1. Background
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a novel coronavirus. The COVID-19 severity and mortality have been found to be directly associated with age, chronic diseases, and immune system deficiency (1). Therefore, older adults suffering from chronic diseases are at a higher risk of serious complications of COVID-19, compared to others (2). Primary statistics in China Center for Disease Control and Prevention indicated that older adults over 59 years had a higher mortality rate after the onset of COVID-19 symptoms, compared to those aged 30 - 59 years (3). In the same vein, 15% of the first wave of deaths in China occurred among individuals aged over 60 years. Based on the statistics provided by China Center for Disease Control and Prevention, the mortality rate was 3.6% in the age group of 60 - 69 years, which could reach 18% in individuals aged over 80 years (4).
Up to now, there is a paucity of information regarding the impact of COVID-19 on health in general and on older adults’ mental health in particular (5). Nonetheless, COVID-19 has changed the elderly’s daily living activities, care, support, ability to forge social relationships, and perceptions. On the other hand, the World Health Organization has recommended strict quarantine for the elderly population in order to control mortality, specifically in involved countries. Nonetheless, older adults face challenges due to spending more time at home, lack of physical contact with their family and friends, and primary cessation of work and activities (1). In addition, an increase in this group’s vulnerability is accompanied by an increase in their fears and worries (6). Yet, these issues have been less taken into consideration.
During the COVID-19 control, older adults over 60 years suffer from more complicated therapeutic conditions and receive less social support, compared to younger age groups, which usually results from complicated treatment regimens (7). Patients’ adherence to the treatment regimen is one of the behaviors that can predict successful treatment of the disease and reduce its negative complications (8). Adherence to treatment has been defined as conformity of patients’ behaviors to healthcare providers’ recommendations (9). Adherence to therapeutic programs and prescribed medications is one of the major challenges among patients suffering from chronic diseases. In case of nonadherence to these programs, patients might experience negative complications, such as disease recurrence and disability progress, eventually requiring immediate treatments and hospitalization (10).
The evidence has demonstrated that almost half of individuals with chronic diseases were not successful in adhering to their treatment regimens and showed weak adherence to medications and food restrictions (11). Generally, compliance with treatment in some chronic diseases is within the range of 40 - 60% (12), which is reported as 59% in Iran (13). On the other hand, chronic diseases in developing countries are poorly managed due to a lack of health resources. However, the challenges presented during the pandemic might affect the patients’ adherence to treatment and ruin the health achievements obtained prior to this condition (14).
Adherence to treatment is affected by numerous factors. Many factors influence an individual’s ability and adherence to the treatment regimen, including psychological factors, such as the patient’s inclinations and opinions, difficult social conditions to follow the diet, and financial and care obstacles, such as the way and level of education of patients and their income. In addition, patients with psychiatric problems and cognitive disorders might have numerous problems with following the diet (15, 16). In this study, the two factors of happiness and hope are investigated as well-being and psychological factors in connection with adherence to the treatment regimen.
An increase in age is accompanied by changes in the quality of psychological well-being. Therefore, the feeling of happiness and well-being is among the challenges faced by humans (17). The definition of happiness involves three dimensions, namely satisfaction with life, maximum positive emotions, and minimum negative emotions (18). Generally, happiness is a broad concept, which includes an emotional and a cognitive component. The emotional component refers to enjoying life; nevertheless, the cognitive component involves satisfaction with life (19). Maintaining happiness is one of the most important ways to deal with the anxiety that has increased due to the spread of COVID-19 in the elderly (20, 21); however, the physical and psychosocial factors in old age have undergone changes (22), followed by the decrease in the happiness of the elderly (23).
Making attempts to achieve happiness leads to a positive attitude toward life, positive self-concept, mental health, emotional balance, optimism, desirable attitude toward oneself and others, balanced social relationships, prevention of grudge, prevention of time waste and laziness, an increase of successes in life, higher living indices, better sleep, willingness to help others, and more efficient decision-making (24). Studies have shown relationships between happiness with self-esteem, life expectancy, and quality of life dimensions, such as physical health, psychological health, social relationships, and environment, among older adults (25). Considering the importance and positive outcomes of happiness in the promotion of individuals’ personal and social lives, numerous psychologists have paid attention to the relationship between happiness and other variables (19).
