1. Background
Cancer is the most well-known life-threatening disease in Western societies. Cancer is “a threshold of life, through which you can see when your life will end” (1). Based on the reports of the World Health Organization and the Ministry of Health of Iran, about 9.6 million people worldwide and about 112 thousand people in Iran will be added to the number of cancer patients annually. In the next 15 years, it will cause 80% of deaths in Iran (2). There are degrees of mental disorders in cancer patients, and the range of these disorders varies from depression, anxiety, lack of adaptation to the disease and reduced self-confidence, reduced life expectancy, loss of sense of coherence to emotional disorders, and fear of disease recurrence and death (3, 4).
Compared to other chronic diseases, it has the highest impact on the life expectancy of patients. The study conducted by Gu et al. in China on cancer patients revealed that the trend of life expectancy in these patients decreases, and the rate of cancer has a positive association with mortality and a negative association with life expectancy in both genders (5). Bower et al. also revealed that cancer reduces life expectancy in cancer patients up to three years after recovery (6). Based on the studies carried out in this area, it can be concluded that cancer is one of the factors that threaten the hope of cancer patients and affects the life expectancy of these patients, which needs more attention. Hope is an inner force that enriches life and helps cancer patients, especially breast cancer, to have a vision beyond their current disorder and pain (7). The studies suggest that patients with a high level of hope have a higher level of tolerance against pain and side effects of chemotherapy, radiation therapy, and long-term treatments (8, 9).
The study conducted by Irving et al. on female students revealed that the subjects in the hopeful group, compared to the hopeless subjects based on their scores on the hope scale, used more hopeful coping styles in the face of an imaginary task of diagnosing and treating cancer (10). In the control group, the level of hope and confidence of patients complaining of cancer pain was higher than that of other patients. The increase in uncertainty and hopelessness of patients is directly associated with the increase in the spread of pain (11). Functions such as psychological adaptation, physical health, and problem-solving skills are directly associated with hope (12). More positive thoughts toward life and a tendency toward the positive aspects of traumatic conditions can be observed in hopeful people in the recovery stage. Hopeful people are more potent in the face of prolonged and painful treatments since hope gives meaning to life and helps patients adapt to cancer (13).
Given what was stated above, it can be concluded that hope in cancer patients can help their treatment process. However, insufficient understanding and lack of knowledge about the disease affect the hope of these patients. Lack of understanding and insufficient knowledge of the disease is closely associated with non-compliance with treatment and its complications. This problem is due to the need for an effective care relationship between the elements of treatment and patient care. The solution to this problem is to improve care and treatment relationships. The concept of “partnership” in the process can be used to improve the relationship between the patient, nurse, and physician. The partnership care model was designed by Mohammadi in 2001 and implemented and evaluated to control hypertension in Babol City (14).
This model used the theory of partnership in care and nursing for the first time in Iran. A mixture was created that forms one of the structural elements of the model as the concept of “partnership care.” Based on this model, the authenticity and effectiveness of care depend on the correct and desirable form of the nature and quality of the care relationship (15). To achieve the model’s goals, the following steps are presented as a regular structure, which acts as a dynamic and interconnected set by observing the relationship and logical and evolutionary sequence. These steps are motivation, preparation, involvement, and evaluation. Specific action plans have been predicted for each step (16). The effects of using this care model on quality of life, social support, self-efficacy, and improvement of patients’ self-concept have been identified (16-23). However, no study was found to investigate the effect of this care model on life expectancy in cancer patients.
2. Objectives
The present study aimed to investigate the effect of nursing interventions based on the partnership care model on the life expectancy of cancer patients.
3. Methods
The present quasi-experimental interventional study with two control and intervention groups was done in 2021. The statistical population included cancer patients undergoing chemotherapy in the internal, blood, and oncology wards of educational hospitals in Shahrekord.
3.1. Sample
The inclusion criteria included having cancer, not suffering from mental illnesses, not suffering from other physical diseases, and being over 15 years old. The exclusion criteria included the occurrence of severe physical complications caused by the disease or treatment that the patient is unable to continue to cooperate, end-stage cancer, and unwillingness to continue participating in the study.
