1. Background
Multiple sclerosis (MS) is a highly prevalent disease in young people caused by the degeneration of the myelin sheath of neurons in the central nervous system (CNS) (1, 2). The prevalence of MS is 100 per 100,000 people in Iran, and women are two to three times more likely than men to be afflicted by MS (3). This chronic and progressive disease runs an unpredictable yet homogeneous course, following an advanced secondary stage and a common mild period (4). Multiple sclerosis leads to a wide range of neurological symptoms, e.g., blurred vision, loss of balance, muscle weakness, and sensory disturbances (5). Recent research has implicated environmental, genetic, immunological, and microbiological factors in its etiology (6, 7). Multiple sclerosis is classified as an autoimmune disease in which the immune system attacks the brain and spinal cord, thereby disrupting their functioning. Since the CNS links all bodily functions and activities, MS can cause various side effects (8, 9).
Problems with balance and controlling the body’s position are the most common challenges experienced by patients with MS with a high rate of falls (10). Numerous studies have confirmed that MS patients’ falling is associated with their dynamic balance disorder. Based on the literature, people who had experienced falling demonstrated poorer performance on balance and up-and-go tests, which assess imbalance in walking and transitions (11, 12). Fear of falling (FOF) is described as a constant concern about falling that may eventually limit daily activities, diminish self-confidence in balance, and ultimately lead to muscle weakness, immobility, and reduced quality of life (13). It can also cause psychological impacts, such as fatigue, lack of social participation, and isolation. Fear of falling can thus cause psychological as well as physical injuries in patients (14). Patients with MS suffer from musculoskeletal, neurological, and balance disorders. The Tinetti test, clinical tests (e.g., standing on one foot, standing with eyes closed, standing with legs open and closed), and walking time test have shown that patients with MS have serious trouble with balance. Balance depends on visual, proprioceptive, and vestibular senses, as well as appropriate motor responses, which are impaired in patients with MS and diminish their balance (15, 16).
Multiple sclerosis as a chronic disease causes depression, anxiety, worry, hopelessness, and disability in performing occupational tasks and social functioning while also negatively impacting familial relationships (17). Disability is a serious symptom and consequence of MS. Disability means the existence of a functional problem at the physical, personal, and social level in one or several areas of life in interaction with environmental factors and health conditions (18, 19). The clinical features of the disease and the emotional and psychological problems of patients with MS lead to disability in different spheres of life, including diminished ability to adapt to the disease, occupational dysfunction, decreased ability to move and walk, fatigue, and aggravated life problems (20). Disability leads to emotional distress and is a major dimension of MS patients’ reduced quality of life. People with MS experience different degrees of disability, and this disease is a common cause of disability in young people (21, 22). Common motor symptoms associated with disability in patients with MS include diminished balance, strength, endurance, and walking speed (23). Scholz et al. (10) showed that patients with MS who had a greater FOF were more likely to fall, walked more slowly, took shorter strides, had a larger ellipse sway area, and suffered from a severer disability.
Imbalance in MS and loss of coordination of organs begin with muscle weakness and spasms. Falling is one of the biggest problems that result from an imbalance in MS. Some patients with MS are out of balance when walking, and their gait is uncoordinated. Examining the factors affecting functioning and determining their importance can lay the ground for many strategic decisions. As such, it is essential to know which variables and to what extent they affect MS patients' FOF. As a practical objective, the results of this study can help patients with MS control their disease, decelerate its progressive course, enjoy a hopeful life, and experience fewer physical and psychological symptoms. Also, understanding and explaining the relationship between FOF and disability in patients with MS can be a basis for designing and implementing intervention programs to treat these patients.
2. Objectives
Based on the above-mentioned considerations, the present study aimed to investigate the relationship between the severity and FOF mediated by disability in patients with MS.
3. Methods
3.1. Design
This was a correlational study based on structural equation modeling (SEM).
3.2. Participants
The statistical population consisted of all patients with MS who visited the neurology centers of hospitals in Sari, Iran, in 2021, of whom 200 cases were selected as the sample using convenience sampling. The sampling time was from May to July 2021. In this study, the sample size was selected based on the research variables. Therefore, 20 samples were considered for each variable (24). A total of 210 questionnaires were distributed among the participants. After removing ten incomplete questionnaires, the data of 200 questionnaires were analyzed. The inclusion criteria were a history of MS, no serious physical illness, no participation in any psychotherapy intervention within one month before the study, and signing informed consent forms. The exclusion criteria were affliction with physical disease and failure to answer the questions in the questionnaires.
