and global institutions are now focused on the production of vaccines and drugs to treat this disease, which is certainly a necessary step, but the psychological aspects of this challenge do not seem to have received adequate attention. For this purpose, it is necessary to adopt psychological interventions by identifying vulnerable patients to reduce their pain and promote their mental health.