1. Background
Irritable bowel syndrome (IBS) is the most common disorder diagnosed by gastroenterologists. It can result in significant disabilities and costs (1), with a prevalence rate of 6% in Iran (2). This disorder can increase healthcare expenditures directly and indirectly. It is a type of functional gastrointestinal (GI) disorder characterized by chronic abdominal pain (CAP), nausea, vomiting, diarrhea, and constipation in the absence of any somatic and physiologic cause (3). The IBS pathogenesis is mainly unknown, with genetic and environmental factors influencing its prevalence. So far, no specific physiological or psychological disorders have been linked with IBS (4).
Social and psychological factors may play a role in the relationship between the central nervous system and the enteric nervous system, whose effects have been reported on the response to treatment and outcomes (5). In addition, the relationship between digestive disorders and psychological disorders indicates a specific gut-brain connection (6). Common IBS risk factors include gastroenteritis, depression, unfortunate life events, hypochondriasis, young age, estrogen therapy in the postmenopausal period, recent antibiotic therapy, food intolerance, and extraintestinal somatic symptoms (7). Although psychological symptoms are not part of IBS, they play an essential role in its clinical course and outcomes (8).
Some studies suggest that the IBS symptoms increase with aggravating psychological factors such as anxiety, mood disorders, depression, and stress caused by nerve stimulation (9, 10). Evidence suggests a higher prevalence of mood disorders and anxiety in IBS patients (11). Cognitive information and external stressors can affect the enteric nervous system, mobility, and secretion through neuron connections (12). Although no psychological symptoms are reported in most IBS patients, some researchers believe that about half of IBS patients are depressed, anxious, and hypochondriac; however, no precise psychiatric diagnosis prevails (13, 14). Patients with IBS who seek help for their symptoms suffer from emotional problems such as anxiety, depression, and personality traits of neurotics (15). Therefore, emotional symptoms or emotion regulation are regarded as the integrated and specific symptoms of IBS (16, 17). Welgan et al. (18) suggest that anger may significantly affect antral motor activity in IBS patients.
Numerous studies have dealt with the effectiveness of psychological therapies for improving IBS. Some effective therapies include cognitive-behavioral therapy (CBT), hypnotherapy, short-term psychodynamic therapy, relaxation, and stress management (13, 19, 20). Cognitive-behavioral stress management (CBSM) training is a practical psychological approach for improving IBS. The CBSM training is a multi-faceted approach through which relaxation, imagery, and other anxiety reduction techniques are combined with common cognitive-behavioral approaches such as cognitive reconstruction, coping effectiveness training, emotional expressiveness training, and anger management. Stress management techniques are successfully used for various emotional and physical problems such as anxiety, depression, insomnia, and diabetes (21-24).
Psychotherapy in medical conditions can reduce costly medical services and improve patients' mental health; therefore, psychotherapy-based interventions are essential in medical conditions and chronic diseases. Psychotherapy can alleviate current stressors of IBS or discover and heal previous essential life events.
2. Objectives
Therefore, the present study aimed to investigate the effectiveness of CBSM for depression, anxiety, cognitive emotion regulation (CER), and quality of life (QoL) in IBS patients.
