1. Background
Schizophrenia, as a severe mental illness, leads to impaired reality evaluation, emotion dysregulation, impaired thinking, impaired decision-making, and severe communication problems (1). Schizophrenia, or psychosis, is a severe and extremely destructive clinical syndrome affecting cognition, emotion, perception, and other behavioral aspects. Schizophrenia usually starts before age 25 and persists lifelong in some cases, and may affect individuals belonging to any social class (2). Schizophrenia is one of the most debilitating psychotic disorders. In addition, schizophrenia and severe mental illnesses are increasingly considered neurological disorders (3). It has been reported in most studies that the cognitive impairment that starts from the first period of schizophrenia continues at least until middle age (4, 5). Also, the prevalence of schizophrenia is approximately one percent (6), and 5 - 25% of individuals with this disorder are treated annually. Moreover, its prevalence is equal in men and women, but the disease onset is earlier in men (7).
Emotional intelligence is also another construct that plays a fundamental role in various disorders (8). Emotional intelligence is a type of non-cognitive intelligence that includes cognition, emotions, appropriate decision-making, the ability to manage one's mood appropriately, impulse control, and desirable social skills (9). One of the main components of emotional intelligence is the emotion regulation process. There are several definitions of emotion regulation. Emotion regulation specifically describes how individuals experience, organize, or regulate emotions, which increases their tolerance in situations of helplessness and helps manage or regulate emotions, including awareness, acceptance, and understanding of emotions to control impulsive behaviors (10). Emotion regulation refers to a wide range of biological, social, and behavioral processes (11). It is also a process in which emotions automatically or voluntarily monitor, evaluate, and modify emotional reactions to pain (12). Many studies have been conducted on the role of emotion regulation or emotion dysregulation due to various disorders, particularly schizophrenia (13). The Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5) also introduces a defect or disorder in emotion regulation, along with a disorder in cognition or behavior, as one of the essential elements in the definition of a mental disorder (14). It is believed that there is a wide range of deficits and problems of emotion regulation in schizophrenia (15), and emotion regulation in schizophrenia may initiate a new insight into this disorder, in which mood instability may be a prominent feature, possibly forming schizophrenia (16).
Today, there is no doubt about the use of psychological treatments in the treatment of schizophrenia because drug therapy, which is considered the first-line treatment in schizophrenia, has some limitations. However, despite the use of medicine, the high rate of relapse continues. In addition, a large number of patients still suffer from persistent positive symptoms, and common antipsychotic drugs have limited effects on negative symptoms and impaired cognitive functions and social functioning (17). Therefore, due to the limitations of drug therapy, much attention has been paid to the treatment of schizophrenia in the field of psychology, and a variety of treatments have been proposed to deal with this disorder effectively; however, what should be noted is the difference between these interventions in terms of ease of implementation and continuity of treatment outcomes. In this regard, researchers have shown that cognitive-behavioral therapy (CBT) significantly affects the improvement of schizophrenia (18).
CBT is a combination of cognitive behavioral approaches, helping the patient to recognize his/her distorted and ineffective thinking patterns through Socratic discussions and organized behavioral assignments. The emphasis is mainly on the behavioral dimension in some aspects of the treatment and the cognitive dimension in other aspects (19). In fact, it can be stated that the quality of life improves when CBT is used. Godfrin & van Heeringen, as well as Driessen & Hollon, have concluded that this intervention affects all aspects of an individual’s life and significantly affects an individual’s increased satisfaction with his/her life (20, 21). There is also strong evidence that the combination of drug therapy and CBT leads to reduced relapse and a longer recovery duration in psychotic patients compared to drug therapy alone (22). Recent studies have shown that CBT has been effective in preventing relapse in patients with schizophrenia (23). A study on the effectiveness of CBT on positive symptoms of schizophrenia showed that CBT increased positive symptoms in individuals with schizophrenia (24).
