1. Background
Sickle cell disease (SCD) is a neglected chronic disease of increasing global health importance. This disease is a hemoglobinopathy defined as HbS. In this disease, red blood cells lose their oxygen-carrying capacity, which is normally presented through painful crises following vascular occlusion (1, 2). The SCD symptoms include vasoocclusive crisis episodes, chronic anemia, fatigue, increased risk of infection, severe damage to body organs, and serious complications in life (3). This disease has affected millions of people around the world (4). In most countries, nearly 10 - 40% of individuals have the sickle cell gene. Overall, the prevalence of the disease has been estimated to be 2% around the globe (5). Besides, the number of SCD infants has been predicted to increase from 305,800 in 2010 to 404,200 by 2050 (6). In Iran, the prevalence of SCD has been reported to be higher in southern provinces, particularly Khuzestan province. According to the latest statistics, almost 500 patients with SCD exist in Khuzestan province (7), where the disease has been detected sporadically among indigenous Arab people (8).
The SCD is a major general health problem (9), which results in higher mortality among pregnant women, adolescents, and children below five years old (5). Patients with SCD tolerate great mental and social burdens, which exert significant effects on their physical, social, mental, and occupational well-being and independence (10). Assessments have revealed that the mean treatment cost was 1389 dollars per month for each patient with SCD, a great portion of which (80.5%) was related to hospitalization (11). Therapeutic measures for these patients include screening infants for prevention and timely treatment, utilization of prophylactic antibiotics against infections, anti-malaria medications, specific vaccinations, various supplements such as folic acid, and disease management alongside continuous follow-up (12, 13). In the disease management process, patients are encouraged to take responsibility for the treatment and control of their disease (14). This approach has been supported as a means of improving the effectiveness of treatment (15). Disease management aims to identify patients or individuals prone to the disease in the society, application of programs for preventing the emergence or progress of the disease, and improvement of self-care and, consequently, the society’s health (16, 17). Evidence has indicated that self-care promotes health outcomes in patients with chronic diseases and SCD (7, 18, 19). In fact, 90% of patients can manage their most important symptoms, i.e., pain at home (20). However, success in self-management of the disease depends on the accurate application of information technology because information plays a pivotal role in individuals’ attempts for self-care. Sufficient information literacy is an essential element for enabling individuals to change their behaviors, improve their lifestyle and quality of life, and promote their health (21). Houwing et al. showed that 78.6% of caregivers had low health literacy according to the SAHL-D (Short Assessment of Health Literacy in Dutch) (22). Caregivers with lower HL were more likely to have lower education and to have been born outside the Netherlands. Only four caregivers (9.5%) reported having difficulties in understanding and applying health information (measured by SBSQ). Mean scores on the Set of Brief Screening Questions (SBSQ) and Perceived Self-Efficacy in Caregiver-Patient Interactions (PECPI) were high, indicating that caregivers perceived their abilities for self-efficacy and their ability to read and understand medical information as quite high (22). Moreover, Perry Caldwell and Killingsworth highlighted there are significant differences in health literacy scores and influencing factors in adolescents with and without SCD (23).
Considering the importance of health literacy, World Health Organization (WHO) has announced it as one of the determinants of health and criteria for enhanced quality of life in the 21st century (24). From WHO’s perspective, quality of life is a broad concept composed of an individual’s perception of one’s physical status, mental status, independence level, social relations, interactions with the environment, beliefs, and personal values (25). Health-related quality of life is a subset of total quality of life, which includes the feeling of mental, emotional, social, and physical well-being and reflects the patients’ subjective evaluation and response to treatment (26). Vilela et al. showed the patients exhibited overall impairment of quality of life, which was more pronounced among adults and under 15-year-old adolescents. Married adults exhibited less impairment of most quality of life domains compared to unmarried adults, and the adults with mood disorders exhibited greater impairment of all quality of life domains (27). In another study, Kambasu et al. highlighted that pain was negatively associated with both physical and psychosocial functioning, whereas getting the Pneumococcal vaccine was positively associated with both physical and psychosocial functioning as reported by children and caretakers (28). This shows that the quality of life of patients with SCD is always an important variable that should be considered in different societies.
