1. Background
According to the literature, type 2 diabetes mellitus (T2DM) is an epidemic metabolic disease that affects about 7% to 8% of the world’s adult population. According to the International Diabetes Federation, this figure is estimated to reach 693 million by 2045 (1, 2). Diabetes mellitus and its related problems and complications (such as macro- and microvascular complications) lead to a decline in health-related quality of life (3). Quality of life is defined as people’s perception of their position with respect to their accepted goals and value systems, given the objective conditions of life. Quality of life in diabetic patients can be influenced by many factors, some of which are diet, diabetes distress, self-care, drug regimen, physical activity, psychological status, and the role of the family in care and treatment (4).
The results of the study by Tol et al. showed that the quality of life of diabetic patients had a significant relationship with diabetes distress; they also reported that the relationship between self-care and quality of life was significant (5). Diabetes distress is an emotional state in which the person has concern and anxiety arising from diabetes. This condition has a mild to severe spectrum, and in addition to physical complications, it causes mental disorders. In this regard, diagnostic methods and strict treatment and healthcare plans can contribute to diabetes distress (6).
Diabetes distress is often accompanied by frustration caused by ongoing dietary commitments, reduced physical activity, and reduced monitoring of the consumption of glucose and medications (7). The results of Mahdiyah and Rifka showed that diabetic patients developed diabetes distress due to fear of complications of diabetes, changes in lifestyle/economic status, and long-term treatment. In this respect, self-care education has been reported to reduce the complications of diabetes and improve the quality of life (6). Several studies have shown that inadequate self-care in diabetes accounts for emotional and behavioral stress and that fear of diabetes complications as a major stressor and cause of diabetes distress affects health and reduces quality of life (8). Self-care behaviors include proper, principled, and regular use of medication, blood sugar control and monitoring, proper diet to control blood sugar, exercise, and proper physical activity (9). These behaviors lead to improved quality of life (10). Non-adherence or poor adherence to self-care behaviors, on the other hand, leads to complications and increased mortality (11).
Finally, it should be noted that since quality of life is a multidimensional concept, various tools are used to analyze the data related to it. Structural equation modeling (SEM) is known as the most general and complete statistical tool used to determine the direction and intensity of the hidden effects between variables. The use of SEM in nursing studies shows their strengths and limitations, and based on the results, this modeling offers practical guidelines and realistic plans for future research (8).
2. Objectives
This study aimed to design a structural equation model of the effect of diabetes distress and self-care activities (predictive variables) on T2DM patients’ quality of life (an outcome of diabetes).
3. Methods
3.1. Design
This research is a descriptive-analytical study.
3.2. Sample
The study population included patients with T2DM referred to medical centers affiliated with Ahvaz Jundishapur University of Medical Sciences in 2020. In order to calculate the sample size, the sample size formula for structural equations was used. as well as 50 observational variables in three questionnaire, 380 T2DM patients were studied as research samples (12).
Inclusion criteria were age over 18 years, history of T2DM at least 1 year before the start of the study, taking oral medications or insulin or both for T2DM, having the ability to read and write in Persian, and giving consent to participate in the study. Patients with gestational diabetes or mental disorders and those who failed to complete questionnaires were excluded from the study.
3.3. Instruments
Data collection tools in this study included 3 questionnaires and a form used to record the patients’ demographic characteristics (including age, sex, education, ethnicity, economic status, duration of diabetes, and type of treatment).
The first questionnaire was Problem Areas in Diabetes Scale (PAID), used to identify depression and emotional stress associated with diabetes. This questionnaire includes 20 questions in 4 subscales (emotional problems, treatment barriers, food-related problems, and social support) (13). The scoring of PAID-20 is based on a 5-point Likert from 0 (no problem) to 4 (serious problem). The total score of the 20 questions is multiplied by 1.25, and the final score will be between 0 and 100. The higher the score, the more distress experienced by the patient. A score equal to or greater than 33 indicates emotional stress, and a score of 38 or higher indicates possible depression (13, 14). The reliability of this questionnaire was calculated by Arzaghi et al. obtained a Cronbach α coefficient of 0.94 (15).