Based on the below formula, the sample size was determined as 25 people in the two control and intervention groups, and considering the probability of 20% dropout, the final sample size was estimated as 30 people for each group and a total of 60 people.
In the present study, samples entered the study according to inclusion criteria and were then divided into two intervention and control groups using random allocation software.
3.2. Data Gathering
The data collection instruments included a demographic information questionnaire, including gender, age, occupation, marital status, educational qualification, and blood type, and Schneider’s Life Expectancy Questionnaire. This questionnaire includes 12 questions scored on a 5-point Likert scale (I strongly agree: 5; I agree: 4; I have no opinion: 3; I disagree: 2; and I strongly disagree: 1). However, questions 3, 7, and 11 are scored in reverse. To get the overall score of the questionnaire, the minimum score is 12, and the maximum score is 60 (20).
The internal consistency of the whole questionnaire is 0.76 to 0.86, its test-retest reliability is 0.80, and at intervals of more than eight to ten weeks, it is higher than the mentioned value (21). In a study on 660 female students in Tehran, Cronbach’s alpha coefficient of this scale was obtained at 0.89 (22). The reliability of this questionnaire in the present study was also measured using Cronbach’s alpha calculation method, and it was estimated at 0.85, indicating acceptable reliability. The present study was conducted by obtaining permission from the Research Deputy and Ethics Committee of Shahrekord University of Medical Sciences, receiving the code of ethics IR.SKUMS.REC.1400.100, and submitting a written letter of introduction by the researcher to the head of Hajar and Kashani teaching hospitals in Shahrekord. By obtaining permission from the officials, based on the inclusion criteria, the research goals and the study implementation method were explained to the selected patients. After obtaining informed consent and emphasizing the confidentiality of the information, sampling was done. In the next stage, the questionnaires were submitted to the participants (the stage before the implementation of the intervention) and then collected after 48 hours. In the implementation stage, the intervention group participated in training classes in groups with 6 - 8 members for nine weeks. The research team presented the education, and each session was arranged according to the participant’s time. The content of the sessions is presented in Table 1 for the patients of the intervention group. The education content was provided based on the stage of the model, needs of patients, review literature, special books, and journal; then, the content was validated by ten academic remembers.
| Sessions | Title | Specific Goals | Strategy | Educational Aids | Duration |
|---|---|---|---|---|---|
| 1 | Motivation | 1: Explaining the current status of patients by presenting information about cancer and its complications. 2: mental problems, complications related to not maintaining morale and losing it. 3: Necessary explanations about the intervention to maintain and control mental states, how to maintain morale, mental rehabilitation, and how to give hope to patients. | Question and answer Group discussions | Clips, PowerPoint, pamphlets, and voice messages | Three 60-minute sessions |
| 2 | Preparation | 1: The cases related to the disease, the effects of the disease, the method of treatment, the statistics of the patients and those who have recovered, the description of mental problems, and the side effects of mental problems were discussed. 2: Stress and anxiety management, presentation of resilience and sense of coherence programs, and presentation of hope therapy training were conducted. 3: Discuss how to take medicines, the effects of treatment regimen on improving conditions, comparing conditions before and after stress, describing the conditions related to hopeful patients, and maintaining coherence. | Question and answer and group discussion | PowerPoint clips, pamphlets, and voice messages | Three 70-minute sessions |
| 3 | Involvement | This stage is one of the most important and sensitive strategic goals of the model. The content of the training sessions was a kind of final assessment and evaluation of the implementation of the model and giving the necessary feedback to the client and informing them of their participation. In this part, while examining the problems of the clients, the positive and negative results of the previous training and actions will be examined and reviewed, and the necessary guidance will be provided to correct the defects. | Question and answer and group discussion | Voice messages | Two 90-minute sessions |
| 4 | Evaluation | Re-completion of the questionnaires by patients | Question and answer | Social network and email | One session |
Content of Training Sessions
At the end of the training sessions, the training booklet was provided to the intervention group participants. The researcher developed this booklet by studying the available books and references, and a psychologist confirmed its content. It contained educational material about cancer and related care and was prepared according to education session goals. However, the control group only received routine intervention. Immediately after completing the training sessions, the questionnaires were again submitted to the research groups, and after enough time (48 hours), they were collected.