3. Methods
3.1. Design and Participants
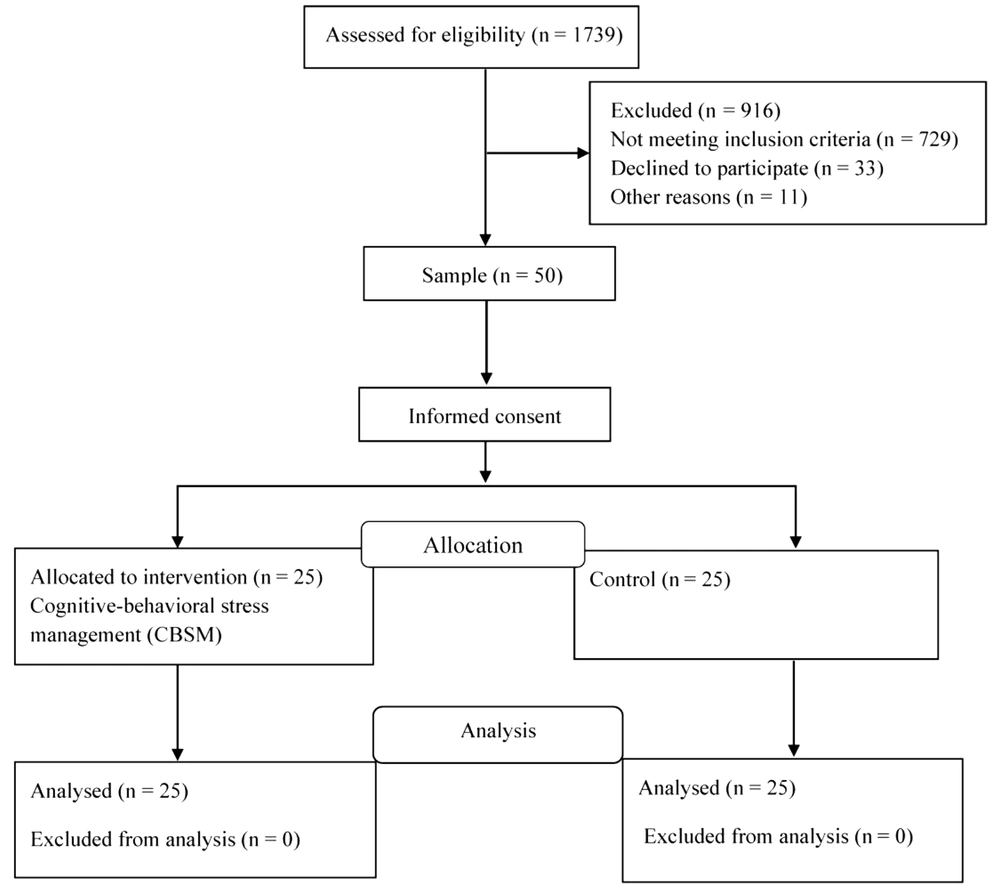
This semi-experimental study utilized a pretest-posttest design with a control group. The statistical population comprised all IBS patients visiting Be'sat Gastroenterology Specialist Clinic of Tehran in 2019. A sample of 50 patients was selected and randomly divided into intervention (CBSM, n = 25) and control (n = 25) groups (Figure 1). We included 25 IBS patients in each group using G-power software with an effect size of 2.45, α = 0.05, and a test power of 0.95. Inclusion criteria for IBS patients were an age of 20 to 55, taking no psychiatric medication in the past month before starting treatment, tendency to participate in the study after receiving explanations about the time, place, and type of therapy sessions, and filling the screening scales including the Beck Depression Inventory-II (BDI-II) and obtaining a score between 14 and 28. To observe ethical considerations and the rights of participants, first, both groups were separately justified that this is academic research and they can participate if they wish; therefore, they completed a written informed consent. In addition, they were assured that their information would be kept confidential.
3.2. Assessment Instrument
Cognitive Emotion Regulation Questionnaire (CERQ): The Emotion Regulation Questionnaire (ERQ) was developed by Garnefski and Kraaij in 2007 (25). The CERQ is a 36-item inventory rated on a 5-point scale from 1 (never) to 5 (always). This questionnaire measures nine cognitive strategies of self-blame, acceptance, rumination, positive reappraisal, refocus on planning, positive refocusing, putting into perspective, catastrophizing, and other-blame (20). Garnefski and Kraaij (25) reported Cronbach's alpha between 0.71 and 0.81 for ERQ subscales. In the present study, Cronbach's alpha coefficient was 0.83 for the questionnaire.
3.2.1. State-trait Anxiety Inventory
The State-trait Anxiety Inventory (STAI) was developed in 1988 to measure anxiety. It is a 40-item self-report measure of trait anxiety and state anxiety. The state subscale contains 20 items, and participants are asked to report their feeling when completing the inventory. The severity of mental anxiety is measured on a 4-point Likert scale (1 = very low, 2 = low, 3 = high, and 4 = very high). The trait anxiety scale also contains 20 items through which the participants report their general feelings of anxiety. The frequency of experienced anxiety is measured on a 4-point scale (1 = never, 2 = sometimes, 3 = often, and 4 = always) (26). Gustafson et al. (26) reported the reliability of this questionnaire as 0.93 based on Cronbach’s alpha coefficient. In the present study, Cronbach's alpha coefficient was 0.88 for the questionnaire.
