1. Background
With a prevalence of about 1% of the total population, schizophrenia is a significant mental health problem worldwide and stressful for patients and their families (1, 2). In Iran, prevalence studies have revealed that 78% of people in the countryside experience schizophrenia (3). Although antipsychotic drugs are the primary treatment for schizophrenic patients, despite their effectiveness, about two-thirds of patients may experience positive and negative symptoms during their lifetime (4). Based on the presence or absence of positive and negative symptoms, schizophrenia can be divided into two types, one and two. Positive symptoms include hallucinations, delusions, abnormal behavior, and thought disorders. The brain structure in these patients is normal, and they respond well to treatment. Negative symptoms include anhedonia, apathy, flat affect, and lack of attention. In addition, there are abnormalities in the brain structure of these patients. Also, these patients do not respond well to treatment (5). One of the biggest challenges in the treatment of schizophrenic patients is the treatment of negative symptoms. Sometimes even a year after the last episode of the disease, negative symptoms are seen in about 50% of patients (6).
Compared to other psychiatric disorders, most psychiatric beds are reserved for patients with schizophrenia (7). Living with a person with a mental health condition has difficulties, some of which are family exhaustion, worry about the recurrence of syndrome symptoms, misgiving about the cause of the disorder, and the stigma of mental illness (8). However, established family environments can predict improving symptoms and social functioning in psychiatric patients (9). Accordingly, family caregivers can be valuable for patients facing major psychiatric disorders. Therefore, by increasing their knowledge about the family member’s disorder, they can help their sick member through therapeutic support (10). This has caused more attention to the patient’s living environment in the last decade. According to experts, as the patient’s life context plays a fundamental role in improving or worsening the disease and its prognosis, this issue has led mainly to the expansion of psychological interventions (focusing on the patient’s primary caregivers) (11). Such treatment programs focused on caregivers can help the family better understand the disorder’s nature, therapeutic interventions, and prognosis (12).
According to the meta-analyses, drug therapy can only have limited effects on the negative symptoms of schizophrenia (13). In their study, Leucht et al. showed that only four groups of second-generation antipsychotics were more effective than first-generation antipsychotics in negative disease symptoms (with an effect size between 0.13 and 0.32). Also, in the analogy between second-generation antipsychotics and placebo, the mean difference (0.39) favored second-generation drugs (14). There is good evidence that pharmacotherapy combined with family-focused programs is a more effective treatment for schizophrenia than medication alone (15).
However, Makinen et al. indicated that the impact of programs focused on the primary caregivers of patients or psychological education to them did not have satisfactory effects on the negative symptoms of patients (16). However, many meta-analyses have provided evidence of the effectiveness of cognitive behavioral therapy (CBT) on the symptoms of schizophrenia, emphasizing CBT for routine care (RC) in the treatment of schizophrenia (17). According to Hassan et al.’s research, the psychoeducational program showed a significant improvement in the severity of the disease symptoms immediately and three months after the intervention (18). Also, Kheirabadi et al. (19) evaluated the efficacy of a need-assessment–based educational program compared with a current program (textbook based) in treating schizophrenia. They concluded that the Positive and Negative Syndrome Scale (PANSS) total score in both experimental and control groups was significantly decreased, but this decrease was considerably more in the intervention group than in the control group. However, the separate scores of positive and negative symptoms decreased only in the intervention group, and the decrease in these scores was not significant in the control group. The response rate was higher in the intervention group, and the relapse rate was lower in this group. In logistic regression analysis, need–assessment–based psycho-education was associated with more treatment response. In Sharif et al.’s study (20), in the experimental group, the intensity of the disorder’s symptoms and the pressure on the patient’s caregivers significantly decreased immediately and two months after the intervention.
In the present article, we report the effects of familial psychoeducational intervention and medication strategies on patients’ positive and negative symptoms. In a randomized study, psycho-social rehabilitation training and single drug control by Wang et al. (21), the intervention group showed significantly lower scores on the scale of positive and negative symptoms of schizophrenia than the control group after treatment.