The final data were collected two months after the intervention, and the level of life expectancy in both the intervention and control groups was evaluated and measured again by the mentioned questionnaire. At the end of the study, the educational booklet was given to the patients of the control group.
3.3. Data Analysis
Finally, after collecting the data of the two studied groups before, immediately after, and two months after the data intervention, they were analyzed using SPSS 24 software and descriptive statistics (mean and standard deviation) and inferential statistics (t-test, chi-square test, Fisher’s exact test, or repeated measure ANCOVA). The normal distribution of all the quantitative variables in each group was approved by the Shapiro-Wilk test at P < 0.05.
4. Results
A total of 60 people entered the study and were randomly divided into two intervention and control groups with 30 cases each. There were no dropouts in the present study, and in general, all the subjects passed the training sessions successfully and completed the questionnaires. In total, the age of the patients ranged from 33 to 65 years, with a mean of 49.45 ± 8.45 years. The mean age of patients was 47.40 ± 1.27 years in the control group and 51.50 ± 1.71 years in the intervention group. The independent t-test showed no difference between the two groups regarding age (P = 0.060). Also, based on the chi-square test and independent t-test, both groups were homogeneous in terms of other demographic characteristics, such as marital status, education degree, gender, blood type, and occupation, before the implementation of the intervention (P < 0.05) (Table 2).
| Subgroup | Control Group | Intervention Group | P-Value |
|---|---|---|---|
| Marital status (married) | > 0.99 | ||
| Married | 26 (86.66) | 26 (86.66) | |
| Single | 4 (13.33) | 4 (13.33) | |
| Degree (bachelor’s degree) | 0.31 b | ||
| Under diploma | 8 (26.66) | 10 (33.33) | |
| Diploma | 6 (20) | 10 (33.33) | |
| Associate degree | 11 (36.66) | 4 (13.33) | |
| Bachelor | 4 (13.33) | 4 (13.33) | |
| Master and above | 1 (3.33) | 2 (6.66) | |
| Gender | 0.79 | ||
| Male | 17 (56.66) | 16 (53.33) | |
| Female | 13 (43.33) | 14 (46.66) | |
| Job | 0.68 | ||
| Self-employed | 13 (43.33) | 12 (40) | |
| Housewives | 9 (30) | 6 (20) | |
| Employed | 5 (16.66) | 7 (23.33) | |
| Retired | 3 (10) | 5 (16.66) |
Distribution of Demographic Characteristics of Patients a
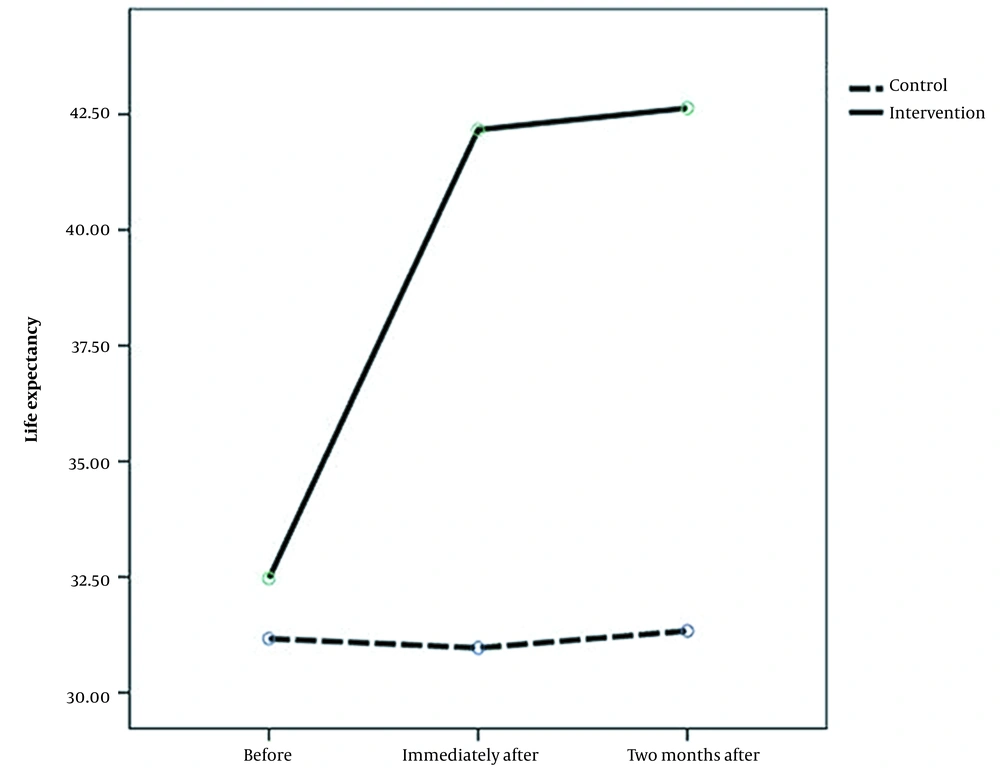
According to Table 3, there was no significant difference between the two groups at the beginning of the study in terms of the total score of life expectancy (before the intervention) (P = 0.82). In general, no significant difference was observed between them regarding the life expectancy component before the intervention (P > 0.05). Immediately and two months after the educational intervention, a significant difference was observed between the control and intervention groups regarding the life expectancy variable (P < 0.05). The result of repeated measure ANCOVA also revealed a significant difference in the trend of scores during the study in life expectancy (P < 0.05) so that a significant increasing trend can be observed in the intervention group. However, in the control group, no significant trend was observed in the scores of the three stages (P > 0.05, Figure 1).
