1. Background
Family members play an important role during the recovery process (1). Family is a complete and coherent system in which any threat to one member means a threat to the whole family. The presence of the family improves the client's self-care and confronting the problems caused by the disease. The family plays a vital role in caring for the patient because supporting the patient accelerates the recovery process (2). One of the most critical aspects of visitation is its psychological effects both on the patient and the visitor (3).
It seems that a good visitation not only can enhance the psychological status of the patient but also strengthens cognitive processes, such as being important and valuable in his/her mind. In addition, good visitation can accelerate and facilitate the process of overcoming the disease through positive visualization and imagery (4). Patient visitation can significantly affect mental and physical status (5). The results of many studies conducted on cardiovascular patients showed the positive effects of talking, looking, smiling, and touching the patient on waking, stimulating the nervous system, reducing heart rate, lowering diastolic blood pressure, and reducing anxiety in the patient (6). However, at present, almost all educational and private hospitals in Iran impose visitation restrictions in special wards (7-9).
Nurses are concerned that the patient's exposure to the family may lead to hemodynamic disorders (10). However, Partovi et al. showed that patients with no visitation restrictions had a better heart rate and more relaxation than those with visitation restrictions (11). Currently, the family visitation policy of patients admitted to the intensive care units has many restrictions (12), whereas family and family life are essential parts of every individual’s health. Concerning its importance and role for the patient, the family should be considered of vital importance in the nursing intervention programs as the patient him/herself. Today, the care environment includes patients and families, and public care involves family and patient care (13-15). For some reason, this continuity in family involvement is not always possible, and the family moves away from the patient. One reason is hospitalization in the intensive care unit, in which the presence of family members is prohibited, and visitations are severely restricted due to the philosophy and structure of such wards, leading to the dissatisfaction of patients and their companions (16, 17). Also, the informational needs of patients differ from one to another. The presence of the family in special wards and the information given to family members can be helpful for patients (18).
However, factors such as time constraints, lack of communication skills training, unclear goals, unknown and ambiguous processes, and other challenges affect family motivation and complicate this communication. Current communications in specialized departments are often inconsistent, inadequate, and of low quality (19). Family members believe that it can be beneficial and effective if they receive understandable and clear information every day. However, it is rare for families to receive sufficient and effective information (20). As a result, the patient's unique values and priorities may not be considered, and costly treatments may make the hospitalization process longer and more difficult for many patients (21).
During the last decade, visitation patterns have faced many challenges regarding patient-centered and family-centered care and moving toward free visitation, as many publications show that it is helpful for the patient, family, and nurse. However, most physicians and nurses find visitation in the cardiac care units (CCUs) stressful and believe patient visitation results in increased heart pain, dysrhythmia, and worsened vital signs (eg, blood pressure and heart rate). Therefore, they argued that patient visitation is dangerous, resulting in imposed restrictions in critical care wards (22). Some studies have investigated this issue, which despite the contradiction of some results, mainly indicated that visitation in critical care wards with special conditions is safe. However, further studies are warranted to prove this finding, evaluate its effect on patients' satisfaction, and find appropriate frameworks for safe visitation.
2. Objectives
Therefore, this study was conducted to investigate the effect of visitation on vital signs and satisfaction of patients admitted to the CCU of Golestan hospital, in 2021.
3. Methods
3.1. Study Design
This randomized clinical trial study aimed to investigate the effect of visitation on vital signs and satisfaction of patients admitted to the CCU in Golestan Hospital, Ahvaz, in 2021. The study was done single blindly, and patients did not know the nature of their group during the study.