Nurses can affect the patients’ quality of life by executing nursing measures. Hence, awareness about the patients’ quality of life can help perform appropriate planning and systematic cares based on each patient’s conditions (29). Generally, assessment of quality of life is done with the purpose of taking proper measures for performance of nursing care, improvement of patients’ knowledge and self-care skills, and promotion of their quality of life (30). To the best of our knowledge, limited studies have been conducted on the relationship between quality of life and information resources associated with disease management amongst patients with SCD. Additionally, patients with lower health literacy have lower control over their disease, which results in more severe disease complications. Therefore, the relationship of information resources associated with disease management with quality of life is of particular importance.
2. Objectives
The present study aimed to determine health literacy (information resources) and their relationship with the dimensions of quality of life among patients with SCD.
3. Methods
3.1. Study Design
The present descriptive-correlational study was conducted in Baghaei-2 Hospital, Ahvaz, in 2020. The research population included all patients with SCD in Iran. The study was conducted on confirmed male and female cases of SCD in Iran.
3.2. Participant
Using Cochran’s formula [n = [(Z1 – α/2 + Z1 – β)2 δ2]/(µ - µ0)2] and considering the error rate of 0.08, β = 0.2, α = 0.05, Z1-∝/2 = 1.96, Z1- β = 0.84, δ = 21, μ = 50, μ0 = 45 and a 150 subject sample size was estimated for the study based on Ahmadi study (11). The participants were selected via accessible sampling. The inclusion criteria of the study were age above 18 years and confirmation of SCD by a specialist. The exclusion criteria of the study were incompleteness of the study questionnaires and incidence of an SCD crisis. These patients have been referred to the thalassemia clinic and the thalassemia ward of Shahid Baghaei-2 Hospital.
3.3. Study Instrument
The study data were collected using an instrument including two parts. The first part contained a researcher-made questionnaire on health literacy (information resources) developed by Salehi et al. in 2015 (31). The validity of the questionnaire was approved by two medical informatics specialists. Its reliability was also confirmed by r = 0.86 using the test-retest method. In this study, the reliability of the health literacy questionnaire was calculated to be 0.73 using the test-retest method. This part of the questionnaire consisted of three sections, the first of which included the patients' demographic information, such as age, sex, marital status, education level, duration of the disease, and living place. The second section included nine questions about the methods of knowledge acquisition about SCD and the impacts of such information on the disease process. Finally, the third section involved the reasons for not acquiring knowledge about the disease. When the patients had acquired knowledge about the disease, they were required to fill out the second part of the questionnaire. If not, they were requested to mention the reasons for not acquiring knowledge about the disease in the final section of the questionnaire. In this instrument, three questions were responded to via a five-point Likert scale, and the rest of the items could be answered by more than one option. The second part of the study questionnaire included WHOQOL-EREF-26 items, which consisted of 24 items in physical, mental, social, and environmental health dimensions. It should be noted that the first two items of the questionnaire did not belong to any of the dimensions and evaluated health status and quality of life as a whole. Thus, the questionnaires contained 26 items scored from 1 to 5. It should also be mentioned that three questions were scored reversely. Thus, each dimension could receive a score from 0 to 100, representing the worst and best conditions, respectively. The validity and reliability of the questionnaire were assessed by Monfared et al. in Iran. The results revealed α = 70% for all dimensions, except for the social dimension (α = 55%). Therefore, two questions (27 and 28) were added to the dimension of social relations to achieve appropriate reliability. Thus, this questionnaire has been standardized in Iran (32).