| Group Stage | Control Group | Intervention Group | Between-Group Comparison |
|---|---|---|---|
| Life expectancy | |||
| Before the intervention | 3.05 ± 16.31 | 995. ± 46.32 | 0.82 a |
| Immediately after the intervention | 2.30 ± 96.30 | 4.16 ± 16.42 | < 0.001 b |
| Two months after the intervention | 2.12 ± 33.31 | 3.15 ± 63.42 | < 0.001 b |
| Repeated measurement | |||
| Time effect | 0.43 | < 0.001 | --- |
| Group effect | < 0.001 |
Mean and Standard Deviation of Life Expectancy Score of Patients in the Two Control and Intervention Groups During the Study
5. Discussion
The present study aimed to investigate the effect of nursing interventions based on the partnership care model on life expectancy in cancer patients in Shahrekord teaching hospitals. The results showed that the control and intervention groups were not significantly different before the intervention in terms of the level of life expectancy, while immediately and two months after the educational intervention, the life expectancy of the patients increased. In a study conducted by Rakhshan et al. to investigate the effect of the intervention based on the partnership care model on life expectancy in caregivers and patients with multiple sclerosis, this model improved life expectancy in multiple sclerosis patients and their caregivers (23). Although the mentioned study was carried out in a different statistical population and with a different type of disease from the present study, its results were consistent with this study (23).
Li et al. also examined the effectiveness of the nursing intervention to increase hope in cancer patients (24). The evidence suggests that nursing intervention has a positive effect on cancer patients’ hope. The results of this study were also consistent with those of the present study (24). In a study aimed at investigating the effect of supportive nursing care on the life expectancy of men with prostate cancer, Cockle-Hearne et al. also reported that supportive nursing care, access to nursing, and supportive care components, especially after treatment, can lead to increased hope in these patients (25). Koo et al. investigated the effect of patient partnership in the treatment process on the survival rate and hope of survival in cancer patients (26). They showed that patients who participated in their treatment process had more hope than patients who did not participate. Also, their treatment process decreased, which was consistent with the results of the present study (26).
