1. Background
As a common condition, low back pain (LBP) is the leading cause of disability in the world (1, 2). Approximately 50 - 80% of individuals experience LBP at least once in their lifetime (3). The overall prevalence of LBP is 28.8%, with men and women accounting for 39% and 60.9%, respectively (4). The rate of LBP in Iran is estimated to be 25.2% (5). Although most individuals with LBP recover quickly within a few weeks or months, about one in three individuals develop chronic LBP, which lasts for 3 or more months (6-8). Most chronic LBP cases have unknown pathoanatomical causes, which are called chronic nonspecific LBP. Therefore, treatment is focused on relieving symptoms, such as pain (9, 10).
The LBP imposes high economic costs on communities. The annual cost of LBP healthcare in the United States is estimated to be $100 billion (11). Psychosocial factors play an important role in chronic LBP (12). Studies have also shown that depression, a psychological factor, is consistently associated with LBP in the adult population (13). A review of the literature indicated that depression was present in 85% of individuals who reported painful conditions (7).
Patients with LBP and depression incurred higher direct costs of healthcare than patients who did not have depression. Therefore, it is important to manage depressive symptoms in patients with LBP (2). Pharmacological therapies, including nonsteroidal anti-inflammatory medications, muscle relaxants, narcotics, and antidepressants, are used to treat LBP (3), which are associated with side effects (14). For example, analgesics might drop blood pressure, impair vital functions, and cause drowsiness, nausea, vomiting, and even shock (3, 8). Therefore, nonpharmacological therapies, including complementary and alternative medicine, should be used to relieve LBP and depressive symptoms.
As one of the most common types of complementary and alternative medicine, acupuncture is the insertion of very thin needles through your skin and has different subgroups, one of which is acupressure (15, 16). Typically, in acupressure, physical pressure with the thumb is applied on specific acupoints (14). Acupressure is a noninvasive, low-cost, and effective alternative to pain relief (17). Acupressure might increase the production of endogenous sedatives and analgesics by stimulating the autonomic nervous system, thereby relieving pain (11).
Numerous studies have addressed the effect of acupressure on LBP. Cheng et al. showed that acupressure could reduce postpartum LBP intensity (18). Ali Awad and Hawash also reported that applying pressure on specific acupoints reduced LBP among nurses (19). A meta-analysis on the efficacy and safety of acupressure in LBP conducted by Li et al. showed that although acupressure had promising effects on reducing LBP intensity, high-quality evidence was not adequate to make an informed decision (11).
Considering depression, some previous studies have shown the effectiveness of acupressure in improving depression in patients with osteoarthritis and patients receiving hemodialysis (20, 21). Nevertheless, there are also contradictory findings on the effect of complementary medicine on depression. For example, de Lorent et al. found that acupuncture was not effective in reducing depression and anxiety among patients with major anxiety (22). Generally speaking, previous research has revealed a bi-directional association between depressive symptoms and bodily pain (23).
2. Objectives
In spite of the importance of this association, empirical studies investigating the simultaneous efficiency of acupressure in back pain and depression among chronic nonspecific LBP patients are very scarce. Therefore, this study aimed to investigate the effect of acupressure on LBP and depression among chronic nonspecific LBP patients.
3. Methods
3.1. Study Design and Participants
In this sham-controlled randomized clinical trial (code no.: IRCT20200812048386N1, accessible at: https://fa.irct.ir/trial/59132), the study population included all patients diagnosed with chronic LBP referred to the neurology clinic of Razi hospital affiliated to Birjand University of Medical Sciences (BUMS), Birjand, Iran.
The inclusion criteria were patients who provided informed written consent to participate in the study, had nonspecific LBP for more than 12 weeks, with no wounds, infections, or fractures at acupoints or sham points, aged over 18 years, were not pregnant, did not use other types of complementary medicine concomitantly (e.g., massage therapy), with no malignancy or autoimmune diseases, not having an addiction to sedatives and alcohol, and not having mental disorders. The exclusion criteria included unwillingness to continue to participate in the study and the use of analgesics due to acute pain.
According to a previous study (24), with test power of 90% (β = 0.1), error coefficient of α = 0.05, parameters S1 = 1.01, S2 = 0.86, mL = 2.97, and m2 = 2.11, as well as an attrition rate of 10 %, the sample size was estimated at 92 subjects (46 per group).