3.4. Data Analysis
All data analyses were performed using the statistical software SPSS, Version 22. P-values less than 0.05 were considered statistically significant. Continuous variables are reported as mean ± standard deviation (SD). Categorical data are expressed as number (percentage). The normality of continuous variables was examined using the Shapiro-Wilk's W-test. The univariate association between patient’s age, disease duration, and quality of life scores was assessed with Pearson's correlation coefficients test. Independent sample t-test was used to compare quality of life scores between two gender (male/female) and marital status (single/married). Quality of life scores between other characteristics was compared with ANOVA. Univariate linear regression models were conducted to examine the association between the explanatory variables and the outcomes of interest (score of QOL domains). In addition, multiple linear regression analysis was not applied to determine the parameters most predictive of the interesting outcomes because there was not found any eligible predictor from the univariate regression models (eligibility criteria: all variables that were significant in univariate analysis at P < 0.1 could include in the multivariate linear regression model). Graphs were drawn using Excel software version 2016.
3.5. Ethical Considerations
The research was carried out after receiving the ethics code from Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1397.917). To collect data, after obtaining the necessary permits, the researcher visited the related medical centers and obtained the subjects' written informed consents, while explaining the purposes and the method of research to them. The patients were informed about the research objectives and procedures, safety of the procedures, confidentiality of the information, anonymity, voluntary nature of the study, and the right to withdraw from the research at any stage of the research.
4. Results
This study was conducted on 150 patients suffering from SCD. The patients aged from 18 to 47 years, with the mean age of 27.56 ± 9.14 years. The duration of the disease ranged from 2 to 45 years, with the mean duration of 25.44 ± 9.2 years. Among the participants, 64% were male, 60% were single, and 12.7% had academic degrees. Other demographic variables have been presented in Table 1.
| Demographic Variables | Values | Physical Health | Mental Health | Social Health | Environment Health |
|---|---|---|---|---|---|
| Age | 27.56 ± 9.14 | -0.077 | -0.077 | -0.063 | -0.075 |
| P-value b | - | 0.346 | 0.352 | 0.447 | 0.362 |
| Gender | |||||
| Female | 54 (36) | 50.38 ± 9.92 | 46.98 ± 9.75 | 47.31 ± 21.96 | 47.07 ± 11.47 |
| Male | 96 (64) | 51.03 ± 10.00 | 46.06 ± 10.28 | 44.06 ± 18.67 | 48.37 ± 11.92 |
| P-value c | - | 0.838 | 0.473 | 0.369 | 0.801 |
| Level of education | |||||
| Illiterate | 9 (6) | 48.66 ± 6.55 | 49.33 ± 10.52 | 40.88 ± 27.73 | 45.33 ± 10.30 |
| < Diploma | 61 (40.7) | 48.22 ± 8.11 | 42.88 ± 8.10 | 43.77 ± 17.94 | 45.72 ± 11.49 |
| Diploma | 61 (40.7) | 54.09 ± 11.31 | 49.72 ± 10.99 | 46.91 ± 19.76 | 51.03 ± 11.43 |
| University | 19 (12.7) | 49.47 ± 9.51 | 45.57 ± 9.17 | 46.57 ± 23.15 | 46.10 ± 12.71 |
| P-value d | - | 0.038 | 0.001 | 0.648 | 0.139 |
| Marital status | |||||
| Married | 60 (40) | 50.80 ± 9.28 | 46.58 ± 8.59 | 45.48 ± 18.11 | 48.05 ± 10.45 |
| Single | 90 (60) | 50.80 ± 10.41 | 46.26 ± 10.98 | 45.06 ± 21.12 | 47.81 ± 12.58 |
| P-value e | - | 0.944 | 0.573 | 0.659 | 0.752 |
| Habitat | |||||
| Province | 56 (37.3) | 51.00 ± 10.18 | 47.60 ± 10.57 | 48.21 ± 22.79 | 49.30 ± 10.82 |
| City | 75 (50) | 50.74 ± 9.95 | 45.64 ± 8.63 | 45.05 ± 17.47 | 47.26 ± 11.73 |
| Village | 19 (12.7) | 50.42 ± 9.72 | 45.78 ± 13.55 | 37.15 ± 18.53 | 46.31 ± 14.39 |
| P-value d | - | 0.987 | 0.370 | 0.201 | 0.300 |
| Duration of disease per year | 25.44 ± 9.21 | -0.009 | -0.013 | -0.046 | -0.076 |
| P-value b | - | 0.912 | 0.875 | 0.573 | 0.357 |
a Values are expressed as mean ± SD or No. (%).
b Pearson test for quantitative variables.
c Based on Mann-Whitney U test.
d KrusKal-Wallis test for non-parametric variables.
e Based on independent sample t-test for parametric variables.