Considering that schizophrenia is one of the most destructive psychiatric disorders, and according to the literature review, few studies have been conducted on the effectiveness of CBT on emotional self-regulation in these patients; therefore, the present study seems important, contributing to more knowledge in disease pathology. Also, given that emotional intelligence and emotional self-regulation play an important role in behaviors and social relationships, such research can be effective and helpful in clinical and treatment centers.
2. Objectives
The current study aims to answer the following basic question: Is CBT effective on emotion self-regulation and its components in patients with schizophrenia?
3. Methods
3.1. Design
The current research is a semi-experimental study with a pretest-posttest design and a control group.
3.2. Samples
The study population includes all patients with schizophrenia who were admitted to Hayat Rehabilitation and Treatment Center for Chronic Mental Patients in 2021 - 2022.
The sample size of the present study was determined by referring to Cohen's table to specify the sample size in experimental studies and taking into account the effect size of 0.70, the test power was 0.91, the significance level was 0.05, and the minimum sample size for each group was 15 people. In addition to Cohen's formula, according to Gall et al., translated by Nasr, the criterion for selecting 15 people for each group is also based on previous studies and experts' opinions, so in semi-experimental studies, a 15-people sample size is considered sufficient (25). Accordingly, 30 people were selected and randomly assigned to experimental and control groups using the convenience sampling method (n = 15 per group). The Self-regulation Inventory (SRI-25) was completed by both groups in the pre-test phase, and the experimental group then received CBT for eight 60-minute sessions per week. Finally, the SRI-25 was completed by both groups in the post-test phase.
The objectives of the study were explained to all participants. All ethical principles were observed, including signing a voluntary informed consent, the right to withdraw from the study at any stage, non-disclosure of information, the confidentiality of all data, and avoiding harm to participants. The research protocol was approved by the Research Ethics Committee of Islamic Azad University (code: IR.IAU.ZAH.REC.1401.067).
The research inclusion criteria included being able to read and write, having a brain injury, having dementia, having a special neurological disease that needs special care, not receiving electroshock at least six months before the study, and finding no shock during the treatment The exclusion criteria were being illiterate, having no brain injury, having no dementia, and having no special neurological disease that needs special care. The patient should not have been seriously affected by the side effects of antipsychotic drugs in such a way that he/she was required to receive special treatment except for the usual treatments. If the patient received an electroshock for any reason during the treatment, he/she would be excluded from the study; also, the patient should not have received psychological treatment, such as metacognitive therapy, music therapy, or family therapy.
3.3. Intervention
The content and goals of the sessions were taken and expanded from the “Cognitive-Behavioral Therapy of Schizophrenia” book by Kingdon and Turkington (26). The training sessions aimed to improve emotion regulation through question-answer and group discussion. The summary of the meetings is presented in Table 1.
| Session | Content and Activities of Each Session |
|---|---|
| First session | Establishing a therapeutic relationship and familiarizing the patient with CBT and group rules |
| Second session | Teaching conversation and negotiation skills |
| Third session | Teaching problem-solving skills |
| Fourth session | Anger and aggression control training |
| Fifth session | Teaching relaxation techniques |
| Sixth session | Stress management skills training |
| Seventh session | Identifying negative thoughts, logical responses to negative thoughts, and correcting them |
| Eighth session | A review of previous sessions and answer the questions |
Abbreviation: CBT, cognitive-behavioral therapy.