The second questionnaire used in this study was Audit of Diabetes-Dependent Quality of Life 19 (ADDQoL-19). This questionnaire includes 19 2-part items related to the physical, mental, and social status of patients. The items of this questionnaire are scored based on 4- and 5-point Likert scales. Physical function domain scores range from 6 to 30, social domain scores from 9 to 45, and mental domain scores from 6 to 30. The total score of quality of life is between 19 and 95 (14). The impact of diabetes on quality of life in each item ranges from -3 (extremely worse) to +3 (extremely better), and in terms of importance, each item is scored based on a scale from 0 (not at all important) to 3 (very important). The final score of this tool measures the quality of life of diabetic patients (16). Both ranges are then multiplied and added together, and their mean is calculated. According to the above analysis, the more negative the score, the lower the quality of life (14, 16). Hirose et al. evaluated the reliability of this questionnaire and obtained a Cronbach α of 0.933 (17).
The third questionnaire used in this study was the Summary of Diabetes Self-care Activities. This questionnaire is a short self-report tool to assess the self-care behaviors of diabetic patients and includes 11 items in the areas of general diet, specific diet, exercise, blood-glucose testing, foot care, and taking medications. Each item is given a score of 0 - 7 depending on the number of times the patient has engaged in a self-care activity in the previous 7 days, with the overall score of the questionnaire ranging from 0 - 77. There are 4 items for nutritional behaviors, 2 items for exercise, 2 items for blood sugar control, 2 items for foot care behaviors, and 1 item for smoking (18). This questionnaire was translated into Persian, and its validity was measured by confirmatory factor analysis, and a Cronbach α coefficient of 0.77 was obtained for its reliability.
3.4. Data Collection
After obtaining approval from the Ethics Committee and Vice Chancellor for Research and Technology of Ahvaz University of Medical Sciences (Ref ID: IR.AJUMS.REC.1398.741), the researcher (Akbari) went to the research environment, and after introducing herself, she provided a complete and accurate explanation of the research objectives to the relevant officials. Next, the study participants were briefed on the research objectives, confidentiality of their personal information, and their right to withdraw from the study at any stage; then, a written informed consent was approved by the ethics committee of Ahvaz University of Medical Sciences was obtained from them.
3.5. Data Analysis
In this study, SPSS version 26 (SPSS Inc, Chicago, Ill, USA), Hayes PROCESS macro version 3.5, and the statistical method of path analysis were used for statistical analysis. The significance level was set at P < 0.05.
4. Results
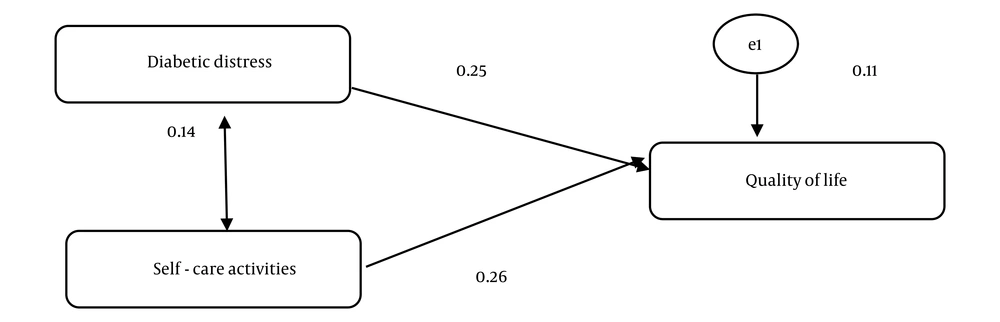
In this study, data were collected from 400 T2DM patients, but 2 patients were excluded from the study due to incomplete questionnaires. Therefore, data analysis was performed on 398 T2DM patients. In the present study, 56.3% of the patients were male, 74.6% were married, 27.1% were housewives, 75.9% had urban residence, 46% had a high school diploma, 42.2% had macrovascular complications, and 41.2% were on oral medication (Table 1). Also, the mean scores of diabetes distress, self-care activities, and quality of life in our diabetic patients were 81.98 ± 15.20, 65.57 ± 11.11, and 56.94 ± 18.62, respectively (Table 2). Also, the relationship between diabetes distress variables, self-care activities, and quality of life in T2DM patients is shown in Tables 3 and 4 and Figure 1.
