1. Background
Attention deficit hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders in early childhood. The global prevalence is 2.7 - 5.29%, which has been increasing in recent years (1). Also, ADHD is frequently linked to academic underachievement, social difficulties, and mental health issues. Moreover, ADHD has a remarkable impact on children, their families, schools, and communities because of its long-term emotional burden and interference with work. Children with ADHD are more at risk of negative results in their childhood and adulthood due to the potential for ADHD side effects to decline over time (2). Adults with ADHD are more likely to have comorbidities with drug or alcohol use, medical condition, and functional impairment (3). Children with ADHD often suffer from other comorbidities, such as oppositional defiant disorder, conduct disorder, depression, anxiety, and Tourette syndrome (4).
According to Barkley's paradigm (Barkley, 2014), people with ADHD have problems restraining themselves in emotionally charged circumstances, which makes them more prone to emotional reactivity than people without ADHD (5). Children and adolescents with ADHD (aged 6 to 15) are considerably more emotionally reactive than participants of the control group to immediate and future challenges that are both positively and negatively emotionally charged (6). While externalizing behaviors signify aggressive and delinquent issues, internalizing behaviors reveal a child's mental state, including depressive disorders, anxiety problems, or somatic symptoms. Children with ADHD, aged 6 - 15, display impressively higher internalizing and externalizing behavior scores than non-ADHD controls, according to parent reports from both community-based and clinical settings (7). Children with internalizing and externalizing behavior disorders and ADHD are more likely to experience health-related problems (8). Compared to children with ADHD alone, children with comorbid externalizing behavior disorders show worse social skills (9).
When someone's mind becomes preoccupied with internal, unrelated thoughts and images instead of focusing on their main work, it is known as mind wandering (MW). Mind wandering is a prevalent experience that constitutes up to 50% of our daily thinking time (10). Two types of MW - deliberate and spontaneous - are believed to reflect different balancing mechanisms between internal self-regulating thought systems (11). A composite list of ADHD side effects was strongly associated with a composite list of MW generated from analyzing data on task-unrelated thoughts during a lab session and everyday life in another study involving an adult population sample (12).
Moreover, a subclinical group with high ADHD symptom scores exhibited problematic mind-wandering episodes that hindered their daily-life performance. ADHD symptoms were also associated with mind-wandering episodes that were detrimental to the task at hand. The need for mindfulness when participating in mindfulness-based interventions was strongly linked to symptoms of ADHD. This study found that a lack of understanding of working memory (MW) moderated the relationship between ADHD side effects and impairment, indicating that increasing knowledge of MW in individuals with ADHD may lead to practical benefits (12).
Various methods have been used to treat the psychological conditions of children and adolescents. Barlow's meta-diagnostic therapy can be mentioned as one of these treatments (13). In this treatment, emotions and maladaptive strategies of emotion regulation are emphasized. Emotional experience and response to emotions are the meta-diagnostic approach's basis (13). Emotional experience and response to emotions are the main basis of the transdiagnostic approach. The goal of integrated transdiagnostic treatment is that the patients acquire skills to manage negative emotions effectively (14). Regarding the psychological conditions of ADHD children, they need to use appropriate intervention and treatment methods.
In Capobianco et al. study, mindfulness and metacognitive therapy are the two treatments accepted in the integrated treatment protocol of transdiagnosis for treating mental disorders (15). In the Barlow treatment protocol, mindfulness is one of the skills taught to people. In Rahl et al.'s research, Xu et al. stated that mindfulness meditation is associated with a reduction in mind wandering and an important outcome for the treatment of anxiety in anxious individuals (16, 17). Mitchell et al. showed the effectiveness of mindfulness meditation treatment on hyperactivity and attention deficit in adults and on the main symptoms, executive functioning, and emotional regulation (18). Schniering et al.'s research stated that meta-diagnostic therapy effectively treats comorbid anxiety and depression in adolescents (19). Carlucci et al. showed that transdiagnostic integrated protocol treatment could improve mental health, especially anxiety, and depression (20).
2. Objectives
Therefore, the present study aimed to investigate the effectiveness of transdiagnostic therapy on behavioral-emotional disorder and excessive mind wandering in children with ADHD.