3.4. Instruments
3.4.1. The Self-regulation Inventory
The Self-regulation Inventory (SRI-25) created by Ibanez et al. contains 25 questions and five subscales (positive functioning, controllability, disclosure of feelings and needs, assertiveness, and well-being seeking) and is scored on a five-point Likert scale from 1 to 5. Psychometric properties of the scale have been approved in foreign (27, 28) and domestic (29) preliminary studies. For the 72-question version, Cronbach's alpha coefficient is 0.74 - 0.92. (30), and for the 25-item version, it is 0.68 - 0.84 (28), confirming the scale’s internal consistency. The one-month test-retest reliability of the SRI-25 has been reported to be 0.87 (30). Examining the psychometric properties of the Persian version of the questionnaire in a sample of 676 students, Cronbach's alpha of each subscale was 0.90 - 0.97, indicating good internal consistency of the test. The correlation coefficients of 134 people from the above-mentioned sample size were calculated twice with a four-six-week interval to measure test-retest reliability. The correlation coefficient for the total scores of self-regulation (r = 0.875), positive performance (r = 0.82), controllability (r = 0.71), disclosure of feelings and needs (r = 0.78), assertiveness (r = 0.80), and well-being seeking (r = 0.86) were significant at a P < 0.001 level. Also, these coefficients confirmed the scale’s retest reliability (31).
3.5. Statistical Analysis
The data obtained from the present study were analyzed using descriptive statistics (mean and standard deviation (SD)) and inclusive inferential statistics (multivariate analysis of covariance (MANCOVA)) using SPSS software version 16.
First, assumptions of the MANCOVA test, including the normality of the data distribution, the variance homogeneity, and the slope of the regression line, were investigated.
4. Results
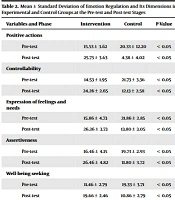
The analysis of the covariance (ANCOVA) test was used to answer the question of whether CBT has a significant effect on emotion self-regulation and its components (positive actions, controllability, expression of feelings and needs, assertiveness, and well-being seeking) in patients with schizophrenia. Furthermore, the Kolmogorov-Smirnov test was used to determine the normality of the data related to positive actions in the pre-test (K-S = 1.06, P ≥ 0.20) and post-test (K-S = 0.62, P ≥ 0.83), controllability in the pre-test (K-S = 0.17, P ≥ 0.12) and post-test (K-S = 0.82, P ≥ 0.50), expression of feelings and needs in the pre-test (K-S = 1.10, P ≥ 0.17) and post-test (K-S = 0.91, P ≥ 0.37), assertiveness in the pre-test (K-S = 0/68, P ≥ 0.74) and post-test (K-S = 0.71, P ≥ 0.68), well-being seeking in the pre-test (K-S = 0.43, P ≥ 0.99) and post-test (K-S = 0.74, P ≥ 0.63), and emotion regulation in the pre-test (K-S = 0/71, P ≥ 0.69) and post-test (K-S = 1.25, P ≥ 0.08). The results showed a significant difference (0.05), and all the components of emotion regulation were normally distributed (Table 2).
| Variables and Phase | Intervention | Control | P-Value |
|---|---|---|---|
| Positive actions | |||
| Pre-test | 15.53 ± 3.62 | 20.33 ± 12.20 | < 0.05 |
| Post-test | 25.73 ± 3.63 | 4.38 ± 4.02 | < 0.05 |
| Controllability | |||
| Pre-test | 14.53 ± 1.95 | 21.73 ± 3.36 | < 0.05 |
| Post-test | 24.26 ± 2.65 | 12.13 ± 2.58 | < 0.05 |
| Expression of feelings and needs | |||
| Pre-test | 15.86 ± 4.73 | 21.86 ± 2.85 | < 0.05 |
| Post-test | 26.26 ± 3.73 | 13.80 ± 3.05 | < 0.05 |
| Assertiveness | |||
| Pre-test | 16.46 ± 4.15 | 19.73 ± 2.93 | < 0.05 |
| Post-test | 26.46 ± 4.82 | 11.80 ± 3.72 | < 0.05 |
| Well-being seeking | |||
| Pre-test | 11.46 ± 2.79 | 19.33 ± 3.71 | < 0.05 |
| Post-test | 19.66 ± 2.46 | 10.86 ± 2.79 | < 0.05 |
| Emotion regulation | |||
| Pre-test | 73.86 ± 7.20 | 103.00 ± 8.19 | < 0.05 |
| Post-test | 122.40 ± 7.42 | 60.80 ± 7.94 | < 0.05 |
As Table 3 shows, the assumption of variance homogeneity was confirmed since there was no statistically significant difference between the studied variables.