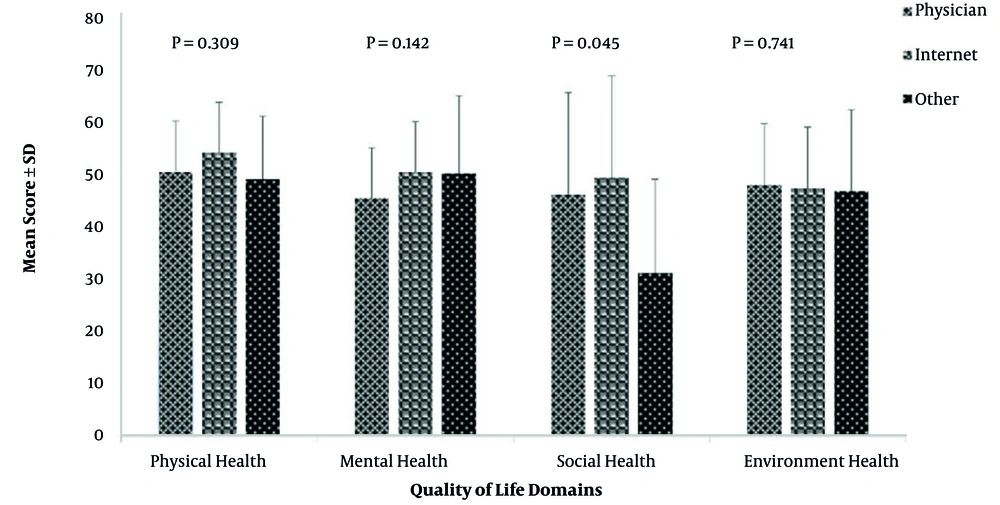
The second part of the results section deals with the knowledge resources among the patients. All patients intended to enhance their knowledge after the confirmation of the disease diagnosis. The most important knowledge-increasing resource was the physician among 83.3% of the patients (n = 125). Additionally, physicians and the internet were expressed as the main ways of acquiring knowledge among 97.3% (n = 146) and 42.4% (n = 59) of the patients, respectively. Moreover, 43.3% (n = 65) and 24% (n = 36) of the patients had acquired knowledge regarding the symptoms and causes of the disease, respectively. Moreover, the findings of the present study showed that 62% (n = 94) and 6% (n = 9) of patients, with the receipt of information from physicians and the internet, respectively, the number of their referrals to medical centers has decreased and 18% (n = 28) and 2% (n = 3) reported that receiving information from physicians and the internet had no effect on the number of their referrals to medical centers. However, no significant relationship was observed between the information resources and the number of referrals to the hospital (P = 0.901). Other information in this area has been depicted in Table 2 (Figure 1).