3.2. Recruitment and Eligibility
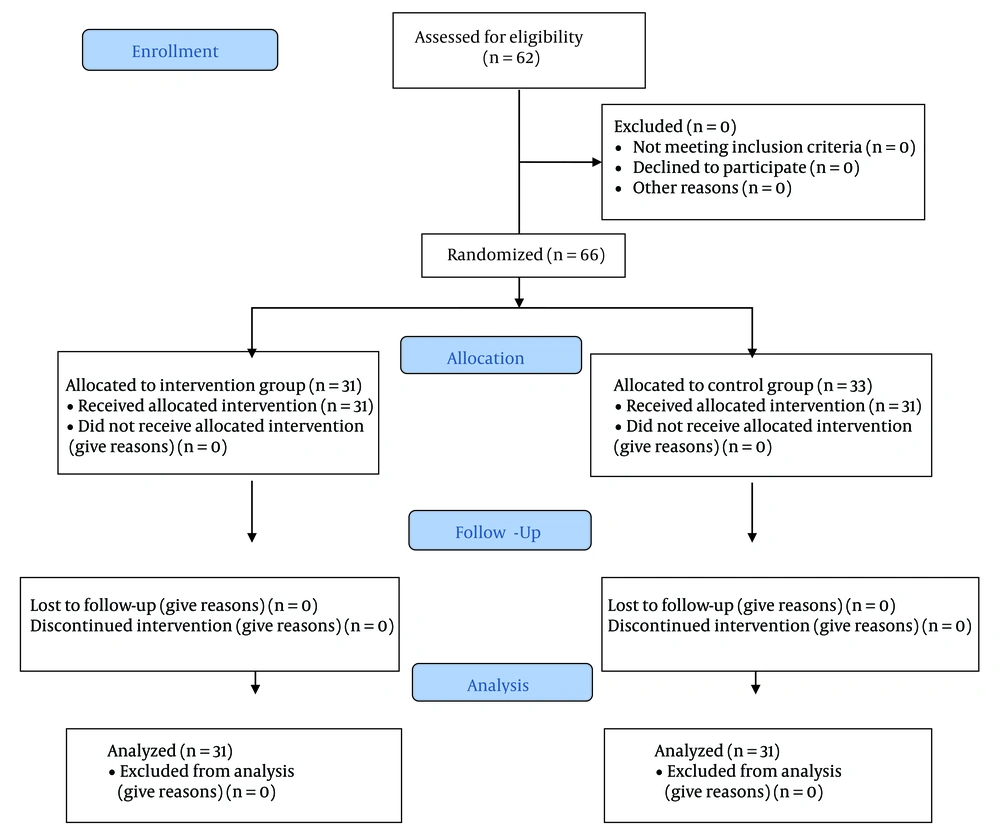
By considering the test power of 90%, α = 0.05, d = 1, s1 = s2 = ½, and 10% drop out, the sample size was determined as 62 subjects (31 in each group) using the following formula (Figure 1. The consort flowchart):
The inclusion criteria were:
(1) No visitation prohibition for the patient according to the attending physician’s opinion;
(2) Patient and companions’ consent to participate in the research;
(3) Visitors should be first-degree relatives of the patient and chosen by the patient;
(4) Age range of 18 to 60 years for the patient.
The exclusion criteria included:
(1) Severe change of vital signs during the study;
(2) Companions and patient’s dissatisfaction to continue the study;
(3) Patient’s death;
(4) Discharge from the ward before the third day of hospitalization.
3.3. Randomization
The research samples were patients admitted to the CCU wards of Golestan Hospital in Ahvaz. Participants were selected using simple random sampling based on inclusion and exclusion criteria using the random number table and were equally divided into control and intervention groups (31 subjects in each group). So that, following surveying patients against inclusion criteria, each of them received a number based on the order of inclusion in the study. The numbers were selected using a random number table. The researcher randomly placed his hand on a point in the table of random numbers, and then the numbers were selected in pairs from left to the right. Only numbers in the sample size range were selected. Even numbers were considered for the intervention group and odd numbers for the control group.
3.4. Intervention
Scheduled visitations were made twice a day, each time for 60 minutes, over three days in the evening shift between 4:00 and 5:00 pm and in the night shift between 8:00 and 9:00 pm for the intervention group. During visitation, an attempt was made to provide the necessary privacy for the patient and the visitor. The person selected from the family members to visit was fixed for three days at the patient's choice. Those in the control group received routine visitation. It should be noted that visitation in Golestan Hospital is currently permitted only on even days from 3 to 4 pm, at which time anyone can visit the patient.