3.3. Ethical Considerations
All ethical considerations were observed in this study; an informed consent form was obtained from the participants, and they were assured that they could freely leave the study whenever they desired. The sampling process began after making the necessary coordination with the Research Department and obtaining the necessary permits. In addition, the data were confidentially analyzed by the researcher. Also, in this study, with the permission of the questionnaire compiler, the Persian version of the questionnaires was used. The study was approved by the Ethical Committee of Islamic Azad University, Tonekabon Branch (code: IR.IAU.TON.REC.1400.028).
3.4. Research Instruments
3.4.1. The Falls Efficacy Scale-International
The Falls Efficacy Scale-International (FES-I) is a 16-item tool that measures the level of concern about falling during 16 social and physical activities based on a four-point Likert scale (1 = not at all concerned to 4 = very concerned). The minimum and maximum scores on this scale are 16 and 64, and scores of 16 - 19, 20 - 27, and 28 - 64 indicate low, moderate, and high FOF, respectively (25). This scale was developed and validated by Yardley et al. (26). Cronbach's alpha coefficient for the scale was 0.70 (27). In the present study, the reliability of this scale based on Cronbach's alpha was equal to 0.80.
3.4.2. Multiple Sclerosis Severity Scale
This scale was measured by a neurologist and given to the researcher. The severity of MS is measured on a scale ranging from 0 to 5 based on the following factors: normal functioning without any restriction in activities or lifestyle, type of MS, duration of disease, disease severity, health, and balance. Scores 0, 1, 2, 3, 4, and 5 represent mild, very low grade, low grade, moderate, severe, and very severe MS, respectively (28).
3.4.3. Kurtzke Expanded Disability Status Scale
Expanded Disability Status Scale (EDSS) was used to evaluate the degree of disability of patients with MS. This scale measures the different states and functions of the CNS. This instrument, along with neurological clinical examinations, assesses the function of the pyramidal tracts, the brain, brainstem, cerebellum, and senses to determine the severity of disability in patients. The respondent’s total score can range from 0 to 10. The interpretation of the scores of the EDSS is as follows: 0: Normal neurological examination; 1 - 1.4: A person without a disability but has some abnormal neurological symptoms; 1.5 - 2.4: The person has the least disability; 2.5 - 4.4: The person has a moderate disability that affects daily activities but can still walk; 4.5 - 7.9: The person has a more severe disability and needs help while walking; 8 - 9.9: The person's disability is very severe and limits him to bed; 10: Death due to MS. Overall, lower scores indicate less disability, and higher scores reflect severer disability (29). This scale was used by a neurologist who collaborated with the study before including the patient in the training program, and the results were given to the researcher.
3.5. Statistical Analysis
Descriptive statistics (mean, standard deviation, and correlation coefficient) were used for data analysis, and SEM was performed to evaluate the proposed model. The Bootstrap method was also adopted to investigate the indirect associations between variables. The data were analyzed using SPSS AMOS software version 25.
4. Results
The demographic data showed that 19.5%, 43.5%, 28%, and 9% of the participants were under 25, 25 - 35, 35 - 45, and over 45 years of age, respectively. In addition, 41.5% were male, and 58.5% of female. In terms of educational attainment, 29.5%, 13.5%, 44.5%, and 12.5% of the participants had a high school diploma, an associate's degree, a bachelor's degree, and a master's or a higher degree, respectively. Table 1 presents the mean, standard deviation (SD), and Pearson correlation coefficients of the research variables.
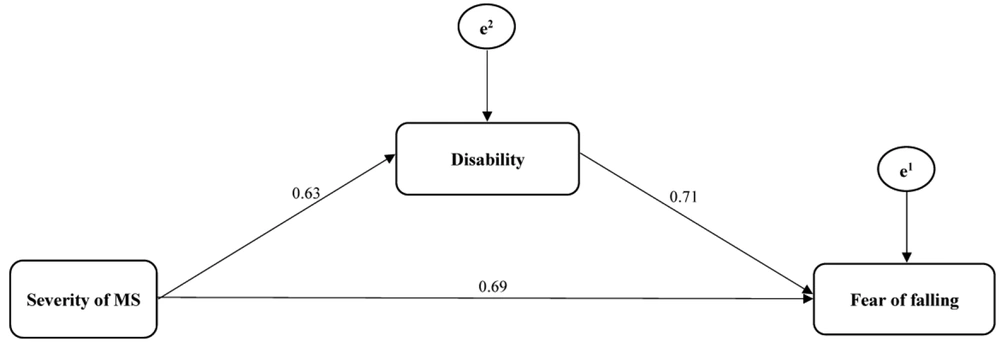
According to Table 2, since the root mean square error of approximation (RMSEA) is equal to 0.014, it can be stated that the proposed model can be finalized without any correction or change. The results confirmed the model’s goodness of fit. The proposed model is shown in Figure 1.