3.2.2. SF-36 Questionnaire
The SF-36 Questionnaire (SF-36) was designed to measure physical and mental health status. It is a 36-item inventory to assess individuals' health in eight domains: Health status, physical function, role limitations due to physical health problems, role limitations due to emotional problems, somatic pain, social functions, vitality or fatigue, and mental health (27). Fallahzade et al. (28) reported Cronbach's alpha of 0.86 for the questionnaire. In this study, Cronbach's alpha coefficient was 0.89 for the questionnaire.
3.2.3. Beck Depression Inventory
The Beck Depression Inventory (BDI-II) is used to measure the severity of current depressive symptoms. In this 21-item scale, the participants are asked to rate the severity of their symptoms on a Likert scale (29). Garcia-Batista et al. (30) reported Cronbach's alpha of 0.89 for the questionnaire. In this study, Cronbach's alpha coefficient was 0.85.
3.3. Intervention
The intervention group received eight 90-minute, weekly sessions of CBSM training based on the treatment protocol developed by Lopez et al. (31). The intervention sessions were conducted by the first author, who had received specialized courses and workshops. No treatment intervention was offered to the control group; they were placed on the waiting list. At the end of the study, to observe ethical considerations, the control group received a course of CBSM. A summary of sessions is presented in Table 1.
| Sessions | Content |
|---|---|
| First | Getting to know the participants, introducing the therapist, acquaintance of participants with the group and explaining therapeutic objectives, familiarity with the rules and agreeing upon the time, number, and duration of sessions, conducting pretest. Introducing the training program, introducing the first component of stress and the first gradual muscle relaxation technique for 16 muscles. |
| Second | Explaining impacts of stress, practicing to raise awareness on somatic symptoms of stress and practicing gradual muscle relaxation, making participants aware of their specific responses and patterns of anger and anger management training, introducing meditation, and exercising mantras for meditation. |
| Third | Teaching effective communication, barriers, steps of expressive behavior, and how to deal with conflicts using problem-solving skills. |
| Fourth | Explaining the relationship between thoughts and emotions, emotions and bodily sensations, and how to change one's assessments in stressful situations to stop negative thoughts. |
| Fifth | Identifying negative thoughts, determining the type of distortion, and how to combine imagery with diaphragmatic breathing and gradual muscle relaxation. |
| Sixth | Teaching the difference between rational and irrational self-talk, recognizing each of them, and teaching five steps to replace logical thoughts. |
| Seventh | Introducing effective and inefficient coping strategies, getting to know the best coping style for different stressors, and identifying the coping style of each participant. Using cognitive review and mental rotation technique with reprocessing to control recurrent mental sparks and changing the meaning of traumatic events. |
| Eighth | Evaluating participants' social support network, identifying obstacles to creating and maintaining social support network, summarizing and concluding the sessions, and conducting the posttest. |
3.4. Data Analysis
Quantitative data were analyzed using the mean and standard deviation. Multivariate analysis of covariance (MANCOVA) was used to examine the effect of CBSM on studied variables. Levene's test was used to check the assumptions of MANCOVA. Data were analyzed in SPSS 23.
4. Results
The participants included 50 male and female patients with IBS, aged 36.39 ± 7.45 years. Demographic variables of IBS patients are presented in Table 2.
| Variables | CBSM | Control |
|---|---|---|
| Age (y) | 37.19 ± 6.31 | 38.95 ± 7.43 |
| Duration of illness (y) | 3.67 ± 1.58 | 4.09 ± 1.81 |
| Education | ||
| High school | 16 (64.00) | 15 (60.00) |
| College education | 9 (36.00) | 10 (40.00) |
| Marital status | ||
| Married | 17 (68.00) | 16 (64.00) |
| Single | 8 (32.00) | 9 (36.00) |
a Variables are expressed as mean ± SD or No. (%).