3.5. Tools and Measurement
Data collection tools included a researcher-made checklist, the first part of which included patient's demographic and clinical information such as age, sex, marital status, level of education, history of hospitalization, underlying heart disease problems, frequency of hospitalizations, diagnosis of hospitalization, and the visitor. The second part of the checklist was related to systolic blood pressure, heart rate, respiration rate, and body temperature. These factors were measured and recorded for all subjects in three stages, including 5 minutes before the intervention, 30 minutes after the start of the visitation, and 30 minutes after the intervention, by the researcher using a Sazgan Gostar monitoring device.
The patient satisfaction questionnaire with the care extracted from Arefi and Talaei’s study (23) was used to assess patients’ satisfaction with the care. This questionnaire contains 11 items to assess patients’ satisfaction with the care and services provided in the hospital. The questionnaire is scored on a four-point Likert scale, including 1, 2, 3, and 4 points for “strongly dissatisfied”, “dissatisfied”, “satisfied”, and “strongly satisfied”, respectively. A score of 11 to 17 shows low satisfaction with the care and services provided by the hospital, a score of 17 to 28 indicates moderate satisfaction, and a score higher than 28 indicates high satisfaction. Minor changes were made in the questionnaire with the approval of 10 esteemed faculty members in the related field to consider the patient’s satisfaction with the visitation as well. The questionnaire was piloted on a sample of 10 patients, and Cronbach’s alpha was calculated at 90%. The items of the questionnaire were filled out by interviewing participants at the end of the third day.
3.6. Statistical Analysis
Data analysis was administered using SPSS version 22 (SPSS, Inc., Chicago, IL, USA). The chi‑square test (or Fisher's exact test) and t-test were used to test the homogeneity of groups for demographic and clinical data. Since the data obtained from the evaluation of the effect of visitation on some of the studied factors were measured three consecutive times, correlated and longitudinal responses were generated. As the generalized estimating equations (GEE) method is efficient in the analysis of correlated and longitudinal data, the effect of the intervention (visitation) was evaluated by this method and also by calculating the variance matrix of the model using the exchangeable method in a longitudinal study. Statistical significance was considered when the P-value < 0.05.
4. Results
The mean age of the participants was 61.82 ± 10.44. The independent t-test showed no significant difference between the study groups concerning the variable of age (P = 0.493). In this study, 34 males (54.8%) and 28 females (45.2%) were assessed, and the chi-square test showed no significant difference between the groups concerning gender (P = 0.399). In terms of hospitalization diagnosis, 31 people (50%) with a diagnosis of acute coronary syndrome (ACS), 13 (21%) with a diagnosis of myocardial infarction (MI), 9 (14.5%) with a diagnosis of decompensated heart failure (DHF), and 9 (14.5%) with a diagnosis of cardiac dysrhythmia were admitted to the CCU, and there was no significant difference between the two groups in this regard (P = 0.895) (Table 1). In the intervention group, in terms of the person who made the visitation, 8 (25.8%) were father, 9 (29%) were mother, 4 (12.9%) were brother, 4 (12.9%) were sister, and 6 (19.4%) were children of the patients.
| Variables | Group | Total | χ2 or t | P-Value | |
|---|---|---|---|---|---|
| Intervention | Control | ||||
| Age | 60.93 ± 10.335 | 62.74 ± 10.633 | 61.82 ± 10.444 | -0.690 | 0.493 |
| Diagnosis | 0.589 | 0.895 | |||
| ACS | 17 (27.41) | 14 (22.58) | 31 (50) | ||
| MI | 6 (9.69) | 7 (11.30) | 13 (21) | ||
| DHF | 4 (6.44) | 5 (8) | 9 (14.5) | ||
| Dysrhythmia | 4 (6.44) | 5 (8) | 9 (14.5) | ||
| Sex | 0.261 | 0.399 | |||
| Male | 18 (29) | 16 (25.8) | 34 (54.8) | ||
| Female | 13 (20.98) | 15 (24.21) | 28 (45.2) | ||
a Values are expressed as mean ± SD or No. (%).