Hope is another variable considered in the present study. Hope is an important compatibility mechanism in patients with chronic diseases, which has been considered a multifaceted and potentially strong factor in effective adjustment (26). According to Benzein and Berg, hope helps patients physiologically and emotionally tolerate the disease crisis; this is, in fact, a factor in predicting the disease process (27). Hope includes individuals’ imaginations and attention to the future and results in making attempts by expecting positive outcomes. Moreover, it has been found to be a multifaceted, dynamic, prospective, and process-oriented concept (28). Hopeful individuals can stand long-term, painful treatments and adhere to treatment regimens more efficiently (29).
Generally, having a clear understanding of psychological well-being factors in patients with chronic diseases is important for planning comprehensive care programs. Additionally, the evidence has indicated that inattention to these factors leading them to be left untreated can result in disability and a decline in the quality of life (30). Attention to these factors is particularly important on the part of healthcare providers, specifically nurses who have close relationships with patients.
Since adherence to treatment regimens depends on numerous factors and is vitally important among older adults with chronic diseases, the identification of all its effective factors, particularly psychological ones, is of utmost importance. However, no studies have been conducted on these three variables in Iran. As mentioned earlier, the studies performed in the field of adherence to treatment regimens have explored other variables. Determining the relationship between psychological well-being factors and adherence to the treatment regimen among the elderly with chronic diseases can help design appropriate interventions and plan for necessary complementary and paraclinical measures.
2. Objectives
Therefore, the present study aimed to evaluate the relationships between happiness and hope with adherence to the treatment regimen among older adults with chronic diseases during the COVID-19 pandemic in 2020.
3. Methods
3.1. Study Design and Setting
This cross-sectional, analytical study was conducted to determine the relationships between happiness and hope with adherence to the treatment regimen among older adults with chronic diseases during the COVID-19 pandemic in April 2020. The study setting included comprehensive health centers, health stations, and geriatric clinics affiliated with Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
3.2. Participants
The research population included all older adults suffering from chronic diseases. The participants were selected from the older adult individuals aged over 55 years who suffered from chronic diseases in Ahvaz. Based on a pilot study performed on 46 individuals indicating r = 0.257 for the correlation between adherence to the treatment regimen and happiness and r = 0.370 for the correlation between adherence to the treatment regimen and hope, considering α = 0.05 and β = 0.1, and using the following formula, the sample size was estimated at 160 and 90 subjects, respectively. With the consideration of the larger sample size (n = 160) and 10% attrition, 200 individuals were recruited (31).
The study participants were selected via convenience sampling. Considering the COVID-19 pandemic and the associated restrictions, after obtaining the necessary permissions, the researcher took the older adults’ phone numbers from the health centers. Through phone contact, the researcher introduced him/herself and assessed the individuals’ conformity to the inclusion and exclusion criteria. The inclusion criteria of the study were the age of 60 years and over, suffering from at least one chronic disease (e.g., cancer, diabetes, hypertension, heart failure, and stroke), awareness of the treatment process, willingness to participate in the research, and understanding of Persian. The exclusion criteria of the study were unwillingness to cooperate, uncompleted study questionnaires, and a history of mental disorders resulting in mood changes and depression with a medical history and reading the patient’s treatment record. Then, the study objectives were explained to the participants, and their oral consent was obtained. Afterward, the study questionnaires were sent to them or their children via WhatsApp. The participants were required to complete the questionnaires and send them back to the researcher. In case of illiteracy, the researcher read the items to the participants through phone contact and completed the questionnaires. It is worth mentioning that the participants determined the time of phone calls. Moreover, the participants were assured that they could withdraw from the study at any stage, which would not have any negative impact on their care process.
The study data were collected using a demographic information form, Morisky Medication Adherence Scale (MMAS), Oxford Happiness Questionnaire, and Herth Hope Index. The demographic information form included the age, gender, occupation, educational level, marital status, and employment status of the participants and their spouses.
