1. Background
Multiple sclerosis (MS) is among the most prevalent chronic conditions of the central nervous system (1), causing demyelination during which high numbers of axons are damaged (2). The symptoms of MS are classified as either observable symptoms (e.g., gait, balance, and vision disorders) (3) or unobservable symptoms (e.g., cognitive, psychological, fatigue, and pain disorders) (4). Approximately 2.5 million people worldwide have MS. This disease is three times more common in women than men. Although the onset is usually between 20 and 40 years, this disease can occur at any age (5). MS affects different aspects of a patient's life and causes the patient to experience severe stress (6). Hence, the patient must be trained in effective strategies for adapting to the disease to keep living. Given the problems and complications associated with pharmacotherapy, it is advisable to use non-pharmacological and psychological methods that can alleviate the anxiety, stress, and emotional problems of patients with MS (7).
Anxiety sensitivity is a variable that has drawn considerable attention among these patients (8). This concept refers to the fear of stress-related physical feelings (e.g., palpitations and difficulty breathing) interpreted as processes that have harmful physical, psychological, and social consequences. For instance, a patient who experiences physical feelings as threats or traumas (i.e., high anxiety sensitivity) will give a response (9). As the anxiety level increases when a patient experiences such feelings, anxiety-related problems often emerge (10). People with high anxiety sensitivity encounter stressful situations excessively through their feelings and thoughts. They experience extremely anxious responses to stressful situations with excessive readiness (11). Anxiety sensitivity is assumed to be a stable orientation variable that indicates the desire to interpret the physical, psychological, and social outcomes of anxiety experiences as annoying and dangerous affairs (12).
Given the growing number of women with MS and the lack of definitive medical treatments, it is now essential to employ psychotherapy as an alternative treatment that can enhance pharmacotherapy. The problems and limitations caused by MS can also affect a patient’s mental health. Hence, it is necessary to use effective cognitive therapies. Mindfulness-based cognitive therapy (MBCT) is a psychological treatment proven effective in alleviating psychological problems in patients with MS (13). MBCT aims to enable participants to communicate their thoughts, feelings, and physical states (14). It also aims to help participants quit inefficient habitual cycles such as rumination, emotional maladjustment, and self-criticism, making them vulnerable to other psychological disorders (15). Mindfulness-based interventions focus on non-judgmentally paying attention, especially on purpose, to the present moment (16). As a clinical intervention, mindfulness-based meditation has been proven to positively affect people's emotional and physical states, especially regarding emotional processing (17). Various studies have shown the effectiveness of mindfulness-based therapy in reducing rumination (17) and mental distress (18) in patients with MS and improving sleep quality in patients with HIV/AIDS (19). Lam et al. analyzed the effectiveness of mindfulness in regulating emotional processing among patients with schizophrenia-related disorders and observed significant improvements in reevaluation and a considerable reduction in rumination within a three-month follow-up period (20). According to Kenny and Williams, mindfulness training can alleviate symptoms of stress and anxiety by reducing emotional processing and increasing emotional regulation (21).
Since MBCT is a novel method, its effectiveness should be analyzed in different cases of psychological disorders. It can also lead to developments in treating mental disorders. The results of this study can be used in treatment centers to help patients with MS. Moreover, finding differences in effectiveness in Iranian cases concerning dependent research variables will also lead to important theoretical and practical implications that can help mental health experts adopt the most effective therapy along with pharmacotherapy.
2. Objectives
Based on the issues outlined in the background, the present study aimed to investigate the effects of MBCT on anxiety sensitivity in patients with MS.
3. Methods
3.1. Design and Participants
This quasi-experimental study adopted a pretest-posttest control group design with follow-up. The statistical population included all women with MS who enrolled in the Tehran MS Society in 2019 and 2020. To select the statistical sample, the researcher first separated patients with clinically isolated syndromes using interferon drugs (e.g., Rebif, Betaferon, Cinnovex, and Actovex) for controlling the course of the disease from the other MS groups. The patients were then matched concerning age, education, marital status, and time since diagnosis.
