1. Background
Thalassemia is a hereditary blood disease (1). This complex disease needs special therapeutic medications (2, 3). Approximately 1.5% of the world’s population is beta thalassemia carriers (4). Thalassemia is highly prevalent in the north and south of Iran and is an endemic disease (5, 6). Observing and monitoring the patient with thalassemia is essential (7).
Information management for families of genetic diseases is vital (8). Chronic disease diagnosis at any childhood stage has negative effects on spiritual, social, and mental performance (9). Chronic disease in infants has two consequences. In the first case, the consequences affect children and family members, such as reduced participation in school, decreased physical activity, and mental and psychological problems, and in the second case, the consequences affect the family system, including changes in roles and communications, as well as disruption of pre-existing routines (10).
Family is the main source of patient support. Families of children with thalassemia may become exhausted due to the frequent hospitalizations of the child for blood injections and because of spending a great deal of time learning about and managing this disease (11). Parents of children with thalassemia often tend to recite their stories. In fact, these stories reveal their feelings, challenges, and medical experiences (12). Researchers and clinicians are always seeking to study managerial problems and the weak performance of families of chronic children (13). One of the pivots of care is offering holistic care (14). The healthcare team has a unique position to offer support to families (15). Punaglom et al. stated that parents’ experience is based on their cultural and community context (16). Pouraboli et al. showed that parents of children with thalassemia have many problems in the healthcare system (17). Atiye Karakul et al. said the healthcare team should be aware of parent experience with children with thalassemia because parents’ experiences help them support, care for, and plan proper intervention (18). One study in Iran showed that parents of children with thalassemia have physical, mental, social, and economic problems (19).
Due to the fact that the family is the main source of support for patients, as well as the fact that a family with a child with thalassemia has to deal with many challenges and experiences, the experiences of the parents, are a source of guidance for healthcare professionals.
2. Objectives
The researcher decided to conduct a research project focusing on supportive systems for parents of thalassemia children.
3. Methods
3.1. Design
This study was done at Hajar Hospital in Shahrekord in 2017. Qualitative inductive was used. Content analysis was applied (19, 20).
3.2. Patient Selection
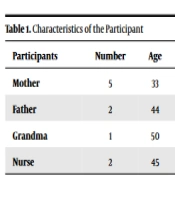
Participants in this study include ten samples of parents, grandmothers, and nurses (Table 1). Purposeful sampling was done for selecting samples. In this study, the selection of participants continued until data saturation was achieved. Saturation means that no additional data are obtained. The inclusion criteria for participants are parents with thalassemia and children with a definite diagnosis of thalassemia and an interest in participating in the study, parents who don’t have serious illnesses such as depression and chronic illness causing significant needs, and the parents themselves. Exclusion criteria included disinterest in cooperating at each stage of the project.
| Participants | Number | Age | Experience of Work |
|---|---|---|---|
| Mother | 5 | 33 | - |
| Father | 2 | 44 | - |
| Grandma | 1 | 50 | - |
| Nurse | 2 | 45 | 20 |
3.3. Data Collection
Deep, semi-structured, face-to-face and individual interviews were conducted for data collection. In semi-structured interviews, the questions are based on the interview process. A number of questions were used in the interview. “Please describe your experience of having a child with thalassemia and its impact on your life” Probing questions were used like: “Please explain more”, “Tell me more about it”, and “How did you feel about it?”, “What do you mean when you say (….)?”. 10 interviews were done. All interviews were recorded. The average interview lasted 30 minutes. The interview was done in the personnel room.
3.4. Data Analysis
We used qualitative content analysis (20). We did not use software for data analysis. All participant statements were entirely recorded by an MP3 recorder and were written word by word, and the content was analyzed and coded. At first, data analysis begins with repeatedly reading the text and finding an overview. Then, the texts are read word by word so as to achieve codes. This is a continuous process, from obtaining the codes to labeling them. After obtaining codes, important paragraphs and sentences are arranged based on similarities and differences, and then the subcategories are combined into a few main categories based on their relations (21).