3.3. Measurements
The MMAS was developed by Krousel-Wood et al. in 2009 (32). This scale contained eight items, seven of which had a yes/no format. In these items, scores 0 and 1 were allocated to “yes” and “no” answers, respectively. The last item was responded to via a Likert scale with the options of never, rarely, often, and always. It should be noted that items five and eight were scored reversely. The total score of the questionnaire was computed by summing up the scores of all the items and could range from 0 to 8. Accordingly, scores < 6, 6 - 8, and 8 represented weak, moderate, and good adherence levels, respectively. In a study carried out by Kooshyar et al. the face and content validity of the questionnaire was approved by experts, and its reliability was confirmed by Cronbach’s alpha equal to 0.68 (16). Moharamzadeh et al. also assessed the psychometric properties of the Persian version of this questionnaire among Iranian hypertensive patients in 2015 and reported its Cronbach’s alpha coefficient as 0.697 (33).
Oxford Happiness Questionnaire was developed by Argyle and Lu in 2002 to evaluate happiness. This questionnaire consisted of 29 multiple-choice items scored from 0 to 3. Therefore, the total score of the questionnaire could range from 0 to 87. The participants were required to read the items and choose the answers that best described their recent feelings (34). The factor analysis performed for this questionnaire revealed seven factors, namely positive cognition, social commitment, positive affect, sense of control, physical fitness, satisfaction with self, and mental alertness (35). For the assessment of the reliability and validity of the original version of the questionnaire, 172 Oxford University students and their companions were requested to fill out the questionnaire through self-report, and Cronbach’s alpha coefficient of 0.91 was obtained (36). In Iran, Alipoor and Noorbala (37) reported the internal consistency of the questionnaire to be 3.91 and 3.93 among male and female subjects, respectively. Additionally, a high correlation was observed between the 29 items of the questionnaire and its total score. Moreover, Cronbach’s alpha coefficient of the questionnaire was 0.93, and its split-half reliability was 0.92. Furthermore, factor analysis resulted in the extraction of five factors, which explained 57.1% of the total variance (38).
Hope was evaluated using the Herth Hope Index. This scale included 12 statements, which could be scored via a four-option Likert scale ranging from 1 (completely disagree) to 4 (completely agree). It should be noted that items three and six were scored reversely. The reliability of this index was approved by studies performed by Herth and Benzein and Berg (26, 27). In Iran, a study performed by Baljani et al. in 2011 confirmed the content validity of the Herth Hope Index and approved its reliability by Cronbach’s alpha coefficient equal to 0.82. The total score of this index could range from 12 to 48, with higher scores representing a better hope status (39).
3.4. Statistical Analysis
After all, the study data were entered into SPSS software (version 24) and were analyzed using descriptive statistics, dispersion indices, and regression. Independent sample t-test and analysis of variance for normal variables and Mann-Whitney test and Kruskal-Wallis test for nonnormal variables were carried out to determine the relationship between demographic variables, hope, happiness, and adherence to the treatment regimen. Finally, linear regression was applied to determine the relationships between variables.
3.5. Ethical Considerations
The present study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1399.116). All necessary permissions for conducting the research were obtained from the relevant administrators, and all methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from the participants in the study.
4. Results
Totally, 220 questionnaires were distributed among the older adults with chronic diseases who were eligible to participate in the research. However, 216 questionnaires were completed, indicating a response rate of 98.66%. The mean age of the participants was 64.70 ± 10.56 years. Additionally, 62% and 38% of the participants were male and female, respectively. Moreover, 179 participants (82.9%) had under diploma degrees. Table 1 shows other demographic data.