| Variables | No. (%) |
|---|---|
| Sex | |
| Female | 174 (43.7) |
| Male | 224 (56.3) |
| Marital status | |
| Single | 55 (13.8) |
| Married | 297 (74.6) |
| Widow(er) | 38 (9.5) |
| Divorced | 8 (2) |
| Employment | |
| Office worker | 94 (23.6) |
| Worker | 26 (6.5) |
| Farmer | 27 (6.8) |
| Housewife | 108 (27.1) |
| Self-employed | 84 (21.1) |
| Retired | 37 (9.3) |
| Unemployed | 22 (5.5) |
| Education | |
| Illiterate | 11 (2.8) |
| Junior high school | 97 (24.4) |
| High school diploma | 183 (46) |
| University degree | 107 (26.9) |
| History of the disease (y) | |
| > 1 | 7 (1.8) |
| 1 - 5 | 132 (33.2) |
| 6 - 10 | 149 (37.4) |
| < 10 | 110 (27.6) |
| Complications | |
| Nil | 73 (18.3) |
| Micro | 168 (42.2) |
| Macro | 65 (16.3) |
| Micro + Macro | 92 (23.2) |
| Type of treatment | |
| Oral medication | 164 (41.2) |
| Insulin | 140 (35.2) |
| Oral medication + Insulin | 94 (23.6) |
| Income (IRR) | |
| > 20 000 000 | 129 (32.4) |
| < 20 000 000 | 267 (67.6) |
| Residence | |
| Urban | 302 (75.9) |
| Rural | 96 (23.6) |
| Age (y), mean ± SD | 63.39 ± 29.57 |
| Weight (kg), mean ± SD | 74.62 ± 11.52 |
Frequency Distribution and Percentage of Demographic Characteristics of the Type 2 Diabetes Mellitus Patients
| Variables | Mean ± SD | Statistical Test |
|---|---|---|
| Diabetes distress | 15.20 ± 81.98 | Path analysis regression |
| Self-care activities | 12.11 ± 65.57 | |
| Quality of life | 18.62 ± 56.94 |
Mean Score of Diabetes Distress, Self-care Activities, and Quality of Life of the Type 2 Diabetes Mellitus Patients
| Variables | Estimate | P-Value | Test |
|---|---|---|---|
| Diabetes distress/quality of life | -0.249 | < 0.001 | Path analysis regression |
| Self-care activities/quality of life | 0.183 | < 0.001 | |
| Diabetes distress/self-care activities | 0.138 | < 0.006 |
Relationship Between Diabetes Distress Variables, Self-care Activities, and Quality of Life in Patients with Type 2 Diabetes Mellitus
According to Table 3, for every 1-unit increase in the score of diabetes distress, the quality of life score of the T2DM patients decreased by about 0.249 (P < 0.001). Also, for every 1-unit increase in the score of self-care activities, the quality of life score of the T2DM patients increased by approximately 0.183 (P < 0.001). Diabetes distress has a covariance of 0.14 with self-care activities. That is, if the score of self-care activities increases, the score of diabetes distress increases by 0.138 (P < 0.006).
| Variables | TLI | IFI | CFI |
|---|---|---|---|
| Value | 1.000 | 1.000 | 1.000 |
Quality of Life of the Type 2 Diabetes Mellitus Patients Based on Diabetes Distress and Self-care Activities Using the Goodness of Fit Test
To evaluate the goodness of fit, the model was saturated, and all variables of quality of life, diabetes distress, and self-care activities were correlated according to the table above and the model below.