2. Objectives
This study aims to investigate the effectiveness of family psychological training as an additional treatment for drug therapy in hospitalized patients with schizophrenia in reducing the negative and positive symptoms of patients.
3. Methods
3.1. Study Design
This study, as a semi-experimental design, was designed as a randomized controlled experimental study.
3.2. Study Population and Sampling
The study population included family caregivers of patients with schizophrenia whose patients were admitted to the psychiatric wards of Shiraz Psychiatric Hospital at the time of sampling from 11 September 2015 to 31 March 2016. Affiliated with Shiraz University of Medical Sciences, this hospital was the largest psychiatric hospital in southern Iran, with 500 beds for psychiatric patients.
According to Cohen (22), to achieve α of 0.05, an effect size of 0.50, and a test power of 0.88, a total of 20 patients was needed for each group. Therefore, this study selected 50 schizophrenic inpatients (10 extra patients were selected due to the anticipated loss of more subjects) who were referred to Shiraz Psychiatric Hospital from September 2016 to May 2017.
3.3. Intervention Procedure
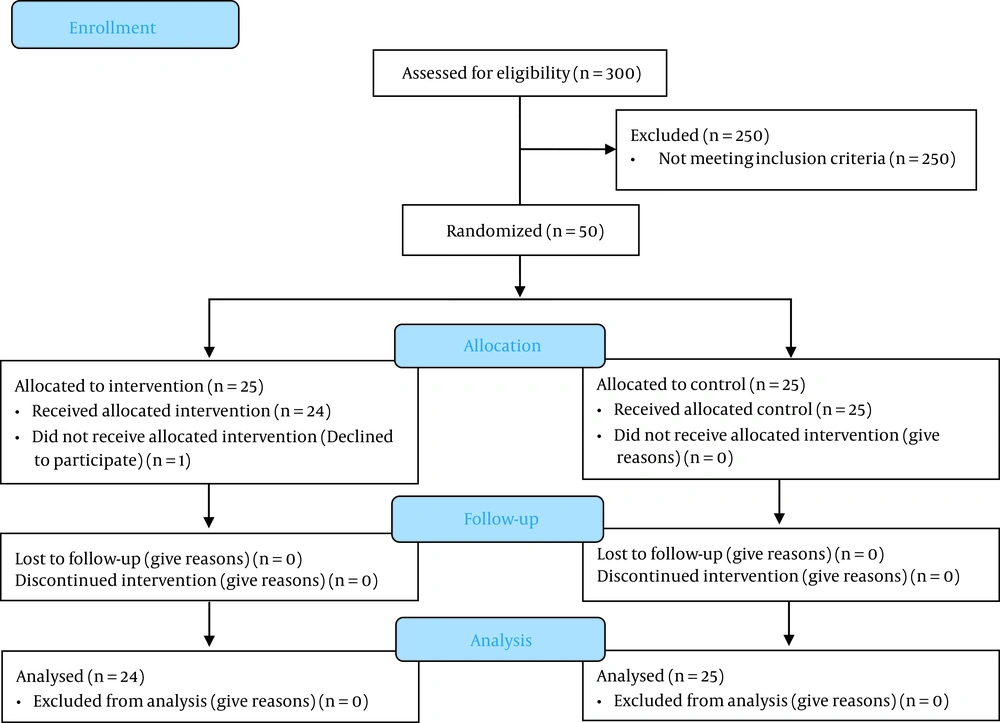
The familial psychoeducational intervention commenced in the hospital for families during the patient’s admission. The patients were selected by convenience sampling. For data collection, a clinical psychologist administered the evaluation scale to all patients in three stages: Before the intervention, at discharge, and two months after discharge (Figure 1). All patients in both groups (25 cases and 25 controls) received pharmacological therapy and care without an organized education program. In this case, 49 Iranian inpatient caregivers were randomly allocated to the experimental (n = 24, one of the patients in the intervention group was removed from the study because of legal issues) or control (n = 25) groups. The intervention group participated in a six-session, 90-minute familial psychoeducational program (an explicit, step-by-step protocol) for three weeks (Table 1). The program lasted nine hours with the family in the hospital. One of the features of this treatment package was its ease of implementation, which did not require special skills for therapists. In addition, this treatment package is easily adjusted to the demographic factors of a specific Iranian inpatient. Participants and practitioners collaborated to identify individual target behaviors and goals in this schedule. The control group merely got pharmacological therapy. Inclusion criteria were an age of 20 - 70, a diagnosis of schizophrenia disorder according to DSM-5 criteria within the preceding two years, no other axis 1 disorder during recruitment, and living with a caregiver three months before hospitalization; also, all caregivers invited to participate must be the primary caregiver with the greatest responsibility for providing care within the family. The exclusion criteria for the study were the family’s participation in another psychoeducational program within the preceding year, caring for more than one family member with mental illness, substance abuse problem in the patient or caregiver, symptoms of serious suicidal thoughts in patients or their caregivers, severe medical illness preventing the continuation of the treatment, brain damage, or more than one session absence of group. For moral principles, participants in the control group were invited to take the familial psychoeducational program at the end of the research. The intervention in the experimental group for all participants and all sessions was conducted by the same clinical psychologist who had worked in clinical psychotherapy for at least 15 years.