| Variables | No. (%) | Adherence to the Treatment Regimen | Hope | Happiness |
|---|---|---|---|---|
| Age (y) | ||||
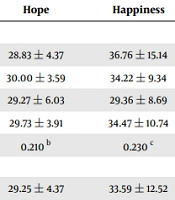
| 55 - 60 | 42 (19.4) | 7.59 ± 2.03 | 28.83 ± 4.37 | 36.76 ± 15.14 |
| 61 - 80 | 163 (75.5) | 7.72 ± 1.63 | 30.00 ± 3.59 | 34.22 ± 9.34 |
| 81 - 90 | 11 (5.1) | 6.81 ± 1.66 | 29.27 ± 6.03 | 29.36 ± 8.69 |
| Total | 216 (100) | 7.65 ± 1.72 | 29.73 ± 3.91 | 34.47 ± 10.74 |
| P-value | - | 0.234 b | 0.210 b | 0.230 c |
| Gender | ||||
| Female | 82 (38) | 7.70 ± 1.94 | 29.25 ± 4.37 | 33.59 ± 12.52 |
| Male | 134 (62) | 7.61 ± 1.57 | 30.02 ± 3.58 | 35.00 ± 9.50 |
| Total | 216 (100) | 7.65 ± 1.72 | 29.73 ± 3.91 | 34.47 ± 10.74 |
| P-value | - | 0.061 d | 0.070 d | 0.068 d |
| Chronic disease | ||||
| Several chronic diseases | 109 (50.5) | 7.72 ± 1.70 | 29.40 ± 4.22 | 34.20 ± 11.61 |
| Diabetes | 39 (18.1) | 8.00 ± 1.43 | 30.41 ± 2.57 | 34.92 ± 7.60 |
| Hypertension | 36 (16.7) | 6.69 ± 1.84 | 29.69 ± 4.93 | 35.55 ± 12.57 |
| Heart diseases | 23 (10.6) | 8.43 ± 1.34 | 29.95 ± 2.67 | 34.13 ± 10.08 |
| Kidney diseases | 7 (3.2) | 7.14 ± 1.86 | 30.14 ± 3.07 | 31.42 ± 5.44 |
| Pulmonary diseases | 2 (0.9) | 7.00 ± 1.41 | 31.50 ± 2.12 | 35.50 ± 0.70 |
| Total | 216 (100) | 7.65 ± 1.72 | 29.73 ± 3.91 | 34.47 ± 10.74 |
| P-value | - | 0.005 e | 0.890 e | 0.909 e |
| Marital status | ||||
| Single | 4 (1.9) | 9.50 ± 1.73 | 27.25 ± 6.23 | 44.75 ± 10.40 |
| Married | 117 (54.2) | 7.74 ± 1.65 | 29.67 ± 4.28 | 37.09 ± 10.76 |
| Divorced | 7 (3.2) | 8.14 ± 1.06 | 30.28 ± 2.56 | 25.85 ± 8.59 |
| Widow | 88 (40.7) | 7.40 ± 1.80 | 29.88 ± 3.34 | 31.20 ± 9.55 |
| Total | 216 (100) | 7.65 ± 1.72 | 29.73 ± 3.91 | 34.47 ± 10.74 |
| P-value | - | 0.061 c | 0.882 c | 0.000 c |
| Educational status | ||||
| High school | 179 (82.9) | 7.69 ± 1.61 | 30.14 ± 3.25 | 32.65 ± 8.88 |
| Diploma | 27 (12.5) | 7.74 ± 1.81 | 27.55 ± 6.11 | 45.48 ± 12.91 |
| Associate degree | 1 (0.5) | - | - | - |
| Bachelor’s degree | 6 (2.8) | 7.00 ± 2.44 | 29.33 ± 5.57 | 33.33 ± 18.56 |
| Master’s degree and higher | 3 (1.4) | 5.66 ± 4.61 | 27.00 ± 6.55 | 46.33 ± 15.04 |
| Total | 216 (100) | 7.65 ± 1.72 | 29.73 ± 3.91 | 34.47 ± 10.74 |
| P-value | - | 0.282 b | 0.269 c | 0.000 c |
| Do you have a job? | ||||
| Yes | 22 (10.2) | 7.31 ± 2.14 | 28.18 ± 4.63 | 38.31 ± 15.18 |
| No | 194 (89.8) | 7.69 ± 1.66 | 29.91 ± 3.79 | 34.03 ± 10.08 |
| Total | 216 (100) | 7.65 ± 1.72 | 29.73 ± 3.91 | 34.47 ± 10.74 |
| P-value | - | 0.311 d | 0.314 d | 0.085 b |
| Do you have health insurance? | ||||
| Yes | 196 (90.7) | 7.65 ± 1.73 | 29.77 ± 3.89 | 34.57 ± 10.75 |
| No | 20 (20.3) | 7.60 ± 1.60 | 29.35 ± 4.20 | 33.50 ± 10.91 |
| Total | 216 (100) | 7.65 ± 1.72 | 29.73 ± 3.91 | 34.47 ± 10.74 |
| P-value | - | 0.755 b | 0.780 b | 0.595 b |
Correlation Between Demographic and Social Characteristics with Hope, Happiness, and Adherence to Treatment Regimen a
The mean score of adherence to the treatment regimen was 7.65 ± 1.72 (range: 3 - 11). Based on the results, weak, moderate, and good adherence to treatment was observed among 23 (10.6%), 65 (30.1%), and 128 (59.3%) participants, respectively (Table 2). The results revealed no significant relationship between the mean score of adherence to treatment and demographic features (Table 1). The mean score of adherence to treatment was significantly associated with the type of chronic disease (P = 0.005; Table 1).