| Areas of Knowledge Acquisition of Patients with SCD | No. (%) |
|---|---|
| Items that require knowledge acquisition | |
| Causes of the disease | 36 (24) |
| Symptoms of the disease | 65 (43) |
| Treatment of the disease | 11 (7.3) |
| Prevent disease progression | 12 (8) |
| disease side-effects | 4 (2.7) |
| Diet | 8 (5.3) |
| The role of exercise in improving the disease | 9 (6) |
| Complementary and other treatments | 3 (2) |
| The impact of resources on the number of visits | |
| The number of my visits has increased. | 3 (2) |
| The number of my visits has decreased. | 114 (76) |
| It did not affect my visit to the doctor. | 33 (22) |
| The impact of knowledge on the healing process | |
| Very much | 10 (6.7) |
| Much | 60 (40) |
| To some extent | 54 (36) |
| Low | 22 (14.7) |
| Very low | 2 (1.3) |
| It had no effect at all. | 2 (1.3) |
| Ensuring the accuracy of the information | |
| Consult a physician | 116 (77.3) |
| Nurse or hematology center staff | 16 (10.7) |
| Individual diagnosis | 7 (4.7) |
| Experience of other patients with sickle cell | 10 (6.7) |
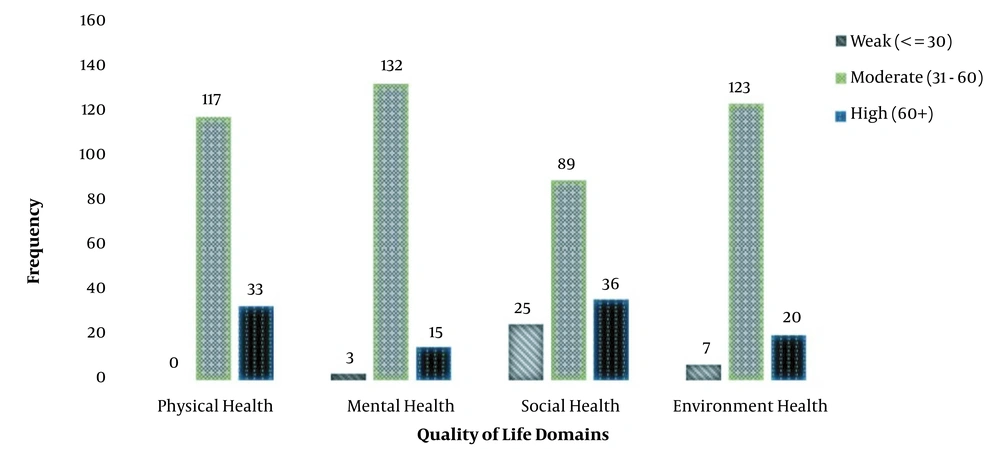
The third part of the results section involves the patients’ quality of life. The quality of life in dimension of physical health, Mental Health, Social Health and environmental health was moderate in 78% (n = 117), 88% (n = 132), 59.3% (n = 89) and 82% (n = 123), respectively (Figure 2). According to the findings, the highest score on quality of life was related to the physical health dimension 50.80 ± 9.94, while the lowest one was related to the social health dimension 45.23 ± 19.91. The scores of environmental health and mental health dimensions were also 47.90 ± 11.74 and 46.39 ± 10.07, respectively.
To examine the relationship between demographic variables and dimensions of quality of life according to the type of variable and its levels, correlation tests were used. The results are given in Table 1. Findings of this part of the study showed statistically significant differences only between patients’ education level and mental health quality of life (P-Value = 0.001). However, no significant relationship was observed between the information resources and the number of referrals to the hospital (R-Pearson = 0.901).
Also, according to Table 3, each of the independent variables, such as patient's characteristics and sources of knowledge increased, were entered into the univariate linear regression model individually (Table 3). The results showed statistically significant differences between place of residence with the dimension of social health (P = 0.037, b = -11.05) and sources of knowledge enhancement with the dimension of social health quality of life (P = 0.010, b = -14.96). According to the Beta values in regression results, increasing age, duration of the disease, and sources of knowledge had a reducing effect on all aspects of quality of life except social health, but there were no statistically significant differences between them. Regarding gender, however, both physical and environmental health showed higher scores in men than women, but the scores other two domains decreased in them. The average score of all aspects of quality of life except physical health was decreased in single people compared to married. Although the regression results revealed the tendency to decrease, it is not statistically significant. In this model, the regression of demographic-clinical variables and health literacy (information sources) account for 6 and 10 percent of the total variance of the score of quality of life, respectively.