| Session | Topic | Handouts | Practice |
|---|---|---|---|
| 1 | Introduction and family story, group rules, and the orientation of caregivers to the program | - | Knowledge of schizophrenia assessment |
| 2 | Understanding schizophrenia and its symptoms | What is psychosis? | Practicing the warning signs |
| 3 | Treatment and follow-up. Orienting caregivers on the warning signs of relapse and relapse prevention | Recovery from psychosis | Practicing the warning signs |
| 4 | What help can the family do? Improving communication skills in the family | How to help patients with psychosis? How to respond to delusions and manage hallucinations and anger | Identifying the signs and signals for help |
| 5 | Problem-solving skill | Problem-solving | Practicing problem-solving skills |
| 6 | Specific issues and crisis prevention. A review and summary of the past sessions. | Reducing the risk of recurrence and preventing the crisis | - |
The Schedule of Familial Psychoeducational Intervention
Instruments: First, demographic information was collected using a questionnaire. After identifying the experimental and control groups, the PANSS was applied to both groups. This scale was developed by Kay et al. (23) to specifically assess positive and negative symptoms of schizophrenia and general psychopathology. The PANSS measures 30 clinical symptoms of schizophrenia; each symptom is scored from 1, indicating the absence of psychopathology, to 7, indicating severe psychopathology, with higher scores indicating poorer mental health status. Internal reliability and criterion-related validity are 0.77 (positive scale) and 0.77 (negative scale), and 0.52 with the Clinical Global Impression-Severity Scale (CGI-S) (24). This scale is one of the most commonly used tools for schizophrenic patients, as it has been used in numerous clinical trials to evaluate treatment success and relapse (25). Today, this scale is used in clinical and research environments and is a reliable tool for assessing symptoms (26).
3.4. Ethical Consideration
Before entering the research, the interests of the study and the optionality of participation were explained to the subjects, and written consent was received from them. Conditions were provided for the control group subjects to participate in the family psychological training intervention program if they wished. It was also emphasized that they could withdraw from the research if they did not intend to cooperate.
3.5. Statistical Analysis
Descriptive statistics were used to display the mean and standard deviation (SD) in both groups, and the ANCOVA method was used to determine the effectiveness of the psychological intervention on schizophrenia symptoms. Data were analyzed using SPSS version 20 software. The significance of the findings was evaluated at the significance level of P < 0.01.