In this research, the parents who were involved in the study were interviewed after obtaining a consent letter from them. Interview and data analysis were done simultaneously. All interviews were analyzed word-by-word. Words containing the key concepts were bolded, and the codes were achieved. After deriving concepts and codes from important sentences, they were classified into subcategories. Finally, the subcategories were merged based on their relationship and reduced to categories.
3.5. Trustworthiness
In order to achieve credibility, opinions from the research team were taken into account when conducting interviews and analyzing data. Team members discussed interview texts and extracted meaning units, themes, and subthemes. A member check has been conducted. For the purpose of determining the dependability of the data, the views of an external viewer familiar with qualitative research, who was not a member of the research team, were obtained. The results were agreed upon by 88% of the participants. A report regarding the progress of the research was prepared in order to ensure conformity. To determine data transferability, data collected from 2 parents outside of the study who had experiences similar to those of the participants were argued and confirmed.
3.6. Ethical Considerations
This study is the result of an approved plan with an ethics code from Shahrekord University of Medical Sciences (IR.SKUMS.REC.1394. 41). Throughout the present study, the confidentiality and anonymity of participants, as well as ethical considerations have been observed.
4. Results
Table 1 shows the characteristics of the participants. Based on data analysis, three categories of the need for supporters, lack of consultative services, and economic problems were obtained (Table 2).
| Main Category | Category | Subcategory |
|---|---|---|
| Lack of supportive systems for parents of child with thalassemia | Need for supporter | Relatives support |
| Need for healthcare team support | ||
| Lack of consultative services | Psychological disorders of all family members | |
| Need for consultation | ||
| Economic problems | Financial support | |
| Father’s employment |
4.1. Need for Supporter
This category was divided into two subcategories: The need for relatives’ support and the need for healthcare team support.
Most parents stated that due to the chronic nature of the disease, support from relatives is necessary. They also declared that the health system does not support them. Most parents stated that a child with thalassemia needs relatives and family support, but most of them were not supported by their relatives. In this regard, a mother said:
“Now the income is low, and the expenses are high, what can this child do? The parents have psychological problems. My husband comes home tired. I cannot argue and fight with him. Other mothers say they are the same way. It’s very difficult. Our life has been shattered. Taking care of a sick child is challenging...” (M4)
A father said:
“Having a child with thalassemia is very difficult. These families need to be supported. But there is no supportive organ in our system. We are alone with a lot of problems …” (F2)
Most parents stated that there was no support system for them. Since there are many children with thalassemia and they have specific problems, there should be supportive organizations. In this regard, a mother said:
“No one supports us. We need a lot of help. I don’t have money. I have been told to take my son to the doctor, but I can’t because I have no money. I can just take him for a blood injection…” (M5).
In this regard, another mother said:
“We hurt. We bring him home after blood injections so that he can experience health. If he was better, he wouldn’t require me. He needs a lot of help. I should ignore myself and help him…” (G1)
4.2. Lack of Consultative Services
The category includes two subcategories, including psychological disorders affecting all family members and the need for consultation.
Most parents stated that they experienced several psychological problems following the birth of a child with thalassemia, but there were no consultative services for them. In this regard, a mother said:
“Since the birth of my child, I have developed a nervous disorder. It is very difficult for parents. We are sad about the blood injection. We are bothered by all the stress. It is very difficult because they should be under supervision…” (M2)
Another mother said:
“My daughter has thalassemia. Her father, my children, and I suffer from neurasthenia. I have a 15-year-old daughter with whom we can’t talk at all. She shouts. Her sister has thalassemia, and now her sister’s child has been added. She can’t tolerate it. I am 45 years old. I have diabetes. I have high cholesterol. I have heart problems, and my thyroid gland is underactive. I take several tablets during the day. Her father is also the same.” (G1)
Another mother said:
“When I ask other mothers who have a child with thalassemia, they say that they are all the same. They suffer from depression. Their minds are obsessed with negative thoughts. We are worried that something will happen to our child. My daughter is now 25 years old; I have been worried about her future since she was a child. It is a terrible life as if we don’t enjoy this world.” (M3)
4.3. Economic Life
This category was specified with two subcategories of financial support and problems of the father’s employment.