| Variables and Score Range | No. (%) |
|---|---|
| Adherence to the treatment regimen | |
| Weak (0 - 5) | 33 (10.6) |
| Medium (6 - 7) | 65 (30.1) |
| Good (8) | 125 (59.3) |
| Hope | |
| Weak (12 - 23) | 13 (6) |
| Medium (24 - 36) | 203 (94) |
| Good (37 - 48) | - |
| Happiness | |
| Weak (0 - 28) | 42 (19.4) |
| Medium (29 - 57) | 163 (75.5) |
| Good (58 - 87) | 11 (5.1) |
Frequency of Adherence to Treatment Regimen, Hope, and Happiness in Older Adults with Chronic Diseases
The mean score of hope was 29.73 ± 3.91 (range: 12 - 36). According to the findings, 13 (6%) and 203 (94%) participants were weakly and moderately hopeful, respectively (Table 2). The results showed no significant relationship between the mean score of hope and demographic variables (Table 1).
The mean score of happiness was 34.47 ± 10.74 (range: 10 - 79). Low, moderate, and high happiness levels were observed among 42 (19.4%), 163 (75.5%), and 11 (5.1%) participants, respectively (Table 2). The mean score of happiness was significantly associated with marital status (P = 0.000) and educational level (P = 0.000; Table 1).
The study results indicated no significant relationship between the mean scores of hope and adherence to the treatment regimen (r = 0.040, P = 0.557). However, the mean score of happiness was significantly associated with the mean score of adherence to the treatment regimen (r = 0.210, P = 0.002). Accordingly, higher happiness levels were accompanied by a higher adherence to the treatment regimen. Table 3 shows the results of multivariate analyses for investigating the relationship between hope and happiness and the mean score of adherence to the treatment regimen. Based on the regression coefficients, no significant relationship was observed between the mean score of hope and adherence to the treatment regimen (b = 0.037, P = 0.222). However, the mean score of happiness was significantly correlated with the mean score of adherence to treatment (b = 0.036, P = 0.001). Considering P = 0.004 and F = 5.674, the fitted regression model was significant. In addition, R2 was equal to 0.051, which indicated that 5.1% of the changes in the mean score of adherence to treatment were determined by the mean scores of hope and happiness (Table 3).
| Model | B | SE | Beta | t | P |
|---|---|---|---|---|---|
| Constant | 5.319 | 1.036 | - | 5.135 | 0.000 |
| Hope | 0.037 | 0.030 | 0.083 | 1.225 | 0.222 |
| Happiness | 0.036 | 0.011 | 0.225 | 3.314 | 0.001 |
| Total score | R = 0.225, R2 = 0.051, R2 adjusted = 0.042, Sig = 0.004, F = 5.67 | ||||
Results of Linear Regression Analysis Between the Total Score of Adherence to Treatment Regimen with the Variables of Hope and Happiness
5. Discussion
This study aimed to determine the relationships between happiness and hope with adherence to the treatment regimen among older adults with chronic diseases. In the present study, the participants showed a moderate level of hope, which is in line with the results of studies performed by Balsanelli et al. (40) but not with a study conducted by Dehbashi et al. on dialysis patients (41). Higher hope levels among patients with chronic diseases might be attributed to the advances in the care services provided for these patients, including faster diagnosis, increased care levels, and support for disease management (42). On the other hand, hope is a positive force that enhances motivation, advancement of goals, and compatibility among patients (43). Bluvol and Ford-Gilboe conducted a study on stroke patients and disclosed that hopeful thinking helped individuals feel that they could control their lives. Therefore, they attributed positive values to their lives and lived more hopefully (44).