3. Methods
3.1. Study Plan
In this clinical trial study, the research population consisted of all students referred to the West Health Center of Ahvaz in 2019 based on the inclusion criteria.
3.2. Sample Size
Thirty children with ADHD who met the inclusion criteria were selected using the simple random sampling method and then assigned to two intervention and control groups (n = 15 each). According to the following formula and similar studies (21), the sample size was determined to be 15 for each group.
Where,
d: Acceptable error, equal to the mean difference between the two groups in a previous study = 2.63
3.3. Sampling Method
The research population consisted of children with ADHD meeting the inclusion criteria. Based on the SCL90 questionnaire, a semi-structured clinical interview with a psychologist and a center physician received a score above 34 on the Connors questionnaire, and they were diagnosed with ADHD. Thirty children with ADHD were selected using the convenience sampling method. The selected children were randomly divided into the intervention (n = 15) and control (n = 15) groups.
3.4. Inclusion Criteria
The following factors were considered in order to check the necessary criteria of the participants to enter the research:
(1) No history of psychotherapy training
(2) At least a high school diploma in parents
(3) No family problems (divorce and separation) and couple problems in parents
(4) No history of mental disorder and not taking medication by the child
(5) Diagnosis of combined attention-deficit/hyperactivity disorder
3.5. Exclusion Criteria
(1) Simultaneous participation in counseling or other psychotherapy programs
(2) Not having an intellectual disability or other mental disorder (learning disorder or other developmental disorders)
(3) Diagnosis of attention deficit/hyperactivity disorder individually
3.6. Assessment Instrument
3.6.1. The Rutter Children Behavior Questionnaire (RCBQ) for Parents and Teachers
Rutter created a questionnaire in 1964 to assess behavior and distinguish between typically developing children and those with behavioral disorders, which was updated in 1967. The child's parent filled out Form A, which is for parents. There are 31 questions, 13 about the child's habits and health, and 18 about behavioral and emotional issues. A 30-question teacher form assesses a child's behavioral issues at school. The cutoff score for differentiating between normal and maladaptive children is between 8 and 13. The parent and teacher questionnaire is classified into 5 subgroups: (1) aggression/hyperactivity, (2) anxiety/depression, (3) social maladjustment, (4) antisocial behavior, and (5) attention deficit disorder (22). The questionnaire has a scoring range of 0 to 62. The test-retest reliability of the Rutter questionnaire was 89% on average (22). Edel claimed 68% reliability using test-retest and split-half methods. The validity of this questionnaire (percentage of agreement between the questionnaire and psychiatrist diagnosis) was significant at the level of 0.001, and the correlation was about 0.85 (23). In the present study, Cronbach's alpha of 0.82 was obtained in (RCBQ) for the sample.
3.6.2. Mind Excessively Wandering Scale
Mind wandering was measured utilizing the recently made Mind Excessively Wandering Scale (MEWS). This dissemination is the essential report of this scale. The MEWS is a 15-item self-report scale reflecting MW in ADHD. Asherson studied the extreme mind-wandering scale on hyperactive and attention-deficit children (24). This research investigated that by reducing items 6, 10, and 14, there was no decrease in the sensitivity and specificity of the scale. By repeating the analysis of the shorter 12-item scale, a sensitivity of 0.89 and a specificity of 0.9 was shown. The scoring of the items of this scale is based on the 4-point Likert scale: 0 = not at all, 1 = sometimes, 2 = most of the time, and 3 = almost always. The total score was between 0 and 36, with the score the cutoff of 15.
Internal consistency was high for all scales for both cases and controls (α > 0.78). The extreme mind wandering scale had a positive and significant correlation between medium and high with the spontaneous mind wandering questionnaire. This correlation in hyperactivity- attention deficit, attention deficit, and hyperactivity scales were 0.76, 0.76, and 0.71, respectively (23). In the present study, Cronbach's alpha for the MEWS was 0.8. Also, its correlation coefficient with the deliberate and spontaneous mind-wandering questionnaire was 0.59.