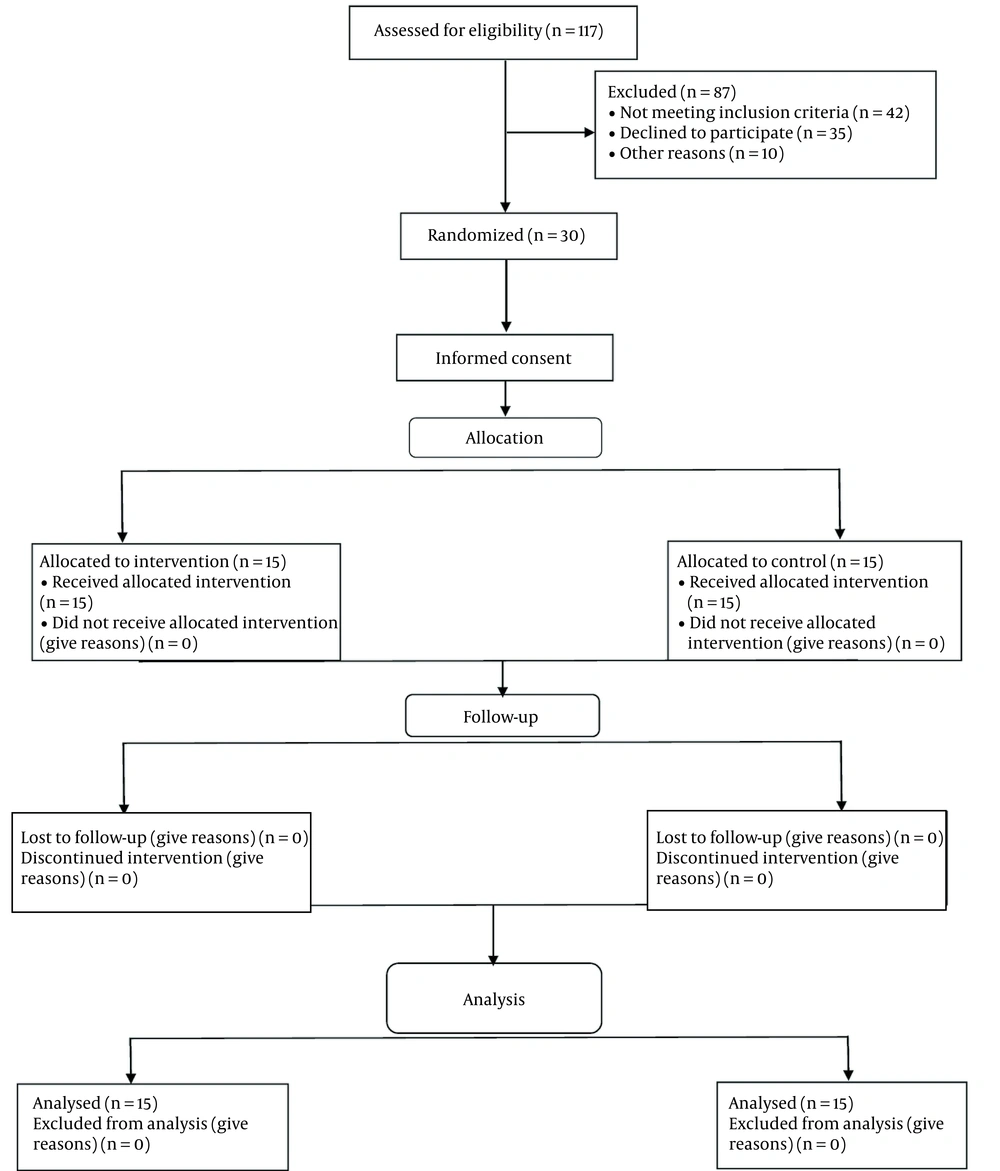
Convenience sampling was then employed to select 30 participants who were assigned randomly to an experimental group and a control group (15 members per group) (Figure 1). The adequacy of sample size was confirmed through G-Power software (ɑ = 0.05, effect size = 1.11, and power test = 0.90). The inclusion criteria were as follows: being diagnosed with MS based on a neurologist’s opinion based on MRI, being in the 20 - 40 age group, and having at least finished high school. The exclusion criteria were as follows: undergoing another therapeutic intervention concurrently, having comorbid psychological disorders (e.g., addiction and depression) or other chronic conditions such as diabetes, and being absent from more than two therapy sessions.
3.2. Ethical Considerations
For compliance with ethical considerations, informed consent forms were obtained from the participants. Moreover, an effective intervention was implemented for the control group after the research. The present research has been approved by the ethics committee of Semnan Islamic Azad University (code: IR.IAU.SEMNAN.REC.1399.009).