In the current study, the participants had a moderate level of happiness, which is consistent with the findings of a study performed by Abdollahi et al. on hypertensive patients (45). The results of a study by Petroviˇc et al., who compared happiness levels before and after COVID-19, showed that individuals’ happiness levels did not change significantly at the end of the study. They further explain that loneliness during the pandemic period helps individuals to turn this complicated process into an opportunity by organizing various activities within their homes (46). On the other hand, the results of some studies show that the pandemic period has had a negative impact on the level of happiness of individuals, especially older individuals, and their anxiety, tension, fatigue, depression, and stress have increased due to the decrease in happiness (47-49).
Global surveys conducted before COVID-19 indicate that women typically experience marginally greater happiness than men (50). The aforementioned data suggest that the null result that was observed might be indicative of a decrease in women’s happiness during COVID-19 (51). Greyling et al. stated that during the outbreak of COVID-19 and the resulting quarantine, individuals’ happiness levels decreased; however, surprisingly, over time, there appears to be a U-shaped relationship between the number of COVID-19 cases and happiness; that is, at first, the research results show a decrease in the happiness. Nevertheless, due to the nature of COVID-19, its high recovery rate, and low mortality, it seems that the level of happiness has increased. However, the effect size is very small; therefore, this increase is negligible (52). Since happiness is associated with individuals’ cognitive evaluation of their satisfaction with life, family, job, and experiences of relationships with others, it can represent their mental health (53).
The participants in the present study showed good adherence to treatment regimens. In a study, Zahetkashan et al. reported that patients with coronary artery disease coped with the threats and challenges caused by the COVID-19 pandemic by targeting their self-care behaviors and tried to adhere to treatments more effectively (54). The data from Khabbazi et al.’s study showed that medication nonadherence was not common within 6 months after the issue of COVID-19 was widely discussed in the media (55). In agreement with the results of the current study, Schmeiser et al. reported 90% adherence in the patients receiving antirheumatic medications (56). Fragoulis et al. reported nonadherence to medications in 14.6% of patients with rheumatic diseases in Greece (57). However, contradictory results were obtained by Pazokian et al. (58) in patients with diabetes and by Kavak and Yilmaz (59) in patients with schizophrenia. Nouira et al. showed that medication nonadherence was reported in 39% of patients in Tunisia, and the predictors of therapeutic nonadherence were polypharmacy, rural origin, and metabolic disease history (60). Several studies presented that with the continuation of quarantines, social distancing, and economic problems during the COVID-19 pandemic, nonadherence to treatment, especially in older adults, is likely to worsen (60). However, about 40% of the older adults in this study had moderate to poor adherence to treatment. The rate of adherence to treatment in this study was about 10%. In another study, it was found that 4 - 31% of diabetic patients never tried to prepare their prescribed medicines and some others refused to take medicines after preparing them (61).
In numerous studies, the prevalence of noncompliance with treatment has been reported within the range of 18 - 71%. This result can be a reason for the hospitalization of 10% of older adults in hospitals and 32% in nursing homes (61, 62). In another study, it was reported that the adherence to treatment of type 2 diabetes patients in the south of Tehran, Iran, was poor (63). In general, adherence to treatment can be affected by various factors, such as prescribed medications and mental, economic, and social factors. Therefore, understanding the psychosocial parameters affecting adherence to treatment among patients with chronic diseases and supporting them in those areas can be effective in their adherence to treatment regimens (64). During the COVID-19 pandemic, the emergency services in Iran played an important role in the follow-up and therapeutic continuity of these elderly patients. Among the reasons for the difference in the results of the studies, it can be pointed to different demographic characteristics of patients in different studies, different levels of development and health literacy in the communities, and different tools used to check the level of treatment compliance of patients.