| Outcomes | Physical Health | Mental Health | Social Health | Environment Health | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameter | Beta | 95% CI for Beta | t | P | Beta | 95% CI for Beta | t | P | Beta | 95% CI for Beta | t | P | Beta | 95% CI for Beta | t | P |
| Age | -0.08 | (-.26,.09) | -0.95 | 0.346 | -0.08 | (-.26,.09) | -0.93 | 0.352 | -0.13 | (.48,.21) | -0.76 | 0.447 | -0.096 | (-.30,.11) | -0.92 | 0.362 |
| Duration of disease | -0.009 | (-.18,.16) | -0.11 | 0.912 | -0.01 | (-.19,.16) | -0.16 | 0.875 | -0.100 | (.45,.25) | -0.56 | 0.573 | -0.096 | (-.30,.10) | -0.92 | 0.357 |
| Gender | ||||||||||||||||
| Female | Ref | - | - | - | Ref | - | - | Ref | - | - | Ref | - | - | |||
| Male | 0.64 | (-2.7,3.9) | 0.38 | 0.706 | -0.91 | (-4.3,2.4) | -0.54 | 0.593 | -3.25 | (9.9,3.4) | -0.96 | 0.339 | 1.30 | (-2.6,5.2) | 0.65 | 0.517 |
| Marital status | ||||||||||||||||
| Married | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - |
| Single | 0.00 | (-3.2,3.2) | 0.00 | > .99 | -0.31 | (-3.6,3.01) | -0.19 | 0.851 | -0.41 | (6.9,6.1) | -0.13 | 0.901 | -0.23 | (-4.1,3.6) | -0.12 | 0.903 |
| Level of education | ||||||||||||||||
| Illiterate | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - | Ref | - | - | |
| High school | -0.43 | (-7.2,6.3) | -0.13 | 0.89 | -6.44 | (-13.2,.36) | -1.87 | 0.063 | 2.88 | (11.2,17.0) | 0.40 | 0.688 | 0.38 | (-7.7,8.5) | 0.09 | 0.925 |
| Diploma | 5.43 | (1.3,12.2) | 1.58 | 0.11 | 0.38 | (-6.4,7.19) | 0.11 | 0.911 | 6.029 | (-8.1,20.1) | 0.84 | 0.401 | 5.69 | (-2.4,13.8) | 1.38 | 0.170 |
| University | 0.80 | (-6.9,8.5) | 0.21 | 0.83 | -3.75 | (-11.4,3.9) | -0.96 | 0.338 | 5.690 | (10.3,21.7) | 0.70 | 0.484 | 0.77 | (-8.4,10.0) | 0.16 | 0.869 |
| Habitat | ||||||||||||||||
| Province | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - |
| City | -0.25 | (-3.7,3.2) | -0.14 | 0.88 | -1.96 | (-5.4,1.5) | -1.10 | 0.272 | -3.16 | (10.0,3.7) | -0.91 | 0.366 | -2.03 | (-6.1,2.0) | -0.98 | 0.329 |
| Village | -0.57 | (-5.8,4.6) | -0.22 | 0.82 | -1.81 | (-7.1,3.4) | -0.68 | 0.499 | -11.05 | (-21.4,.69) | -2.11 | 0.037 | -2.98 | (-9.1,3.1) | -0.96 | 0.341 |
| Job | ||||||||||||||||
| Employed | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - |
| Student | 3.52 | (6.3,13.4) | 0.70 | 0.482 | 3.48 | (-6.3,13.3) | 0.70 | 0.485 | 2.93 | (17.6,23.5) | 0.28 | 0.779 | 4.35 | (-7.2,15.9) | 0.74 | 0.459 |
| Housewife | 0.96 | (9.2,11.1) | 0.19 | 0.851 | 2.50 | (-7.6,12.6) | 0.49 | 0.626 | -1.82 | (22.9,19.3) | -0.17 | 0.865 | 3.50 | (-8.4,15.4) | 0.58 | 0.562 |
| Jobless | -0.46 | (10.6,9.7) | 0.09 | 0.929 | -2.69 | (-12.8,7.4) | -0.52 | 0.601 | -2.21 | (23.4,19.0) | -0.21 | 0.837 | -2.36 | (-14.3,9.6) | -0.39 | 0.696 |
| Increased knowledge resources | ||||||||||||||||
| Doctor | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - | Ref | - | - | - |
| Other sources a | 3.61 | (-2.3,9.5) | 1.20 | 0.23 | 4.99 | (-0.95,10.9) | 1.60 | 0.099 | 3.22 | (8.4,14.9) | 0.55 | 0.586 | -0.64 | (-7.7,6.4) | -0.18 | 0.856 |
| Internet | -1.40 | (-7.1,4.3) | -0.48 | 0.63 | 4.72 | (-1.0,10.4) | 1.63 | 0.106 | -14.96 | (-26.2,3.7) | -2.63 | 0.010 | -1.21 | (-8.0,5.5) | -0.35 | 0.724 |
a Printed sources, family and friends, other infected patients, disease-related training classes.