3.3. Procedure
The experimental group received eight 90-minute mindfulness-based stress alleviation interventions, whereas the control group received no training. Anxiety sensitivity was measured in both groups before the intervention for the pretest and again after the intervention for the posttest. The follow-up step was implemented three months after the intervention.
3.4. Research Instruments
3.4.1. Demographic Survey Questions
A researcher-made demographic survey questionnaire was used to collect demographic information from the participants. The questions of this questionnaire were to collect information related to age, duration of illness, and marital status of women.
3.4.2. Anxiety Sensitivity Index
The anxiety sensitivity index (ASI) was developed by Taylor and Cox and consisted of 30 items. This tool consists of four components: fear of respiratory symptoms, fear of publicly observable anxiety reactions, fear of cardiovascular symptoms, and fear of cognitive dyscontrol. The ASI is scored on a five-point Likert scale (i.e., “1” for “very low,” “2” for “low,” “3” for average, “4” for “high,” and “5” for “very high”). The minimum and maximum scores are 30 and 150, with higher scores indicating greater anxiety sensitivity (22). According to the results reported by Taylor and Cox, this tool has acceptable validity and reliability and is useful and effective in measuring and evaluating anxiety sensitivity (22). They reported that the internal consistency of the ASI score was 0.95. Foroughi et al. (23) reported an alpha Cronbach coefficient of 0.90 for the tool.
3.5. Treatment Protocol
3.5.1. Mindfulness-Based Cognitive Therapy Protocol
The mindfulness-based cognitive therapy (MBCT) sessions were based on the protocol developed by Kabat-Zinn (24) in eight 90-minute sessions. This therapeutic approach integrates the elements of cognitive-behavioral therapy for depression with the principles and skills of mindfulness (24). Table 1 gives a summary of the contents of the intervention sessions.
| Session | Objective | Content |
|---|---|---|
| 1 | Getting to know the concept of mindfulness | Introducing members to each other; explaining the nature of therapy sessions; presenting the concept of mindfulness and its role in stress alleviation |
| 2 | Learning about mindfulness techniques and the correlation between mindfulness and stress | Providing relaxation training by creating and relieving tension in muscles, learning about the wandering mind, and practicing paying attention to your body and respiration |
| 3 | Teaching how to tame the wandering mind and its relationship with positive and negative thoughts | Teaching how to relax by recalling muscular groups, performing sitting meditation, and doing the exercises that keep attention focused on the present moment, controlling s negative automatic thoughts |
| 4 | Teaching, observing thoughts, and living in the moment | Practicing breath control training; acquiring knowledge about thoughts and feelings; observing thoughts without making value judgments and controlling negative automatic thoughts |
| 5 | Relaxation techniques and meditation | Relaxation training and meditation in different situations; teaching presence at the moment and observing thoughts together with positive thoughts |
| 6 | Teaching the relationships between thoughts and moods, and negative feelings | Teaching the relationships of thoughts with moods and negative feelings; sitting meditation; concentration on emotional feelings; changing moods and thoughts based on the type of their relationships |
| 7 | Teaching the techniques of tolerating distress and controlling negative automatic thoughts | Teaching the technique of tolerating distress to control negative automatic thoughts and create positive thoughts |
| 8 | Implementing stress alleviation techniques to control negative thoughts in real-life environments | Revising stress alleviation techniques, using those techniques at the moment, and generalizing them to the entire real-life process |
The Structure of Mindfulness-Based Cognitive Therapy Sessions
3.6. Statistical Analyses
Data analysis was performed in SPSS. The Shapiro–Wilk test was conducted to check the normal distribution of the variables in both the pretest and posttest. Moreover, Levene's test was employed to analyze the homogeneity of variance. Finally, repeated measures of ANCOVA were utilized to analyze the effects of mindfulness-based cognitive therapy on anxiety sensitivity in women with MS.