Table 3 presents descriptive data (mean and standard deviation) of depression, anxiety, CER, and QoL. The mean scores of depression, anxiety, negative and positive cognitive strategies, and QoL of the intervention and control groups were similar in the pretest. However, the mean scores of depression, anxiety, and negative cognitive strategies were lower in the intervention group than in the control group in the posttest. In addition, the mean scores of positive cognitive strategies and QoL were higher in the CBSM group than in the control group.
| Variables | CBSM | Control | P (Between Groups) |
|---|---|---|---|
| Depression | |||
| Pretest | 30.36 ± 2.49 | 29.80 ± 2.62 | 0.211 |
| Posttest | 24.70 ± 2.34 | 29.73 ± 2.76 | 0.001 |
| P-value (within groups) | 0.001 | 0.318 | - |
| Anxiety | |||
| Pretest | 28.80 ± 3.02 | 30.11 ± 3.39 | 0.158 |
| Posttest | 23.80 ± 2.88 | 29.43 ± 2.77 | 0.001 |
| P-value (within groups) | 0.001 | 0.124 | - |
| Positive cognitive strategies | |||
| Pretest | 41.40 ± 3.75 | 42.26 ± 3.34 | 0.191 |
| Posttest | 46.01 ± 4.10 | 41.77 ± 3.73 | 0.001 |
| P-value (within groups) | 0.001 | 0.218 | - |
| Negative cognitive strategies | |||
| Pretest | 38.93 ± 5.86 | 39.67 ± 6.52 | 0.208 |
| Posttest | 35.48 ± 5.63 | 40.12 ± 4.63 | 0.001 |
| P-value (within groups) | 0.001 | 0.108 | - |
| QoL | |||
| Pretest | 90.94 ± 8.50 | 91.41 ± 8.43 | 0.179 |
| Posttest | 105.93 ± 7.85 | 92.03 ± 8.39 | 0.001 |
| P-value (within groups) | 0.001 | 0.196 | - |
The homogeneity analysis of variance showed that the significance of Levene's test in the scores of anxiety, depression, CER, and QoL was greater than 0.05. Therefore, the homogeneity of variance (HOV) assumption in the studied groups was met. The homogeneity of the regression slope also supported the insignificance of the interaction between conditions and the pretest. There was a significant difference between the intervention and control groups in the variables in the posttest after controlling for the pretest scores.
Table 4 presents the univariate analysis of covariance results for the variables under study. Examining the differences between the intervention and control groups showed that by eliminating the effect of pretest, there was a significant difference between the two groups in depression (F = 31.15, P < 0.001), anxiety (F = 25.11, P < 0.001), positive cognitive strategies (F = 9.54, P = 0.021), negative cognitive strategies (F = 14.19, P < 0.001), and QoL (F = 15.48, P < 0.001). Therefore, the CBSM effectively reduced negative mood (depression and anxiety) and CER and improved QoL in IBS patients.
| Variables | SS | df | MS | F | P | η2 |
|---|---|---|---|---|---|---|
| Depression | 258.13 | 1 | 258.13 | 31.15 | 0.001 | 0.42 |
| Anxiety | 282.84 | 1 | 282.84 | 25.11 | 0.001 | 0.36 |
| Positive cognitive strategies | 97.06 | 1 | 97.06 | 9.54 | 0.021 | 0.27 |
| Negative cognitive strategies | 3139.45 | 1 | 3139.45 | 14.19 | 0.001 | 0.33 |
| QoL | 489.17 | 1 | 489.17 | 15.48 | 0.001 | 0.40 |
5. Discussion
The present study aimed to investigate the effectiveness of CBSM for depression, anxiety, CER, and QoL in IBS patients in Tehran. The results showed that the CBSM effectively reduced negative moods (depression and anxiety) in IBS patients. This finding is consistent with Kennedy et al. (32) and Gros et al. (33). To adjust to their conditions, patients experience changes in daily activities, somatic reactions such as sleep disturbance, and thinking or emotions. Of course, reactions such as decreased activity may have long-term consequences (34). When a patient experiences pain, bloating, constipation, or diarrhea, how they think about their symptoms can affect how anxious they become. Negative thoughts about illness may increase patients' anxiety and cause more severe symptoms manifested in behavior such as increased physician visits (32).