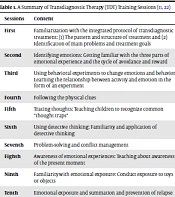
3.7. Intervention
The session content was based on the integrated TDT treatment protocol for emotional disorders for children and adolescents. There were 10 sessions of 45 minutes in the presence of parents and children twice a week by the researcher (after completing the training course of TDT) (25). The control group did not receive any intervention. After the end of the research, TDT intervention was implemented in the control group for ethical issues. After completing the last training session, the post-test was performed simultaneously and under the same conditions in two groups. A summary of sessions is displayed in Table 1.
| Sessions | Content |
|---|---|
| First | Familiarization with the integrated protocol of transdiagnostic treatment: (1) the pattern and structure of treatment and (2) identification of main problems and treatment goals |
| Second | Identifying emotions: Getting familiar with the three parts of emotional experience and the cycle of avoidance and reward |
| Third | Using behavioral experiments to change emotions and behavior: Learning the relationship between activity and emotion in the form of an experiment |
| Fourth | Following the physical clues |
| Fifth | Tracing thoughts: Teaching children to recognize common "thought traps" |
| Sixth | Using detective thinking: Familiarity and application of detective thinking |
| Seventh | Problem-solving and conflict management |
| Eighth | Awareness of emotional experiences: Teaching about awareness of the present moment |
| Ninth | Familiarity with emotional exposure: Conduct exposure to toys or objects |
| Tenth | Emotional exposure and summation and prevention of relapse |
3.8. Data Analysis
Quantitative data were analyzed using the mean and standard deviation. A multivariate analysis of covariance was used to examine the effect of TDT on studied variables. Levine's test was utilized to check the presumptions of MANCOVA. Data were analyzed in SPSS 16.
4. Results
Two cases in the control group dropped. The participants included 30 children aged 11.2 ± 1.2 years. Demographic variables of children with ADHD and parents are presented in Table 2.
| Cases | MCT | Control |
|---|---|---|
| Child's age | 11.2 ± 1.2 | 10.5 ± 1.5 |
| Age of parents | 25 ± 1.5 | 27 ± 2.1 |
| Child education | 5 ± 2 | 4 ± 2 |
| Gender | 6G and 9B | 6G and 9B |
Demographic Variables of the Participants (N = 15 per Group)
Table 3 presents descriptive data (mean and standard deviation) of behavior-emotional disorder and excessive mind wandering. The results showed that the mean scores of emotional-behavioral disorder changed from 31.33 to 23.4 and that of mind wandering from 18.93 to 15.26 after the intervention. The mean score of the subscales of Rutter's Children's Behavior Questionnaire also changed, including aggression/hyperactivity from 10 to 7.7, anxiety/depression from 4.8 to 3, social incompatibility from 5.5 to 4.6, antisocial behavior from 4.2 to 3, and inattention from 6.4 to 4.5 after the intervention. The homogeneity examination of change appeared that the centrality of Levene's test in the scores of emotional-behavioral disorder (0.146), excessive mind wandering (0.205), aggression/hyperactivity (0.102), anxiety/depression (0.421), social incompatibility (0.342) antisocial behavior (0.14) and inattention (0.62) were greater than 0.05. Subsequently, the homogeneity of change (HOV) presumption within the examined groups was met.
| Dependent Variables | Df1 | Df2 | F | P-Value |
|---|---|---|---|---|
| Behavior-emotional problems | 1 | 26 | 2.251 | 0.146 |
| Excessive mind wandering | 1 | 26 | 1.687 | 0.205 |
| Aggression/hyperactive | 1 | 26 | 2.882 | 0.102 |
| Anxiety/depression | 1 | 26 | 0.669 | 0.421 |
| Social maladjustment | 1 | 26 | 0.939 | 0.342 |
| Antisocial behavior | 1 | 26 | 2.317 | 0.140 |
| Attention deficit disorder | 1 | 26 | 0.243 | 0.626 |
Levin's Test of Homogeneity of Variance in the Dependent Variables of the Research
Table 4 shows a significant difference between the experimental and control groups regarding subordinate factors at the level of P < 0.000, so there was a critical difference between the two groups in at least one of the dependent variables. The impact measure coefficient appears that 34.53% of the difference between the two groups was related to the test intercession. The test control was 99.