4. Results
The participants in the present study were 30 women with MS. The mean age of women was 37.21 ± 5.78 years. Also, the duration of the disease in the participants was 5.81 ± 2.43 years. Twenty (66.67%) women were married, and 10 (33.33%) were single. The mean ± standard deviation (SD) of the pretest, posttest and follow-up scores of anxiety sensitivity in the experimental group were 101.66 ± 2.63, 93.86 ± 3.11, and 94.00 ± 3.62, respectively, which was significantly different from the control groups. Table 2 presents the means and SD of the scores on anxiety sensitivity components for both groups in the pretest, posttest, and follow-up.
| Variables | Phases | MBCT Group, Mean ± SD | Control Group, Mean ± SD |
|---|---|---|---|
| Fear of respiratory symptoms | Pretest | 23.73 ± 1.48 | 23.60 ± 1.24 |
| Posttest | 22.06 ± 2.15 | 23.53 ± 1.59 | |
| Follow-up | 21.13 ± 2.29 | 23.60 ± 1.68 | |
| Fear of cardiovascular symptoms | Pretest | 47.93 ± 2.71 | 37.00 ± 2.24 |
| Posttest | 34.60 ± 1.80 | 37.06 ± 2.15 | |
| Follow-up | 35.82 ± 1.60 | 37.00 ± 2.04 | |
| Fear of publicly observable anxiety reactions | Pretest | 23.60 ± 1.27 | 23.93 ± 1.71 |
| Posttest | 21.66 ± 1.60 | 23.93 ± 1.95 | |
| Follow-up | 21.73 ± 1.75 | 24.13 ± 1.68 | |
| Fear of cognitive dyscontrol | Pretest | 17.33 ± 2.71 | 17.46 ± 2.24 |
| Posttest | 15.20 ± 1.80 | 17.46 ± 2.15 | |
| Follow-up | 15.13 ± 1.60 | 17.60 ± 2.04 | |
| Anxiety sensitivity (total) | Pretest | 101.66 ± 2.63 | 102.33 ± 3.60 |
| Posttest | 93.86 ± 3.44 | 102.00 ± 3.83 | |
| Follow-up | 94.00 ± 3.62 | 102.40 ± 3.22 |
Mean and Standard Deviation (SD) of the Anxiety Sensitivity Components in the Experimental and Control Groups
According to the Shapiro–Wilk test results, the significance level was 0.05 for anxiety sensitivity components; hence, the research variables had a normal distribution. It was then possible to use the repeated measures ANCOVA. According to the results, the F-statistic of Levene’s test was not significant for the homogeneity analysis of the research variable in the experimental and control groups. Therefore, it was possible to use repeated measures of ANCOVA.
The results indicated that mindfulness-based cognitive therapy mitigated anxiety sensitivity components in women with MS, whereas no significant differences were observed in the control group (Table 3). According to Table 3, the mutual effect of group × time was significant on anxiety sensitivity (P < 0.001). It was determined that the means of the MBCT group were significantly lower than those of the control group when it came to the total anxiety sensitivity score and scores for all four components (i.e., fear of respiratory symptoms, fear of publicly observable anxiety reactions, fear of cardiovascular symptoms, and fear of cognitive dyscontrol).
| Variables | Source | SS | df | MS | F | η2 | P-Value |
|---|---|---|---|---|---|---|---|
| Fear of respiratory symptoms | Time | 37.43 | 2 | 18.71 | 2.48 | 0.11 | 0.046 |
| Group | 36.63 | 1.77 | 20.59 | 21.96 | 0.34 | 0.001 | |
| Time × group | 25.98 | 3.55 | 7.32 | 7.97 | 0.27 | 0.001 | |
| Fear of cardiovascular symptoms | Time | 44.58 | 2 | 22.27 | 3.54 | 0.14 | 0.038 |
| Group | 29.43 | 1.49 | 19.71 | 158.96 | 0.79 | 0.001 | |
| Time × group | 22.11 | 2.98 | 7.40 | 59.72 | 0.74 | 0.001 | |
| Fear of publicly observable anxiety reactions | Time | 62.68 | 2 | 31.34 | 4.83 | 0.19 | 0.013 |
| Group | 23.88 | 1.91 | 12.44 | 137.61 | 0.77 | 0.001 | |
| Time × group | 20.16 | 3.83 | 5.25 | 58.09 | 0.73 | 0.001 | |
| Fear of cognitive dyscontrol | Time | 59.65 | 2 | 29.83 | 6.32 | 0.23 | 0.004 |
| Group | 30.68 | 1.68 | 18.17 | 268.46 | 0.87 | 0.001 | |
| Time × group | 25.18 | 3.37 | 7.46 | 110.18 | 0.74 | 0.001 | |
| Anxiety sensitivity | Time | 800.54 | 2 | 400.27 | 10.70 | 0.34 | 0.001 |
| Group | 467.65 | 1.89 | 247.37 | 238.49 | 0.85 | 0.001 | |
| Time × group | 361.98 | 3.78 | 95.73 | 92.30 | 0.82 | 0.001 |
Repeated Measurement Results for the Effects of Time and Interaction Time and Group
5. Discussion