Most parents stated that they did not have enough money to buy medicine. This situation was doubled for families whose fathers had thalassemia. In this regard, a mother said:
“Well, it has its own difficulties because they should be under supervision most of the time, but it is more difficult for the child. I myself have a financial problem too because I should buy their medicine …” (M2)
Another mother stated that:
“Since her father has thalassemia, it is difficult for him to work. He cannot do every job; first there is a financial problem, then …” (M5).
Another mother said:
“My husband does not have a good job, he works two months a year, and he is unemployed the rest of the months. He is self-employed, and if he works, if he finds a job…”
5. Discussion
Based on data analysis, three categories of the need for support, lack of consultative services, and economic problems were obtained. The results of the present research determined that parents of a child with thalassemia need the support of relatives and the healthcare team and the results of other studies confirmed this finding. Findings of research revealed that chronicity of thalassemia and threat to the life of the child during life cause them stress, and they become susceptible to mental disorders (22). As Sapountzi-Krepia et al. stated, parents who have a child with thalassemia do not receive sufficient support (11). Gharibeh et al. stated that nurses play an important role in supporting children with thalassemia in disease management and decreasing their psychological problems (23).
We found that in families who have a child with thalassemia, all members face mental disorders and require consultative services. Caocci et al.’s findings revealed that parents of patients with thalassemia need psychological support throughout their life (24). Cipolleta et al. suggest that a family-based approach should be utilized when dealing with chronically ill children (25). Healthcare teams should be familiar with the relation between disease progress and risk factors and palliative care in families of these children (25). Furthermore, Christian stated that the new knowledge in thalassemia care is guidance for pediatric nurses so that they may apply new strategies to establish a balance between the needs of children with chronic disease and teaching self-management/effective self-management to their parents (26).
The results of the present study revealed that most families, due to problems with the father’s employment, need financial support, which is in line with the results of other studies. In order to reduce parents’ stress, family-based plans, such as providing medical information, and mental and financial support, are essential (27). Heath et al. stated that the parents of a child inflicted with chronic disease are the key facilitators (28). Parents need to be supported by the healthcare team. These parents should be given care services training (28).
Although parents stated that the social support of nurses is good, it is necessary to promote cooperation in this regard (29). Social support is one of the key factors in decreasing parents’ stress and their physical health (30).
Parents’ frustration, social isolation, and lack of knowledge, as well as disruptions in family relations, must be recognized by the healthcare team, and they should offer consultative services to parents. The healthcare team has an important role in the life of these children. At first, they should listen to parents’ concerns well, and then they should help them in decision-making (31). Therefore, recognizing parents’ beliefs about problems is important for better understanding; it also increases their motivation to cooperate in social support (32). The healthcare system is faced with various challenges, and patients’ experiences are quality indices that have an effect on the economic improvement of healthcare organizations (33). Findings from our study can help to policy maker for planning and designing proper interventions.
5.1. Limitations
As a qualitative study, it cannot be applied to other communities or cultures.
5.2. Conclusions
The results of the present study revealed that the need for support, lack of consultative services, and economic problems are major problems for parents of children with thalassemia. Since thalassemia is a chronic disease, the parents of these children need support and consultative services throughout their life. The present study is a qualitative study, but it cannot be generalized to all societies. The present study revealed that the parents of children with thalassemia need the support of the healthcare system. This depends on the point of view and decisions of health planners who are responsible for the health of society.
5.3. Suggestions
It is necessary for authorities and healthcare planners to take measures in order to support parents of children with thalassemia (the forgotten part of the health system). The consultant-trained nurse has an important role in supporting these families.