| Name of Test | Value | Ratio F | Degree of Freedom Hypotheses | Degree of Error | Level | Size of Test | Power Effect |
|---|---|---|---|---|---|---|---|
| Pilay effect group | 0.600 | 17.266 | 2.000 | 23.000 | 0.000 | 0.600 | 0.999 |
| Lambda willkes | 0.400 | 17.266 | 2.000 | 23.000 | 0.000 | 0.600 | 0.999 |
| Hoteling effect | 1.501 | 17.266 | 2.000 | 23.000 | 0.000 | 0.600 | 0.999 |
| Largest root on | 1.501 | 17.266 | 2.000 | 23.000 | 0.000 | 0.600 | 0.999 |
Results of Multivariate Analysis of Covariance on the Mean Post-test Scores of Behavioral-Emotional Problems, Cognitive-emotional Regulation Strategy, and Mind Wandering of the Experimental and Control Groups
To find out this difference, a one-way analysis of variance was performed in Mancoe's text, and the results are shown in Table 5. It showed that transdiagnostic training caused a change in symptoms of the experimental group compared to the control group. According to the table, 41.54% of the effect of transdiagnostic training was reducing the variable of behavioral-emotional problems. After that, 20.8% of the effect size of transdiagnostic training affected excessive mind wandering. The test power was 100 and 99, respectively.
| Variables | The Sum of the Squares | Degree of Freedom | Mean of the Squares | F | Level of Significance | Effect Size | Power Effect |
|---|---|---|---|---|---|---|---|
| Behavioral-emotional problem | 497.069 | 1 | 497.069 | 41.547 | 0.000 | 0.634 | 1.000 |
| Mind wandering | 157.965 | 1 | 157.965 | 20.836 | 0.000 | 0.465 | 0.992 |
Results of a One-way Analysis of Variance on the Mean Post-test Scores of the Dependent Variables of the Experimental and Control Groups
Multivariate analysis of covariance was used to assess if the transdiagnostic treatment significantly reduced the subscales of emotional-behavioral disorder. Table 6 shows a significant difference between the test and control groups regarding dependent variables (aggression and hyperactivity, anxiety and depression, social incompatibility, antisocial behavior, and lack of attention) at the P < 000 level. In this manner, it can be expressed that there was a significant difference between the two groups in at least one of the dependent variables. The covariance analysis of one variable was performed in the Mancoe text to understand this difference.
| Name of Test | Value | Ratio F | Degree of Freedom Hypotheses | Degree of Error | Level | Size of Test | Power Effect |
|---|---|---|---|---|---|---|---|
| Pilay effect group | 0.916 | 36.887 | 5 | 17 | 0.00 | 0.916 | 0.100 |
| Lambda willkes | 0.084 | 36.887 | 5 | 17 | 0.00 | 0.916 | 0.100 |
| Hoteling effect | 10.849 | 36.887 | 5 | 17 | 0.00 | 0.916 | 0.100 |
| Largest root on | 10.849 | 36.887 | 5 | 17 | 0.00 | 0.916 | 0.100 |
Results of Multivariate Analysis of Covariance on the Mean Post-test Scores of Aggression/Hyperactivity, Anxiety/Depression, Social Incompatibility, Anti-social Behavior, and Attention Deficit Disorder of the Experimental and Control Groups
Table 7 shows that the F values of the dependent variables of aggression and hyperactivity, anxiety and depression, social incompatibility, and antisocial behavior were 16.36, 20.5, 42.33, and 11.09, respectively, which were significant at the levels of P < 0.001, P < 0.00, P < 0.00, and P < 0.003. The F value for the inattention variable was 0.346, which was not significant at the level of P < 0.563. The effect sizes in the dependent variables of aggression and hyperactivity, anxiety and depression, social incompatibility, and antisocial behavior were 16.36%, 20.5%, 42.3%, and 11.09% of the changes due to the experimental intervention.