5. Discussion
The present study aimed to evaluate the knowledge acquisition areas, information resources associated with SCD management, and their relationship with quality of life. To the best of our knowledge, this research is among the rare studies on the relationship between the two above-mentioned variables among patients with SCD.
The results indicated that all patients intended to acquire knowledge about their disease. Speller-Brown et al. also disclosed that most patients and their parents had a relatively high knowledge level about SCD (33). In a cross-sectional study of health literacy among adult caregivers of children receiving chronic transfusion therapy and adolescents with SCD personally receiving chronic transfusion therapy, 34% of caregivers and 69% of adolescents had inadequate health literacy based on standardized testing, and low health literacy was associated with lower disease-specific knowledge (34). The results of a study by Perry Caldwell and Killingsworth showed that acquiring knowledge had a positive impact on the patients’ treatment process and assisted them in the management of the disease (23). The results of a meta-analysis also disclosed that the patients with higher health literacy and knowledge about the disease showed better adherence to treatment (35). In the same vein, Van Der Heide et al. conducted a study on Dutch patients with diabetes in 2013 and reported a significant positive relationship between the patients’ health literacy and their self-management and general health (36).
The findings of the current study showed that in spite of the daily increasing tendency to use the virtual space and the availability of the internet, physicians were the most common resource for acquiring knowledge. These results were in agreement with those obtained by Mayer et al., Salehi et al., and Farzin et al. (31, 37, 38). This implies that the patients considered their physicians as a reliable information resource, and information transfer would be successful in case of the existence of an appropriate relationship between the patients and physicians and other members of the treatment team (39). Generally, patients expect their physicians to provide them with all their required information. Nonetheless, this is not always possible due to time limitations, physician’s impatience, weak communication skills, carelessness about the patient’s need for information, and differences in the patient’s and physician’s linguistics concepts (39, 40). Nurses should be used to solve this problem because patient education is an independent nursing practice and is one of the main and inevitable responsibilities of this profession (41). Nurses have more access to patients and their families, and they spend a lot of time caring for patients. They can even evaluate the training given to patients based on the nursing process (42).
In the present study, most patients intended to increase their knowledge about the symptoms and causes of the disease. However, they were not willing to acquire knowledge about the disease complications. It seems that acquiring information about the disease symptoms was more important for the patients because they were involved in the disease for a long time period. Babalola et al. demonstrated that most mothers of infants with SCD did not have any information about the disease inheritance patterns, which indicated that they intended to acquire knowledge about the causes and complications of the disease, which seemed to be their main concern (43).
The present study investigated the quality of life of patients suffering from SCD. Based on the results, the highest mean score of quality of life was related to the physical health dimension, followed by environmental health, mental health, and social health dimensions. In the research by Roberti et al., the highest score on the quality of life was related to the social health dimension, while the lowest score was related to the environmental health dimension (44). Dampier et al. stated that the lowest score on quality of life was related to the physical health dimension (45). Another study also showed that the lowest score on quality of life was related to the physical health dimension, including physical activity and independent function, among children (10). These results were contrary to those of the present investigation.