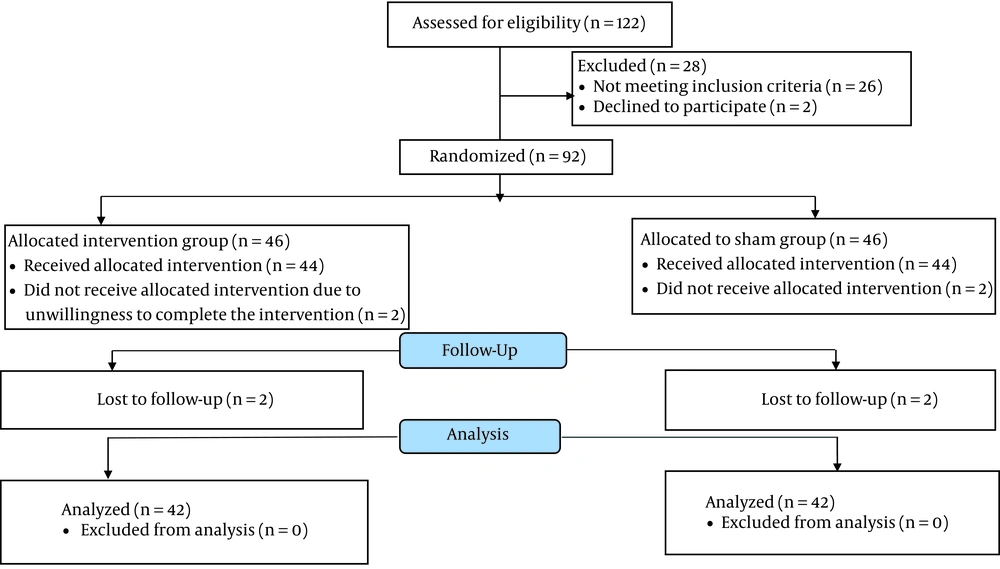
A total of 92 eligible participants were selected using the convenience sampling method. A demographic characteristics questionnaire, the Visual Analogue Scale (VAS), and the Beck Depression Inventory-II (BDI-II) were completed. These individuals were then randomly assigned to acupressure (n = 46) and sham (n = 46) groups using block randomization with a block size of 4 and a randomization ratio of 1:1 (Figure 1). In this single-blind, sham-controlled randomized clinical trial, the patients were blind to the allocation.
3.2. Intervention
A traditional Chinese medicine practitioner trained and granted a certificate to the first researcher. The researcher had to ensure that patients could locate the acupoints. He instructed them to stimulate the trigger points with their thumbs to create a feeling of warmth, heaviness, and numbness regarding the patient’s pain threshold. The intervention group had pressure on Feng chi (GB20), Shufu (KID-27), and Yintang (EX-HN-3) acupoints daily for 4 weeks; nevertheless, the sham group had pressure on Huangshu (KI16), Jiache (ST6), and Chengjiang (CV24) acupoints daily for 4 weeks. The patients applied the pressure on each specified acupoint for 5 minutes, for a total of 15 minutes once a day for 4 weeks (25, 26). A printed pamphlet containing information about how to locate and press the acupoints/sham acupoints was handed to the participants. The patients were required to complete the intervention before going to bed. Furthermore, Auto Reminder SMS was used to remind them of the intervention. Finally, the patients were asked to complete a checklist to ensure that they had pressure on acupoints timely.
3.3. Data Collection Tools
3.3.1. Demographic Information Questionnaire
This questionnaire includes age, gender, marital status, education level, smoking history, duration passed since LBP had been diagnosed, the mean number of analgesics used per week, and body mass index (BMI).
3.3.2. Visual Analogue Scale
The VAS is a straight line of fixed length (usually 100 mm). Patients make a handwritten mark on this line that represents a continuum between “no pain” on the left end (0 cm) and “worst pain” on the right end of this scale (10 cm). The VAS has been widely used in pain research. Its validity and reliability have been satisfactory in studies related to LBP (27).
3.3.3. Beck Depression Inventory-II
The Persian version of the BDI-II was used to assess depression (28). This 21-item questionnaire assesses the severity of depression. Participants respond to each item on a four-point Likert scale (from 0 to 3), with higher scores indicating more severe depression. The validity and reliability of this inventory were 0.72 and 0.83, respectively (29). In the present study, Cronbach’s alpha for this instrument was 0.77.