The present study findings showed no significant relationship between hope and adherence to the treatment regimen. Consistently, Alipour et al. emphasized that hope could not be a suitable mediator for adherence to the treatment regimen among patients with diabetes (38). Habte et al. also showed the negative impact of hope on adherence to the treatment regimen. In other words, they regarded hope as an obstacle to the acceptance of antidiabetic drugs among some participants (65). In contrast, Kavak and Yilmaz revealed a significant relationship between hope and adherence to treatment (59). A study by Javanmardifard et al. showed that a significant reverse correlation was also observed between hope and adherence to treatment (42). Overall, adherence to the treatment regimen might be affected by factors, such as attitude toward the disease, hope for the treatment of the disease, mildness of the disease, disease complications, easy application of the regimen, and its cost-effectiveness (65). Considering the discrepancy among the results, further studies in this field are warranted.
The results of the present investigation revealed a significant relationship between happiness and adherence to the treatment regimen, which is in line with the findings of a study carried out by Cuffee et al. on patients suffering from hypertension. They mentioned that the patients with higher happiness levels showed better adherence to their treatment regimen (66). The evidence has indicated that nonpathological emotional states, such as happiness, can result in psychological well-being, thereby exerting a profound effect on the incidence of health-related behaviors (67). Since adherence to the treatment regimen is a health-related behavior, it can be positively affected by happiness. However, McDonald et al. stated that short-term interventions for the empowerment of patients’ happiness were not effective in the promotion of their adherence to treatment (68), which is contrary to the findings of the current study. Therefore, long-term interventions for strengthening happiness, including the empowerment of interpersonal relationships, improvement of relationships between patients and their family members, and establishment of appropriate relationships between patients and society, have to be implemented among patients with chronic diseases in order to achieve the effect of happiness on adherence to treatment (69).
Based on the results, adherence to treatment regimen and hope were not associated with demographic variables, which is consistent with the results of several studies conducted on the issue (70). However, some studies have shown significant relationships between the aforementioned two variables and demographic features (42). It seems that the relationship between the aforementioned variables and demographic characteristics depends on the type of the disease rather than the effect of the disease on patients and their quality of life.
The current study’s findings revealed a significant relationship between happiness and marital status. Similarly, Cheah and Tang reported significant relationships between happiness and some demographic features, such as marital status (71). Generally, care and supportive relationships are vitally important among patients suffering from chronic diseases. Such support can be provided by family members, particularly the spouse, and can help individuals identify their capabilities and resources and succeed in coping with the disease (72). Therefore, it can be concluded that during disease conditions, specifically chronic diseases, the presence of the spouse can be effective in increasing the elderly patient’s happiness level.
The findings of the current study also revealed a significant relationship between happiness and educational level, which is in agreement with the results obtained by Saffari et al. (73). Delavar and Shokouhi Amirabadi showed there was a significant relationship between happiness and educational level of students during the COVID-19 period (74). Education can play a pivotal role in choosing appropriate coping methods for reducing stress, improving psychological well-being, and solving problems associated with diseases. Therefore, higher educational levels can affect the selection of proper coping strategies against chronic diseases, eventually helping patients maintain their happiness as a component of psychological well-being.
5.1. Limitations
Considering the desirable cooperation on the part of the participants, the study suffered from no particular limitations. Nonetheless, due to the restrictions associated with the spread of the coronavirus, having access to older adult individuals was quite difficult and affected the study sample size. The completion of the study questionnaires electronically was also accompanied by several problems.
5.2. Conclusions
The participants in the current study had moderate levels of hope and happiness and showed good adherence to their treatment regimens. The results revealed no significant relationship between hope and adherence to the treatment regimen. However, a significant relationship was observed between happiness and adherence to the treatment regimen. Therefore, happiness as a psychological variable affecting psychological well-being can be effective in adherence to treatment among patients with chronic diseases. In this context, designing interventions for increasing happiness among these patients can affect their health-related behaviors, such as adherence to treatment, eventually improving their disease process and enhancing their quality of life. Therefore, measures should be taken to familiarize nursing students and healthcare personnel with these interventions in order to promote patients’ happiness levels. On the other hand, policymakers are recommended to develop programs to increase happiness among older adults who mostly suffer from chronic diseases. Based on the present study’s findings, increasing the happiness level can enhance adherence to the treatment regimen as a health-related behavior.