A study was conducted at King Khalid University to describe the QoL among university students (46). The university students demonstrated significantly better physical functioning and general health compared with the quality of life of patients with SCD in Saudi Arabia. Surprisingly, the bodily pain among the university students was even worse compared with Saudi Arabia patients with SCD (47). The results of a study by Ahmed et al. and McClish et al. show that adolescents with SCD had more physical pain and poorer social functioning than adults with SCD (47, 48). In this study, the highest score on quality of life was associated with the physical health dimension. The results of these studies show that the presence of disease and manifestations such as pain in patients has a greater impact on the social and psychological performance of patients, while in the general population, clinical manifestations have a greater impact on physical health. A recent meta-analysis has similarly reported that the perceptions of consequences an illness may have and emotional representations dimensions have the strongest relationships with psychological outcomes, including QOL, across a wide range of illnesses such as cancer, epilepsy, heart failure, rheumatoid arthritis, and pulmonary diseases (49). In SCD, the illness can be devastating with multiple hospitalizations and possibility of life-threatening complications. Patients can be emotionally affected by seeing negative outcomes among their peers. The illness can be quite unpredictable, and it is yet difficult to predict an individual’s life course with the illness (50).
The current study findings also demonstrated that the disease had a negative impact on the patients’ social and mental functions. The low score of the social dimension might be attributed to the fact that the patients were faced with problems in conformity to the disease or were not supported by the society, directing them towards isolation from the society. Furthermore, several studies have shown that patients with SCD experienced various mental problems, such as low self-esteem, death anxiety, role limitation due to emotional problems, and reduced concentration, followed by functional problems. These results were consistent with those of the present investigation, indicating the need for serious measures regarding the mental health dimension of quality of life (44, 51, 52).
Another important finding of this study was the statistically significant difference between the dimension of social health and sources that increase knowledge. These results were in line with most of the results of studies Jovanik et al., Zheng et al., and Farghadani et al. conducted in this field and did not match the results of Couture et al (53-56).
The present research evaluated the relationship between the quality of life dimensions and demographic variables. The results revealed a significant relationship between the mental health dimension of quality of life and the patients’ education level. Similarly, Adzika et al. reported that education level was significantly associated with the SCD patients’ quality of life, but not with their anxiety (57). The higher the patients’ education level, the higher they would be able to use the available methods for management of the disease, use self-care, collect their required information, and take part in therapeutic decision-making processes. The results also showed a significant relationship between the knowledge resources and the social health dimension.
The findings of the current study can be used as a basis for further investigations on the efficiency of educational programs regarding increasing the SCD patients’ knowledge of their disease and standardization of educational programs. Because nurses spend more time with the patient than other members of the treatment team, it is worthwhile to educate the patient with SCD about disease information and remove barriers to education that can have a detrimental effect reduce on the health dimensions physical, psychological, social, and environmental (58). It seems that the continuation of supportive and educational care by nurses in different stages of diagnosis and treatment of this disease. Therefore, the existence of permanent centers for this is necessary, which requires serious attention of officials in this regard.
5.1. Study Limitation
In the present study, the data were collected using a self-report questionnaire. Considering the subjective nature of quality of life, different individuals might have had various perceptions of this concept and provided different responses. Therefore, systematic error might have occurred. Moreover, most of the study participants were Arab, which might affect the generalizability of the results. Finally, further longitudinal studies with larger sample sizes are recommended to assess the quality of life.
5.2. Conclusions
Most patients referred to physicians as the most important source of increasing the level of knowledge. In addition, the most important reason for patients to increase their awareness was the causes and symptoms of the disease. In addition, the average quality of life of patients in the areas of physical health and social health received the highest and lowest scores, respectively. The results also revealed a significant relationship between the knowledge resources and the social health dimension of quality of life. Therefore, emphasizing the concept of health literacy in the healthcare system leads to increasing the knowledge and awareness of patients and their primary caregivers in the field of disease. It is also one of the indicators of the quality of nursing care is educating patients and giving effective information. On the other hand, the issue of health literacy and patient education has an impact on all aspects of nursing, treatment, and costs. Therefore, nursing managers should identify barriers to patient education by nurses and seek to remove them. Also, evaluation of the quality of life by nurses as a health determinant is necessary for policymaking and specific measures appropriated to particular features. Therefore, interventions are suggested to be planned to increase SCD patients’ exhilaration and improve their mental and social health, eventually enhancing their quality of life.