In terms of patients' satisfaction with the care and services provided in the hospital, the results of the chi-square test showed a significant difference between the two groups (P < 0.000) so that the satisfaction level in the intervention group was higher than that of the control group (Table 2).
| Variables | Group | Total | χ2 | df | P-Value | |
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| Satisfaction Rate | 26.13 | 2 | 0.000 | |||
| Low satisfaction | 3 (4.83) | 20 (32.26) | 23 (37.1) | |||
| Moderate satisfaction | 8 (12.90) | 7 (11.29) | 15 (24.2) | |||
| High satisfaction | 21 (33.86) | 3 (4.83) | 24 (38.7) | |||
a Values are expressed as No. (%).
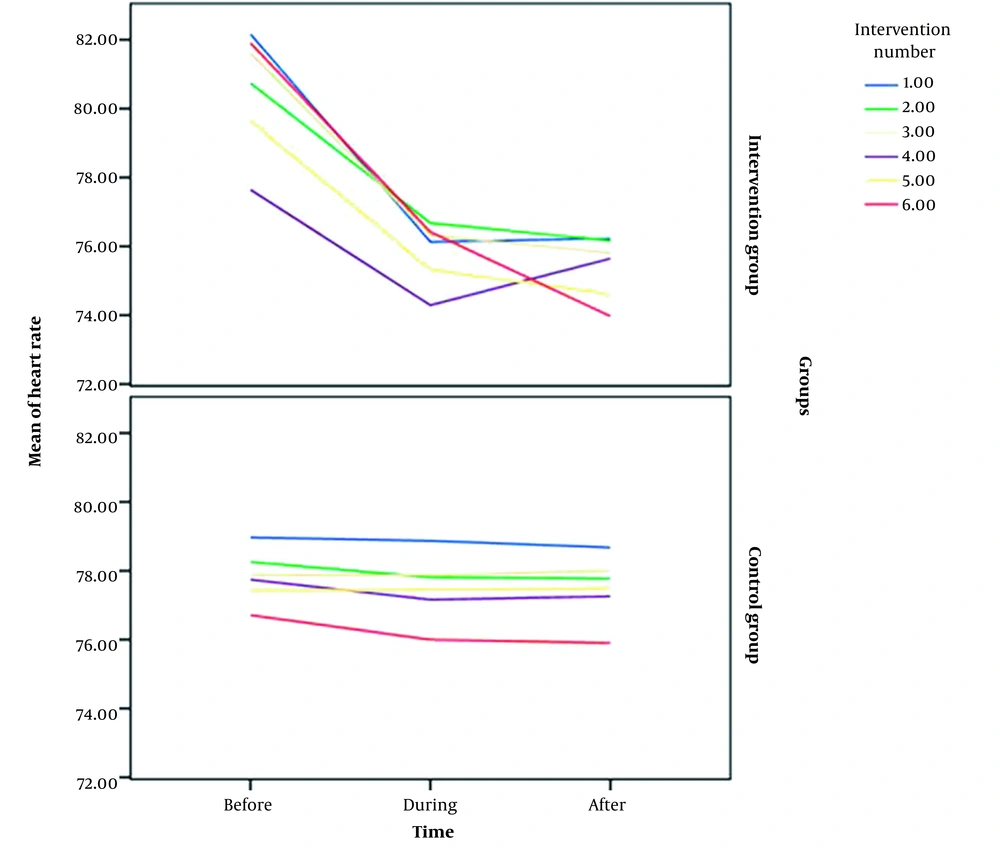
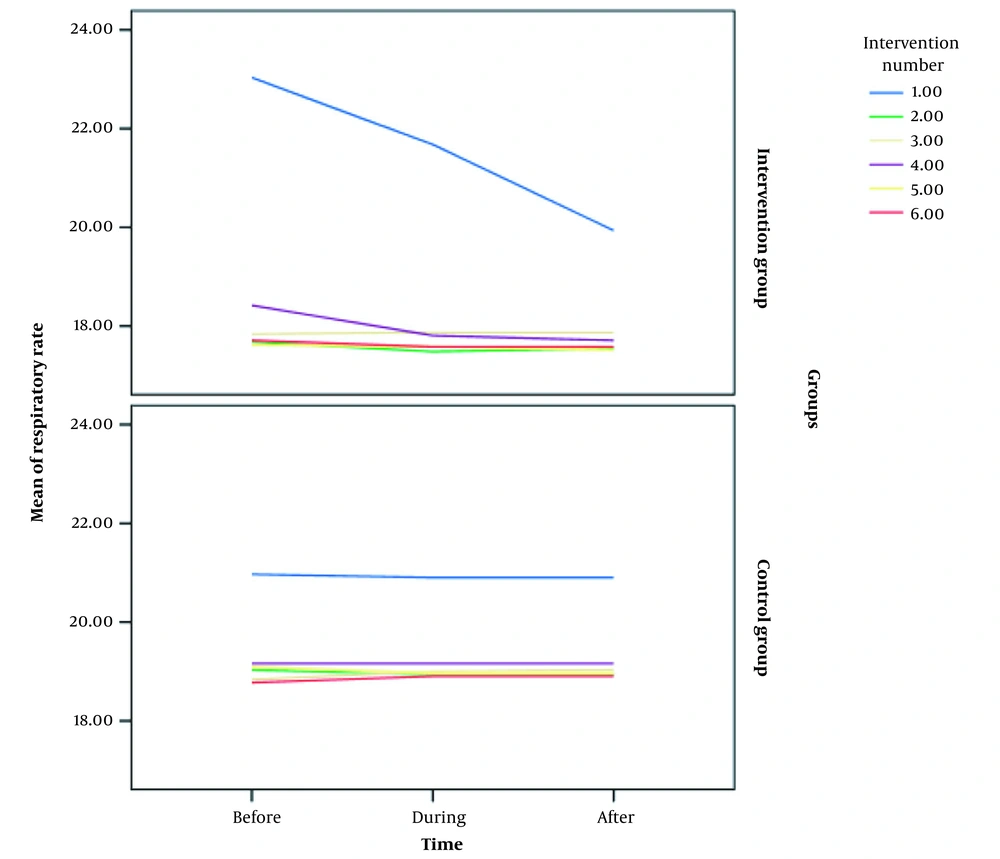
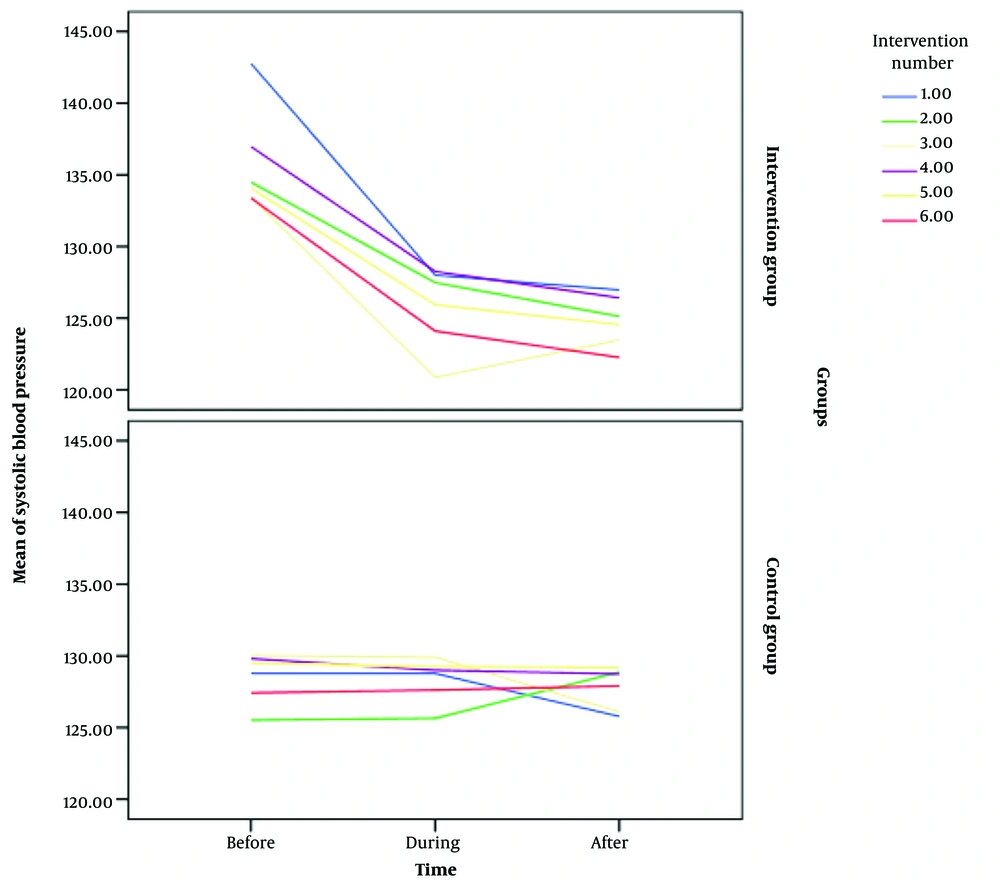
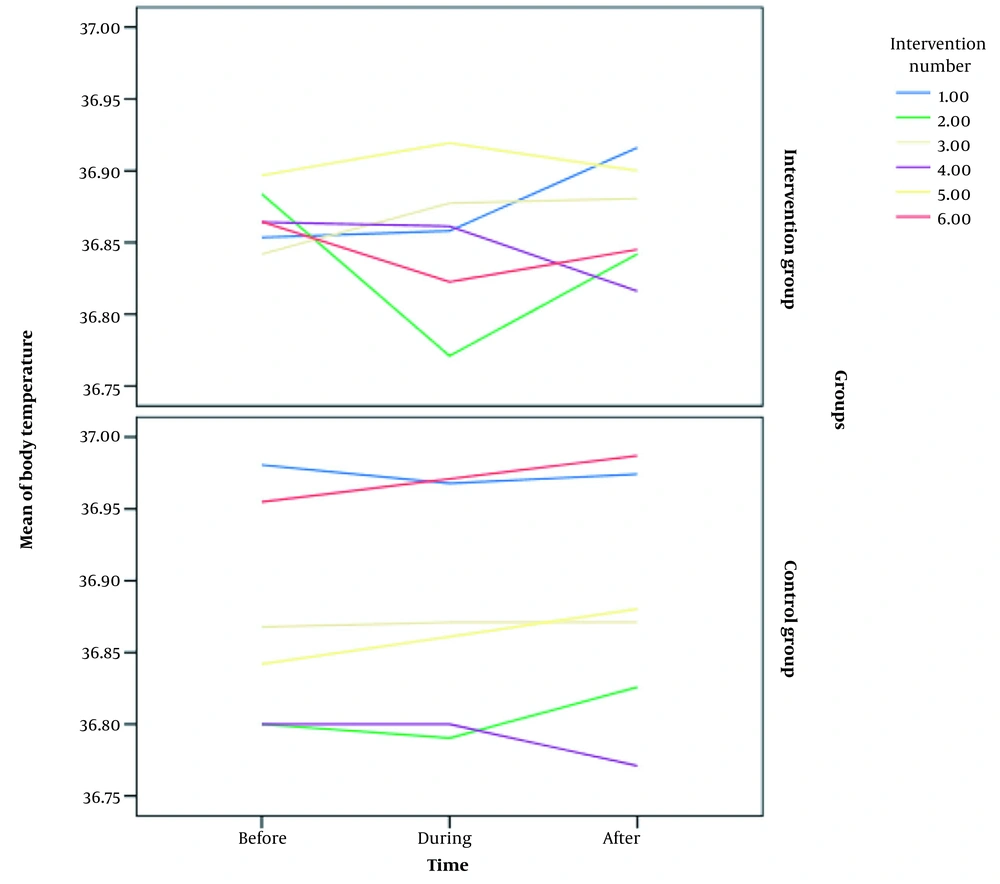
The independent t-test showed no significant difference between the mean heart rate of patients in the intervention group and control group before the intervention (P = 0.313), but during (P = 0.003) and after the intervention (P = 0.004), this difference was significant. Regarding systolic blood pressure, there was also no significant difference between the mean systolic blood pressure of patients before interventions (P = 0.126), but during (P = 0.005) and after the intervention (P < 0.000), this difference was significant. However, in terms of body temperature and respiration rate, no significant difference was observed between the two groups before, during, and after the intervention (Table 3). It should be noted that the values of the variables and their fluctuations both in the intervention group and in the control group were usually in the normal range.