| Fit Indicators | χ2 | df | (χ2/df) | IFI | TLI | CFI | NFI | RMSEA |
|---|---|---|---|---|---|---|---|---|
| Proposed model | 2.46 | 1 | 2.46 | 0.93 | 0.92 | 0.95 | 0.93 | 0.014 |
Abbreviations: IFI, incremental fit index; TLI, Tucker Lewis index; CFI, comparative fit iIndex; NFI, normed fit index, RMSEA, root means square error of approximation.
Table 3 shows the results of estimating path coefficients for testing direct hypotheses. The results showed there was a direct relationship between the severity of MS and FOF (β = 0.69; P = 0.002) and between the severity of MS and disability (β = 0.63; P = 0.001) in patients with MS. Moreover, there was a direct relationship between disability and FOF (β = 0.71; P = 0.011) in patients with MS (Table 3).
| Path | Proposed Model | |
|---|---|---|
| β | P | |
| Severity of multiple sclerosis (MS) to fear of falling | 0.69 | 0.002 |
| Severity of MS to disability | 0.63 | 0.001 |
| Disability to fear of falling | 0.71 | 0.011 |
| Severity of MS to fear of falling through the mediating role of disability | 0.124 | 0.003 |
The bootstrap method was used to evaluate the significance of the intermediary relationship. The results showed a significant indirect path from the severity of MS to FOF through the mediating role of disability in patients with MS (P = 0.003) (Table 3).
5. Discussion
This study aimed to investigate the relationship between the severity of MS and FOF through the mediating role of disability in patients with MS in Sari in 2021. The results showed a positive relationship between the severity of MS and FOF and between the severity of MS and disability in patients with MS. Also, there was a positive relationship between disability and FOF in patients with MS. The results indicated that disability had a mediating role in the relationship between the severity of MS and FOF in patients with MS. These findings are consistent with the research results of a previous study (30).
Multiple sclerosis is a chronic and progressive disease of the CNS. In MS, the myelin sheath that insulates neuron fibers and rapidly transmits information from the brain to other parts of the body is damaged, and messages sent from the nervous system are slowly transmitted or completely stopped. This causes a variety of symptoms, such as imbalance, fatigue, blurred vision, and numbness of the legs or arms (12). Multiple sclerosis is the leading cause of non-traumatic disability in adults and the most prevalent progressive neurological disease in young people. Imbalance, falls, and walking limitations in people with MS can impact a wide spectrum of functions, activities, and participation in daily activities at home, the workplace, and in the community. Falling is a major problem for the healthcare system. The World Health Organization (WHO) cites the FOF as the third leading cause of chronic disability worldwide. People with MS are more likely to fall due to their physical condition (31).
Fear of falling and its ensuing physical and psychological complications affect the health of patients with MS (10). Falling is an event that unintentionally places the person on the ground or on any lower level due to a reduced level of consciousness, sudden bouts of epilepsy, paresis, or stroke. Falling in patients with MS can lead to disability, hospitalization, and death (31). It is, therefore, a serious problem among these patients, and its psychological impacts may lead to mobility impairment and reduced quality of life.
Multiple sclerosis is a chronic disease of the CNS, in which the myelin sheath is locally degenerated. It is the most prevalent non-traumatic cause of neurological disability in young people. Disability is a common symptom in people with MS (11). This disorder, along with other factors, increases the FOF and prevents the patient from performing everyday tasks. The severer the MS, the greater the patient's inability to perform daily tasks.
5.1. Limitations
The most important limitations of the present study are as follows: (1) because it was conducted on patients with MS in Sari, Mazandaran Province, the results should be cautiously generalized to patients with MS in other provinces and regions of Iran, and (2) the research data were collected through questionnaires, and the unconscious data obtained from questionnaires are prone to distortion and may jeopardize the research findings.
5.2. Conclusions
The severity of MS had a positive relationship with FOF and disability in the patients. Moreover, disability had a mediating role in the relationship between the severity of MS and FOF. The results of this study can be used to alleviate disability in patients with MS. Considering the importance of developing a model of FOF, our findings can provide a basis for future studies to investigate stress-induced problems and behavioral disorders, such as depression and develop appropriate psychological interventions. It is also recommended to develop the necessary plans for reducing FOF in patients with MS.