| Variables | The Sum of the Squares | Degree of Freedom | Mean of the Squares | F | Level of Significance | Effect Size | Power Effect |
|---|---|---|---|---|---|---|---|
| Aggression/hyperactivity | 16.987 | 1 | 16.987 | 16.362 | 0.001 | 0.438 | 0.971 |
| Anxiety/depression | 21.006 | 1 | 21.006 | 20.500 | 0.000 | 0.494 | 0.991 |
| Social incompatibility | 6.967 | 1 | 6.967 | 42.339 | 0.000 | 0.668 | 1.000 |
| Anti-social behavior | 2.255 | 1 | 2.2.55 | 11.094 | 0.003 | 0.346 | 0.888 |
| Attention deficit disorder | 0.060 | 1 | 0.060 | 0.346 | 0.563 | 0.016 | 0.087 |
Results of a One-way Analysis of Variance on the Mean Post-test Scores of the Dependent Variables of the Experimental and Control Groups
5. Discussion
The results showed that the integrated transdiagnostic treatment significantly affected behavioral-emotional disorder and excessive mind wandering of children with ADHD. The present study indicated the significance of integrated transdiagnostic treatment for behavioral-emotional disorders of ADHD children. Behavioral-emotional disorders include five areas: Aggression/hyperactivity, anxiety/depression, social incompatibility, antisocial behavior, and inattention disorder. The present study showed that integrated transdiagnostic treatment significantly affected all areas except inattention. These findings were in line with the results of this research, which states that teaching mother's emotional management reduces the behavioral-emotional disorder of their sons (26). Moreover, this training significantly affects all areas of behavioral problems, except inattention. Another research stated that emotion regulation is associated with increased attention in the visual field and response inhibition (auditory and visual) in ADHD children (27). Other research has proposed transdiagnostic therapy as a model for improving executive function and quality of life (28).
In the explanation of the present study, it can be said that emotional impulsivity is higher in children with hyperactivity and attention deficit than in normal children. Children with hyperactivity and attention deficit take action without considering the effects of their actions and have difficulty controlling their responses (29). The integrated transdiagnostic therapy protocol teaches parents and children to identify their emotions, conduct behavioral tests to modify their emotions and behaviors, follow physical cues, track thoughts, and detect faulty thinking. This approach helps individuals face therapy with their emotions and develop positive adaptive strategies towards emotions, reducing behavioral-emotional disorders. Although symptoms of attention deficit decreased in the experimental group, as well as other components of behavioral problems, this decrease was not statistically significant. To explain this finding, it can be said that attention deficit has stronger biological foundations than behavioral problems and shows resistance to change (29). For this reason, the need to combine drug therapy with psychological therapy and longer training is felt.
The present study showed the significant effect of integrated transdiagnostic treatment on reducing excessive mind wandering in children with ADHD. Research has proposed metacognition and mindfulness as part of transdiagnostic treatment (15). Also, due to the lack of research directly examining integrated transdiagnosis on excessive mind wandering, the present study is based on one of the components of transdiagnostic treatment, namely mindfulness, in previous research (30). This inquire about is steady with inquire about stating that mindfulness instructs individuals to screen their display minute involvement in an open and tolerating way and diminish intellect meandering (16). Mindfulness treatment changes the attention from the inner world to the present world in students with high anxiety and reduces mental wandering (17).
In the explanation of the present study, it can be said that spontaneous mind wandering plays an important role in destroying the cognitive function and daily life of hyperactive and attention-deficit children (31). Transdiagnostic treatment involves training hyperactive children to become more aware of their emotions, thoughts, and behaviors in their current situation, with a particular focus on attention deficit. Various strategies that the interventions have taught parents and children help them use effective and practical techniques to deal with excessive wandering (25).
5.1. Conclusions
According to the present study, TDT significantly reduced excessive mind wandering and behavioral-emotional problems in children with ADHD. It is recommended that counseling centers use TDT as a psychological treatment along with drug treatment in children with ADHD and other diseases, including disobedience and conduct disorder in different age groups. One of the limitations of this research was that it was not double-blinded because the same therapist taught both treatments. Therefore, it would be better to teach two interventions by two different therapists. Another limitation was that the research sample included children aged 9 to 13 with specific eligibility criteria, making the results not generalizable to other children and teenagers.