| Variables | Group | t | df | P-Value | |
|---|---|---|---|---|---|
| Intervention | Control | ||||
| Heart rate | |||||
| Before intervention | 80.61 ± 11.91 | 80.63 ± 10.22 | 0.786 | 1 | 0.313 |
| During intervention | 75.86 ± 9.79 | 78.52 ± 10.17 | 16.34 | 2 | 0.003 |
| After intervention | 75.40 ± 10.13 | 75.40 ± 10.05 | 15.24 | 2 | 0.004 |
| Respiratory rate | |||||
| Before intervention | 18.71 ± 7.16 | 19.31 ± 4.94 | 0.742 | 1 | 0.351 |
| During intervention | 19.33 ± 6.49 | 19.34 ± 4.93 | 0.884 | 1 | 0.492 |
| After intervention | 19.02 ± 5.48 | 19.31 ± 4.95 | 0.691 | 1 | 0.394 |
| Systolic blood pressure | |||||
| Before intervention | 135.85 ± 11.49 | 134.50 ± 13.24 | 1.11 | 1 | 0.126 |
| During intervention | 125.77 ± 13.21 | 128.36 ± 11.41 | 12.34 | 2 | 0.005 |
| After intervention | 124.80 ± 9.2 | 127.86 ± 15.6 | 21.18 | 2 | 0.000 |
| Body temperature | |||||
| Before intervention | 36.8 ± 0.34 | 36.87 ± 0.23 | 1.245 | 1 | 0.126 |
| During intervention | 36.85 ± 0.31 | 36.87 ± 0.25 | 0.311 | 1 | 0.874 |
| After intervention | 36.86 ± 0.29 | 36.88 ± 0.23 | 0.416 | 2 | 0.795 |
a Values are expressed as mean ± SD.
The GEE showed a significant difference between patients' mean heart rate and systolic blood pressure in the intervention group during different times (P < 0.000); in other words, at different times (ie, before, during, and after visitation), their values were declined during and after visitation compared to before it. However, there was no statistically significant difference between the mean body temperature and respiration rate in the intervention and control groups at different times. More details are given in Table 4 and Figures 2 to 5.