5. Discussion
The aim of this study was to investigate the effect of diabetes distress and self-care activities on the quality of life of T2DM patients. The mean score of diabetes distress was moderate to severe in our T2DM patients. Consistent with the findings of the present study, the mean score of diabetes distress obtained by Tol et al. was moderate (5). Mirzaei et al. found that 45.6% of their patients had stress, indicating a high prevalence of stress in their study, which is consistent with the findings of the present study (19). It can be argued that diabetes distress is prevalent among T2DM patients and is accompanied by a wide range of problems in these patients, ranging from tragic problems to ongoing self-care needs, such as continuous glycemic control, medication, insulin injection, food intake control, and regular physical activity (20). Therefore, it is essential to provide training to reduce this distress and associated emotional problems in these patients. Also, the mean score of self-care activities in our T2DM patients indicates that the level of self-care activities and behaviors of these patients is relatively desirable. Self-care behaviors play a vital role in preventing and improving the symptoms of the disease; health educators must first identify these factors to promote patients’ self-care behaviors. After taking into account these factors, they can formulate training programs and interventions.
In this study, the mean score of diabetes-dependent quality of life indicates a relatively good quality of life in our T2DM patients. The results of Krzeminska et al. showed that ADDQoL in T2DM patients in Poland, the Czech Republic, and Slovakia was good or very good (21). Further, “good,” “very good,” and “excellent” levels of the present general quality of life were declared by 65% of women and 52% of men with T2DM in Bak et al. study (22).
According to the results of the present study, for every 1-unit increase in the score of diabetes distress, the quality of life score of T2DM patients decreased by about 0.249 (P < 0.001). This means that the higher the rate of distress and its associated problems in these patients, the lower their quality of life. Our results also showed that for every 1-unit increase in the score of self-care activities, the quality of life score of T2DM patients increased by about 0.183 (P < 0.001). This means that promoting self-care activities and behaviors of diabetic patients enhances their quality of life. In this respect, Cherrington et al. found that diabetic patients’ self-care activities reduce depressive symptoms and thus help to improve the quality of life in these patients (23).
Further, Mishali et al. showed that self-care of diabetic patients plays a role in their adherence to treatment and diabetes control and that it is necessary to include self-care assessment in the first stage of designing interventions, which in turn can improve patients’ quality of life (24). Therefore, refraining from self-care activities increases the likelihood of diabetes-associated complications. These complications will consequently have a great impact on the quality of life of the individual and family and impose high economic burdens on individuals and society. Thus, as far as future planning for diabetes education and control is concerned, it is wise to invest in self-care activities and improving patients’ quality of life.
In the present study, diabetes distress had a covariance of 0.14 with self-care activities. That is, if the score of self-care activities increases, the score of diabetes distress increases by 0.138 (P < 0.006). In other words, as patients’ diabetes distress increases, so do their self-care activities. In line with this finding, the results of a study showed that problems such as diabetes distress are very common in diabetic patients and have a significant impact on diabetes self-care activities (25). Javadi et al. examined the relationship between self-care and emotional distress (diabetes distress) in diabetic patients. They found that the levels of distress and self-care activities in these patients were moderate and that there was a significant negative correlation between the 2 variables, such that increasing diabetes distress reduces patients’ self-care activities (26), which is different from the results of the present study. In order to explain this discrepancy, it should be noted that the correlation between these 2 variables is a mutual one. Javadi et al. (26) argued that increased hardships and distress caused individuals to lose sight of taking care of themselves and avoid self-care behaviors related to diabetes. However, we believe that the presence of distress and stressors obliges the patient to do more self-care activities. Therefore, the different results regarding the effect of these 2 variables on each other can have such a justification. Given that distress is one of the most important and effective factors in improving patients’ self-care behaviors, it is necessary to consider it when designing educational and counseling programs aimed at enhancing patients’ self-care behaviors and preventing complications of diabetes.
5.1. Conclusions
According to the results of this study, all variables of quality of life, diabetes distress, and self-care activities were correlated. As diabetes distress increases in these patients, the overall quality of life of patients will decrease. Diabetes distress is the most important factor in the quality of life of diabetic patients, so it should be given special attention. Finally, it should be noted that in health education and health promotion, considerable emphasis is placed on improving the quality and standards of life by increasing people’s participation in health-related self-care activities directly and indirectly. This could be achieved by adopting effective health strategies for choosing the right and accessible lifestyle, which will result in reduced diabetes distress and enhanced quality of life in these patients.