Behaviors such as changing diet, focusing on symptoms, avoiding social situations to control and reduce symptoms, or avoiding the consequences of illness that may result from patients' shame and embarrassment put patients in a vicious circle of fear and avoidance. Physiological, cognitive, and behavioral responses are interdependent and contribute to disease persistence. Therefore, changing cognition and behavior or both can potentially improve patients, and cognitive reconstruction techniques can also be helpful. The CBT helps reduce the severity of symptoms in IBS patients by altering dysfunctional beliefs and cognitive errors, reducing depression and anxiety, and improving their mental state (32).
The CBT applies various techniques such as anxiety management training, muscle relaxation training, negative thoughts control, destructive automatic thoughts recognition, and replacing more rational thoughts to neutralize the triggers of anxiety and its persistence. The rationale for using cognitive-behavioral therapies lies in the same thinking. In CBT, self-control training and the therapist's guidance make participants discover how their thoughts cause and maintain anxiety (35). This program considers patients' thinking processes in stressful situations and aims to change wrong and irrational assessments to replace them with rational and objective assessments. On the other hand, patients learn appropriate coping strategies for various problems. The second part of the program contains relaxation techniques that can eliminate physiological symptoms of stress. Therefore, this comprehensive therapeutic plan intervenes in stress's cognitive and physiological aspects and reduces anxiety and depression in patients (36).
The results also suggested that the CBSM was effective in IBS patients' CER. This finding is consistent with Kleinstauber et al. (37). In this training approach, IBS patients learned to promote their cognitions, feelings, and reactions to their emotional state and relationship with society and increase their tolerance and flexibility in facing challenges by realistically and positively evaluating their circumstances. The CBT changes the content of negative thoughts about oneself by identifying cognitive errors, challenging them, and behavioral tests. Therefore, it balances negative emotions about self, and by discovering and correcting negative and irrational thoughts of these people through organizing dysfunctional thoughts, it reduces ineffective beliefs such as the need for the approval of others, high self-expectations, self-blame, emotional problems, and worries associated with anxiety and helplessness toward change. In general, cognitive therapy entails a set of strategies such as confrontation, practical relaxation, skills training, and cognitive reconstruction training that affect pessimistic thoughts and negative emotions and help patients understand their thoughts and behaviors and emotions affecting their behavior (37).
The results suggested that CBSM increases IBS patients' quality of life. This finding is consistent with the results of Kinsinger (21). The QoL is a psychological variable that varies from person to person. In this study, numerous techniques were used to directly make small but effective changes in people's perception of life. For instance, imagery training was presented to improve the mood of IBS patients. They learned to use the gradual contraction and relaxation when they are in a stressful situation during the day in their leisure time and use this technique several times during the day, depending on their condition. Most IBS patients were optimistic about these techniques and provided positive feedback. Thus, they understood the difference between being stressed and relaxed and experienced its benefits; therefore, they were encouraged to repeat the training. This study sought to strengthen the coping styles of individuals as internally reinforced resources and improve the patients' QoL by teaching them different ways of challenging negative spontaneous thoughts. In addition, CBT provides practical solutions in daily life, increasing the use of appropriate coping strategies, improving communication with family and friends, successfully solving life challenges, and increasing life satisfaction, which ultimately increases the QoL (38).
This study faced some limitations. Since the present study was performed on IBS patients visiting Be'sat Gastroenterology Specialist Clinic of Tehran, caution should be observed in generalizing the results to other communities at different times and places due to different cultural conditions. Due to the difficulty of access to participants, it was not possible to conduct a follow-up stage to monitor the stability of the results.
5.1. Conclusions
According to the present study, the CBSM effectively reduced depression and anxiety and improved QoL and CER in IBS patients. Counseling centers are recommended to apply CBSM and consider its effectiveness in reducing depression and anxiety in IBS patients. Therapists are also recommended to apply CBSM in workshops to improve QoL and CER in IBS patients.