Engelbak Nielsen et al. also showed that cancer patients are in a better condition if they participate in clinical trials and have better psychological conditions, which was consistent with the results of the present study (27). Movahedi et al. also stated that providing nursing intervention can effectively improve the life expectancy and general health of cancer patients, which was consistent with our results (28). With increasing pressure on patients caused by the complications of the disease, emotional changes begin in them. It was found that nursing interventions are significant for increasing the level of hope since it is the most common psychological factor after the diagnosis of the disease, and it can be considered the main factor contributing to the quality of life of patients. Patients with this disease often think about the end of their lives and lose hope after learning about it (29). In the partnership care model, face-to-face and written training were used to enhance knowledge on the nature of the disease, proper diet and physical activity, and aggravating and mitigating factors. The partnership care model made patients more sensitive and responsible toward treatment since it activated patients in the framework of team therapy. Additionally, in this model, they are placed in small groups and exchange ideas with physicians and nurses, which can give them hope to regain their health since the more a patient obtains knowledge about his or her disease and takes care of himself or herself and cooperates with the treatment team, he or she can take steps to maintain and improve his or her health and ultimately improve his or her quality of life, which can make him or her more hopeful.
Also, it can be stated that since the partnership care model as an intervention factor increases the person’s ability to cope with the stressful situation of the disease, this type of treatment increases the person’s adaptability and hope. By using this type of intervention, a person will be more capable in terms of mental health, especially adapting to life problems, including illness (even an incurable disease, such as cancer), which will increase his or her life expectancy, as the person is more psychologically prepared and his or her acceptance to cope with the complications caused by chemotherapy will be more (30).
In general, the nursing partnership care model creates a sense of security, hope, love, and life in the person so that he/she feels peace of mind and satisfied by living without fear of the future and the sadness of the past and also seeks to modify the goals and lifestyle through modifying communication. Having an optimistic attitude to life makes it easier to cope with the disease. It facilitates the recovery from both the physical and emotional aspects of all types of diseases, resulting in increased life expectancy. When a patient realizes that his or her disease can reduce complications with better management and adherence to what his or her physician prescribes, he or she will be more optimistic about the path of treatment and life (31).
Also, the active participation of patients should be transferred from care providers to patient-nurse partnership as much as possible. In the partnership care-based intervention, the patient plays a key role, and all care and treatment activities are focused on communicating with him or her. The goal of this program is to achieve relative independence, self-determination, health promotion based on capabilities, lifestyle, and increased quality of life, which all were achieved in the present study. Moreover, the effect of various social, economic, and cultural factors on the patient’s quality of life is inevitable (32).
Furthermore, involving the patient in self-care activities by encouraging him or her to express his or her problems, as well as involving the patient in setting goals and planning to solve problems through communication with him or her, has also played a significant role in increasing the cooperation between the patient and the treatment staff. This cooperation makes him or her aware of his or his treatment process, which makes him or her more hopeful than before, and has a more open view about the result of his or her treatment, which improves his or her life expectancy.
5.1. Study Limitations
However, the findings of this study should be considered along with its limitations. The participating patients were restricted to only one training hospital; thus, it is recommended that the research be repeated with a larger sample and in different centers. Also, it is recommended that the intervention be presented for more days and hours.
5.2. Conclusions
The present study aimed to investigate the effect of nursing interventions based on the partnership care model on the life expectancy of cancer patients in Shahrekord teaching hospitals. The results revealed the usefulness and effectiveness of the partnership care model in increasing the life expectancy of cancer patients. Given the positive effect of life expectancy on the recovery of patients, it is necessary to consider these psychological variables in patients and try to improve their level. Based on the obtained results, it can be stated that the partnership care model is a suitable intervention to improve the level of these variables. Thus, it is recommended for nursing professors and trainers in university settings, as well as nursing officials in clinical settings, to familiarize more nursing students and working nurses with the partnership care model to provide the necessary conditions to apply it. Also, since only the partnership care-based intervention was considered in this study and other effective educational interventions were ignored, it is necessary to use this care method along with other routine care models.