3.4. Ethical Considerations
The Ethics Committee of BUMS approved the proposal of the current study (approval no.: IR.BUMS.REC.1398.384, accessible at: https://ethics.research.ac.ir). All the participants were assured that their participation would be voluntary, their information would remain confidential, and they could withdraw from the research without penalty.
3.5. Data Analysis
SPSS software (version 24) was used for data analysis. Descriptive statistics, including mean, standard deviation, and frequency, were applied to describe the patients’ demographics. Due to abnormal data distribution, the Mann-Whitney U and Wilcoxon tests were used to compare depression and LBP within and between the groups. Analysis of covariance (ANCOVA) was applied to investigate whether there was a difference between the two groups in terms of the mean scores of depression and back pain intensity after the intervention by controlling the baseline scores of these two variables. The significance level was considered less than 0.05.
4. Results
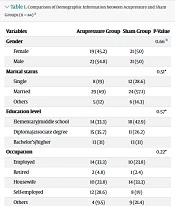
Of 92 participants, 8 patients (4 participants from each group) withdrew from the trial. Therefore, 84 participants in the acupressure (n = 42) and sham (n = 42) groups were examined (Figure 1). The mean age values of the acupressure and sham groups were 39.05 ± 8.66 and 40.60 ± 7.72 years (P = 0.39), respectively. The BMI mean values were 25.93 ± 2.47 and 26.02 ± 1.86 kg/m2 for acupressure and sham groups (P = 0.91), respectively. The mean values of the average duration of LBP in the acupressure and sham groups were19.00 ± 6.31 and 15.12 ± 7.77 months, respectively (P = 0.17). Table 1 shows the comparison of other demographic characteristics.
Regarding the mean scores of LBP and depression, a significant difference was not observed between the acupressure and sham groups at the baseline (P > 0.05); however, the mean scores of LBP and depression in the acupressure group were significantly lower than the sham group after the intervention (P < 0.05). Moreover, the mean LBP and depression scores in both groups were significantly lower after the intervention than before the intervention (P < 0.05; Table 2). For the patients of the acupressure group, the back pain severity and depression significantly improved from the pretest to the posttest when compared to the measurements of the sham group (P < 0.001; Table 3).
Finally, ANCOVA was employed to evaluate the effect of acupressure on LBP and depression while controlling the baseline scores of these two variables in both groups. The ANCOVA results showed significant differences in these two variables between the two groups of acupressure and sham after the intervention. Depression and LBP significantly improved in the acupressure group (P < 0.05; Table 4).
5. Discussion
The current study aimed to evaluate the effect of acupressure on LBP and depression among chronic nonspecific LBP patients. In this study, applying pressure on Feng chi, Shufu, and Yintang acupoints reduced patients’ LBP severity. Murphy et al. showed a positive improvement in LBP in the self-acupressure group than in the routine care group (14). Additionally, Cheng et al. examined the effect of acupressure on postpartum LBP. They found that the mean VAS score in the acupressure group was significantly lower than in the control group (18). Ali Awad and Hawash also reported that acupressure was successful in reducing LBP in nurses (19). Movahedi et al. argued that acupressure reduced the severity of LBP in female nurses 2 and 4 weeks after the intervention (24). Different acupoints and different lengths of intervention were the key differences between the current study and the four studies mentioned above.
Nevertheless, the results of some studies are in contrast with the findings of the current study. Mu et al. performed a meta-analysis aimed at determining the effects of acupuncture on chronic nonspecific LBP. They found that acupuncture might not have a more clinically significant efficacy than the sham in reducing pain immediately after the intervention (30).
Ernst believed that acupressure might stimulate A-delta fibers in the skin, which reach the gray area of the brain, probably inhibiting pain stimulation, thereby reducing the perception of pain. In addition, acupressure might activate enkephalins in brain neurons and inhibit pain transmission to the brain. Finally, acupressure releases endorphins and meta-enkephalin in the brain and activates the pain relief system in the midbrain (31).
According to the current study, by controlling the baseline scores of depression in both groups, the mean score of depression in the acupressure group was significantly lower than in the control group after the intervention. Consistent with this finding, some previous studies have shown the effectiveness of acupressure in improving postpartum depression (18), depression in patients with osteoarthritis (20), depression in hemodialysis patients (24), and depression in older adults (32). It should be noted that the acupressure points and the duration of intervention in the aforementioned studies are different from those of the present study. However, there are some contradictory results in this regard. Lan et al. indicated that acupressure did not reduce the depressive symptoms of patients with liver cancer (33). De Lorent et al. showed that acupuncture did not affect depression and anxiety in patients with anxiety and major depression disorders (22). According to the results, acupressure does not have the same effect on depression in patients with different medical conditions.