4. Results
A summary of the socio-demographics of heads of households (families) and patients is presented in Tables 2 and 3. In total, 62% of the caregivers were females, with an average age of 37.36 ± 10.242 years. Most of them were between 51 and 60 years (42%), and the lowest age range was under 30 years (6%). Caregivers were mothers (40%), followed by spouses and brothers (16% each), fathers (14%), sisters (8%), children (4%), and others (2%). The most school education frequency was related to high school (48%). Table 4 indicates the mean and standard deviation of PANSS in both groups. The preliminary results showed no statistical difference between the groups’ PANSS scores at the beginning and posttest (Table 5). In the posttest evaluation, both groups showed a relatively similar reduction in PANSS. However, there was no significant difference between the groups. The same reduction trend was seen in the follow-up stage (two months after). Compared to the control group, participants in the intervention group showed statistically significant improvements in PANSS scores at the two-month follow-up (Table 6).
| Components | Frequency (%) |
|---|---|
| Sex | |
| Men | 19 (38) |
| Women | 31 (62) |
| Age | |
| Under 30 | 3 (6) |
| 31 to 40 | 4 (8) |
| 41 to 50 | 14 (28) |
| 51 to 60 | 21 (42) |
| 60 or above | 8 (16) |
| Relative | |
| Father | 7 (14) |
| Mother | 20 (40) |
| Spouse | 8 (16) |
| Sister | 4 (8) |
| Brother | 8 (16) |
| Children | 2 (4) |
| Other | 1 (2) |
| Occupation | |
| Jobless | 2 (4) |
| Public | 8 (16) |
| Privet | 13 (26) |
| Housewife | 27 (54) |
| Marital status | |
| Single | 5 (10) |
| Married | 31 (62) |
| Divorced | 6 (12) |
| Widow | 8 (16) |
| Education | |
| Guidance | 13 (26) |
| High school | 24 (48) |
| Collegiate | 13 (26) |
Socio-demographics of Heads of Households (Families)
| Component | Frequency (%) |
|---|---|
| Sex | |
| Men | 36 (72) |
| Women | 14 (28) |
| Age | |
| Under 30 | 14 (28) |
| 31 to 40 | 18 (36) |
| 41 to 50 | 12 (24) |
| 51 to 60 | 6 (12) |
| 60 or above | 30 (60) |
| Marital status | |
| Single | 13 (26) |
| Married | 6 (12) |
| Divorced | 1 (2) |
| Family history | |
| Yes | 28 (56) |
| No | 22 (44) |
| Addiction history | |
| Yes | 13 (26) |
| No | 37 (74) |
| Alcohol history | |
| Yes | 3 (6) |
| No | 47 (94) |
| Occupation | |
| Jobless | 43 (86) |
| Public | 7 (14) |
| Privet | 0 (0) |
| Housewife | 0 (0) |
| Education | |
| Widow | 2 (4) |
| Guidance | 22 (44) |
| High school | 22 (44) |
| Collegiate | 4 (8) |
Socio-demographics of Patients
| Time | Mean ± SD |
|---|---|
| Pretest | |
| Experimental | 82.5 ± 12.594 |
| Control | 84.72 ± 9.629 |
| Posttest | |
| Experimental | 50.08 ± 11.477 |
| Control | 51.92 ± 9.823 |
| Follow-up (two months) | |
| Experimental | 38.54 ± 5.564 |
| Control | 58.56 ± 6.609 |
Means and Standard Deviations for Positive and Negative Syndrome Scale
| Time | t | df | P-Value | |
|---|---|---|---|---|
| PANSS | Pretest | -0.695 | 47 | 0.491 |
| Posttest | -0.603 | 47 | 0.550 |
Positive and Negative Syndrome Scale Scores at Pretest and Posttest in the Intervention and Control Groups
| Time | df | F | P-Value | Eta | |
|---|---|---|---|---|---|
| PANSS | Posttest | 1 | 0.049 | 0.825 | 0.001 |
| Follow-up | 1 | 165.931 | 0.001 | 0.793 |
Positive and Negative Syndrome Scale Scores at Posttest and Two-Month Follow-up and Analysis of Covariance Results (Tests of Between-Subject Effects)
5. Discussion
In addition to drug therapy in schizophrenia, psycho-social approaches are part of the therapy that modify the period of the disease in an excellent way (27). From this standpoint, the present study investigated familial psychoeducational intervention for hospitalized schizophrenic patients in Shiraz. Like many other studies, there is a need for higher levels of familial psychoeducational interventions as a supplemental treatment to pharmacotherapy in inpatients with schizophrenia. The present study focused on the impact of psychoeducational intervention in Iranian families with a schizophrenic member. Our primary goal was to test the hypothesis that familial psychoeducational intervention can reduce the symptoms of schizophrenic inpatients.