The present study aimed to investigate the role of MBCT on anxiety sensitivity in women with MS in Tehran. The research findings indicated that mindfulness-based cognitive therapy influenced anxiety sensitivity in women with MS. These results are consistent with the results of previous studies (25). Hoogerwerf et al. (25) reported that MBCT had a positive effect on the reduction of severe fatigue and several psychological factors in patients with MS. Unlike the anxiety attribute that points to the willingness to experience anxiety symptoms, anxiety sensitivity includes the principle that exaggeration of anxiety response facilitates acquiring conditioned fear of an annoying stimulus. This mindset acts as a risk factor for anxiety disorders and panic disorders. According to the cognitive theories of anxiety, the conceptualization of anxiety sensitivity indicates that negative cognitive appraisal is a risk factor in creating and maintaining anxiety. These theories state that negative cognitive evaluation of a physical feeling causes a quick setup of anxiety that can exacerbate feelings of anxiety (26).
The MBCT is a skill training program that teaches clients to identify and detach from ruminative and negative thoughts (27). Mindfulness helps people shift from a mental state in which they always evaluate and judge performance to a mental state of existence (25). Although existence might be considered a pure concept, it is partly similar to the feeling of being encouraged for new success, openness, and readiness to encounter misperceptions that used to be followed (28). There is also a similarity between this state and the temporary disorientation experienced by an individual after adopting a new path. The MBCT causes people to reduce their negative evaluations of the disease and provide opportunities for revision and favorable evaluations. Reducing negative evaluations and non-judgmental interactions will reduce the cognitive deviations caused by the negative approach to the condition in the person's mind. As a result, people's cognitive processing will be done with better efficiency. Such an approach reduces the involvement of patients' thoughts and feelings, leading to decreased anxiety and worry about the disease and life (25).
Teaching meditation and improving mindfulness enhances mental balance in patients with MS. Meditators manifest higher levels of mindfulness, better attention performance, and higher levels of cognitive flexibility. Attention performance and cognitive flexibility are positively correlated with levels of mindfulness. In the first step of mindfulness training, a patient is asked to practice mindful breathing and, when this awareness extends to thoughts, feelings, or physical senses, return to concentration and mindful breathing (13). By repeating the return of awareness to mindful breathing, patients are helped to know about the nature of mindfulness activities and distinguish between mental activities and their responses to these activities.
Due to mindfulness exercises and awareness of physical and mental sensations, the participants realize that their heart rate and breathing change when anxious. By doing exercises, the participants focus their attention more on the body, which increases the awareness of the body, feelings, and thoughts related to anxiety; as a result of this awareness, the feeling of controlling the symptoms and then reducing the anxiety. Moreover, in patients with MS, the change in awareness from mental content to mindful breathing can interfere with rumination processes and reduce the potential power of mental events, thereby mitigating impulsive, reactive, or spontaneous responses to these events. Cognitive therapy is a psychotherapy based on the theory of emotional disorders, clinical studies, and empirical studies. This therapy is an organized version of psychotherapy designed to alleviate symptoms and help patients learn effective methods of coping with disturbing problems. In this therapy, all efforts are focused on problem-solving (27).
5.1. Limitations
This study faced limitations, such as the vicissitudes of MS and the use of therapeutic drugs to control symptoms during the interventions in both experimental and control groups. The study was also limited to women with MS who had enrolled in the Tehran MS Society; therefore, caution should be exercised when generalizing the research results to other statistical populations. It is recommended that future studies include other populations and male participants.
5.2. Conclusions
According to the research results, the mindfulness-based cognitive therapy intervention with reprocessing can affect the anxiety sensitivity of women with MS through available techniques and methods. Hence, it is recommended that mindfulness-based cognitive therapy techniques be adopted to reduce anxiety sensitivity in patients with MS.