In general, researchers believe that massage stimulates acupoints and improves energy meridians of the body, which causes a proper response in various body organs and glands. Acupressure causes the secretion of neurotransmitters, adrenergic hormones, and the mediating mechanism of endorphins, thereby reducing the symptoms of depression (21).
In the present study, depression and LBP in the sham group were significantly reduced due to the placebo effects of the acupressure used for the sham group. De Lorent et al. studied the effectiveness of acupressure in managing depression in older adults, the results of which are similar to the results of the present study. Depression was reduced in the sham group in both studies (22). Kaptchuk acknowledged that sham acupuncture increased placebo responses. According to Kaptchuk, further studies are needed in this regard (34).
One of the limitations of the present study was that the participants were selected from only one neurology clinic. Further studies can help strengthen the study by including multisite participants. In the current study, the outcomes were also measured only immediately after the intervention sessions and not over a longer term. The long-lasting effects of acupressure with different protocols can be evaluated in future randomized trials.
5.1. Conclusions
Self-acupressure on Shu Fu, Yin Tang, and Feng Chi points can reduce LBP and depression among patients with chronic nonspecific LBP. The findings of this study can be used in designing and evaluating more robust protocols. Moreover, the replication of this study with a larger sample size would allow better generalizations.
| Variables | Acupressure Group | Sham Group | P-Value |
|---|---|---|---|
| Gender | 0.66 b | ||
| Female | 19 (45.2) | 21 (50) | |
| Male | 23 (54.8) | 21 (50) | |
| Marital status | 0.51* | ||
| Single | 8 (19) | 12 (28.6) | |
| Married | 29 (69) | 24 (57.1) | |
| Others | 5 (12) | 6 (14.3) | |
| Education level | 0.57* | ||
| Elementary/middle school | 14 (33.3) | 18 (42.9) | |
| Diploma/associate degree | 15 (35.7) | 11 (26.2) | |
| Bachelor’s/higher | 13 (31) | 13 (31) | |
| Occupation | 0.22* | ||
| Employed | 14 (33.3) | 10 (23.8) | |
| Retired | 2 (4.8) | 1 (2.4) | |
| Housewife | 10 (23.8) | 14 (33.3) | |
| Self-employed | 12 (28.6) | 8 (19) | |
| Others | 4 (9.5) | 9 (21.4) | |
| History of smoking | 0.50* | ||
| No | 14 (33.3) | 17 (40.5) | |
| Yes | 28 (66.7) | 25 (59.5) | |
| Mean use of analgesics per week | 0.27* | ||
| None | 19 (45.2) | 14 (33.3) | |
| Once | 11 (26.2) | 18 (42.9) | |
| Twice or more times | 12 (28.6) | 10 (23.8) |
a Values are expressed as No. (%).
b The results of the chi-square test.
| Variables/Time | Acupressure Group | Sham Group | P-Value |
|---|---|---|---|
| LBP | |||
| Pretest | 62.61 ± 8.28 | 61.66 ± 9.08 | 0.45* |
| Posttest | 38.33 ± 7.29 | 58.80 ± 10.40 | < 0.001* |
| P-value | < 0.001** | 0.04** | |
| Depression | |||
| Pretest | 22.64 ± 5.54 | 23.79 ± 2.54 | 0.26* |
| Posttest | 14.29 ± 3.61 | 20.26 ± 2.46 | < 0.001* |
| P-value | < 0.001** | < 0.001** | < 0.001 |
a * The results of the Mann-Whitney U test; ** The results of the Wilcoxon test.
a The results of the Mann-Whitney U test
| Variables | Acupressure Group, Mean ± SE | Sham Group, Mean ± SE | F | P-Value a |
|---|---|---|---|---|
| Back pain | 38.07 ± 1.18 | 59.06 ± 1.18 | 155.89 | < 0.001 |
| Depression | 14.57 ± 0.33 | 19.97 ± 0.34 | 125.30 | < 0.001 |
Abbreviation: SE, standard error.
a The results of analysis of covariance.