In this randomized controlled trial of the effectiveness of family intervention for schizophrenia, both intervention and control groups showed significant clinical improvement at the end of the remedy. However, the improvement was sustained only in the intervention group at eight weeks of follow-up. The results were encouraging. The significant finding of this study was that familial psychoeducational intervention had superior efficacy for psychotic symptoms in partially responsive inpatients with schizophrenia. In general, this finding is in congruence with investigations that examined the effectiveness of family psychoeducational intervention for schizophrenia at a single time point (16, 18-21, 28, 29). As a clear example, Xiong et al. (30) examined family-based intervention for schizophrenic patients in China. They showed that improvements in patients’ symptoms might have been related to enhanced treatment compliance because families could better supervise the patient’s use of antipsychotic drugs. While the findings from foregone studies about schizophrenia are incompatible, most trials have shown that the severity of psychiatric symptoms can be reduced at post-treatment and follow-up (31).
Ahmadi et al. assessed the effectiveness of family psychological training for preventing the recurrence of symptoms in patients with schizophrenia spectrum disorders. The results of covariance analysis showed that familial psycho-education programs, prevented the relapse of negative and positive symptoms in pations with psychosis disorders (32). The findings of Sharma et al.’s research also showed that the PANSS scores of patients in the treatment group significantly decreased after caregivers’ psychological training (33). In this regard, Motaghipour and Tabatabaei’s research also showed that psychological education of patients with severe mental disorders and their families caused a significant reduction in the recurrence rate of symptoms or re-hospitalization and a significant decrease in the psychological burden of the disease and the distress of the families (34). Also, Rangrazian et al.’s research indicated that disease management effectively decreased the positive and negative symptoms of schizophrenic patients (35). In line with previous studies, our findings confirmed that adding a brief psychoeducational intervention to routine care in a psychiatric clinic is an effective way to ameliorate the significant symptoms of schizophrenia.
5.1. Conclusions
Across the psycho-social approaches for curing psychotic disorders, family psycho-education is the most commonly used. The target of the training of families who have a member with schizophrenia is to decrease return rates, reclaim family functions, and raise collaboration and treatment admission.
The current research indicated that the family psychological education program for patients with schizophrenia helps improve the conditions and management of these patients by providing specialized and targeted care. The family psychological intervention program helps improve the positive and negative symptoms of the disorder more stably by reducing the environmental stress of the patient and making them commit to taking medication. Also, such programs increase the effectiveness of the care provided by health workers, psychiatrists, clinical psychologists, and patient caregivers. Therefore, the patient caregiver’s comprehensive, dedicated, and specialized caring, can lead to the patient’s trust in the family, therapist, medication, and psychotherapy programs. Therefore, the research results can be used to prevent early relapse and re-hospitalization. This will be possible by planning to increase the awareness of schizophrenic patients’ caregivers and improve the relationship between the patients and their families. It is also suggested to provide such interventions for the families of schizophrenic outpatients.