| Effects | F | P-Value |
|---|---|---|
| Heart rate | ||
| Intercept | 4277.950 | 0.000 |
| Group (intervention *control) | 0.019 | 0.889 |
| Time | 83.445 | 0.000 |
| Group * time | 65.484 | 0.000 |
| Respiratory rate | ||
| Intercept | 3942.60 | 0.000 |
| Group (intervention*control) | 2.535 | 0.111 |
| Time | 4.428 | 0.109 |
| Group * time | 4.55 | 0.102 |
| Systolic blood pressure | ||
| Intercept | 16294.16 | 0.000 |
| Group (intervention*control) | 0.088 | 0.766 |
| Time | 73.258 | 0.000 |
| Group * time | 60.932 | 0.000 |
| Body temperature | ||
| Intercept | 6207360.90 | 0.000 |
| Group (intervention * control) | 0.319 | 0.572 |
| Time | 1.606 | 0.448 |
| Group * time | 0.588 | 0.754 |
5. Discussion
The results showed no significant difference between patients' mean heart rate and systolic blood pressure in the intervention and control groups before the intervention. Also, no significant difference was observed between the two groups regarding body temperature and respiration rate before, during, and after the intervention. In addition, there was a significant difference between the mean heart rate and systolic blood pressure of patients in the intervention group during different times; in other words, at different times (ie, before, during, and after visitation), their values were declined during and after visitation compared to before it. However, no significant difference was observed between the mean body temperature and respiration rate in the intervention and control groups at different times. Mahmoudi et al. showed that increasing the duration and frequency of visitations up to 30 minutes per day in three 10-minute intervals in the intervention group, compared to 10 minutes per day in the control group, could decrease systolic and diastolic blood pressure indices in patients admitted to the intensive care unit (24), which is consistent with the results of the present study. In this regard, Salavati et al. showed that the mean heart rate, systolic and diastolic blood pressure, mean arterial pressure, and respiratory rate in the intervention group 10 minutes before and during visitation, 10 minutes after the start of the visitation, and 10 minutes after the end of the visitation were not significantly different (1), which is not consistent with the results of the present study. Furthermore, Akbari et al. showed that increasing the duration and frequency of family visitations of the patient in the ICU resulted in reduced systolic blood pressure up to 30 minutes after the visitation. However, no effect was observed on systolic blood pressure after a long time, ie, 24 hours after the first visitation, 24 hours after the second visitation, and 48 hours after the second visitation (25). Rezaie et al. showed that increasing the visitation time to 30 minutes per day in the evening shift increased systolic blood pressure in patients in the intervention group up to one hour after the visitation, compared to visitations from behind a glass wall in the control group, which did not affect patients’ physiological indices (26). Rahmani et al. reported that the mean systolic blood pressure of patients in the intervention group significantly reduced on the third day of hospitalization compared to the first day of hospitalization, whereas the mean systolic blood pressure in the control group increased on the third day of hospitalization compared to the first day of hospitalization; this difference was not statistically significant (4).
The present study is different from previous studies in some ways. For instance, the duration of the companion's presence at the patient's bedside was less than twice a day, and studies performed in the CCU had fewer visitation restrictions than those performed in the ICU. Also, the results of the present study regarding patients' satisfaction with the care provided in the CCU and the services provided in the hospital showed a significant difference between the two groups; that is, those in the intervention group presented a higher level of satisfaction than controls. In this regard, Heidarzadeh et al. showed that the scheduled visitation was a good way to reduce anxiety in patients with angina pectoris admitted to the CCU, so it could replace the prohibited visitation method in ICUs (27). In a study on 53 subjects, Orlean compared the anxiety and satisfaction level of the spouses of patients admitted to the ICU in two methods of free visitation and four times a day. This study showed that the spouses of the patients belonging to the free visitation group had higher satisfaction than those in the restricted visitation group (28). Also, Najafvandzadeh et al. showed that an appropriate visitation policy should be adopted in the CCU to provide a treatment setting intended to reduce patients' unpleasant psychological and physiological reactions and to create an environment in which patients' anxiety and psychological stress are minimized so that patients' cardiovascular complications are also decreased, and their health and satisfaction levels are increased (29). Yari-Bajelani et al. showed that free visitation led to reduced anxiety, improved sleep quality, and increased patients' satisfaction after coronary artery bypass graft surgery (30).
5.1. Conclusions
It can be argued that a scheduled visitation for the presence of family and friends at the bedside of patients admitted to the intensive care unit not only does not lead to disturbing vital signs but also can cause positive clinical changes in vital signs and satisfaction level. Thus, based on the findings of this study, there is no reason for restricted visitations in patients admitted to the coronary care unit. Hence, by designing appropriate visitation policies, it is possible to pave the way for increasing patients' satisfaction and the efficiency of the treatment and care system.
5.2. Limitations
It is necessary to mention some limitations of our study, including resistance by ward staff against the daily presence of patients' families in the ward, especially during the early days. We tried to educate the families and increase the staff's awareness of the study's objectives to solve this problem. Fortunately, this problem was largely resolved over time.