| Tests of Variance Homogeneity | F | DF1 | DF2 | P-Value |
|---|---|---|---|---|
| Research variables | 0.63 | 1 | 28 | 0.43 |
| Positive actions | 0.08 | 1 | 28 | 0.77 |
| Controllability | 1.10 | 1 | 28 | 0.30 |
| Expression of feelings and needs | 0.41 | 1 | 28 | 0.52 |
| Assertiveness | 0.10 | 1 | 28 | 0.74 |
| Well-being seeking | 0.14 | 1 | 28 | 0.70 |
Another assumption of ANCOVA is the regression line slope. The results of different dimensions were as follows: Positive actions (f = 0.85, P = 0.54), controllability (f = 0.06, P = 0.79), expression of feelings and needs (f = 0.20, P = 0.89), assertiveness (f = 0.38, P = 0.86), well-being seeking (f = 1.36, P = 0.29), and the total score of emotion regulation at the pre-test and post-test stages (f = 1.26, P = 0.38). The results of the homogeneity of the slope of the regression line showed that the data supported the slope of the regression hypothesis due to the significance level of P < 0.05. Due to the confirmation of the three conditions, we can now take the MANCOVA.
The results of the Wilks's lambda test, comparing the cognitive behavioral therapy training intervention group with the control group in terms of a new variable obtained from the linear combination of dependent variables, indicate a significant difference overall (Wilks' lambda = 0.07, f = 49.31, P < 0.05). The results demonstrate a significant difference between the intervention group and the control group based on the dependent variables, with this difference accounting for 62% of the variance. In other words, 62% of the variance can be attributed to the differing influence of the dependent variables between the experimental and control groups. To further explore which specific dependent variables show a significant difference between the two groups, univariate covariance analysis was conducted using the MANKOVA test, and the results are presented in Table 4.
| Variables | Sum of Squares | Degrees of Freedom | Mean Square | F | Significance Level | Effect Size |
|---|---|---|---|---|---|---|
| Positive actions | 366.95 | 1 | 366.95 | 68.47 | 0.05 | 0.74 |
| Controllability | 346.85 | 1 | 346.85 | 61.86 | 0.05 | 0.72 |
| Expressing feelings and needs | 398.76 | 1 | 398.76 | 50.88 | 0.05 | 0.68 |
| Assertiveness | 546.40 | 1 | 546.40 | 58.71 | 0.05 | 0.71 |
| Well-being seeking | 251.69 | 1 | 251.69 | 62.62 | 0.05 | 0.73 |
In order to test the hypotheses more precisely, the results of MANCOVA for each of the CBTs are given below.
After removing the pre-test effect on the dependent variables, the results of Table 4 show a significant difference between the adjusted mean scores of positive actions (f = 68.47, η2 = 0.74, P < 0.05), controllability (f = 61.86, η2 = 0.72, P < 0.05), expression of feelings and needs (f =50.88, P < 0.05, η2 = 0.68), assertiveness (η2 = 0.71, P < 0.05, f = 58.71), and well-being seeking (η2 = 0.73, P < 0.05, f = 62.62) at the pre-test and post-test stages. According to the eta coefficients, CBT was the most effective on the positive actions variable (0.74%); that is, 0.74% of the difference in the follow-up scores of the positive actions variable is related to the CBT effect.
5. Discussion
The present study aimed to determine the effectiveness of CBT on emotion self-regulation and its components in patients with schizophrenia. The results of the current research showed that CBT improved emotion self-regulation and its components in patients with schizophrenia in the post-test stage (Table 4), which are consistent with some previous studies (13, 32, 33).
The literature review shows no similar research published on the effectiveness of CBT on clinical symptoms of schizophrenia. Therefore, the current research is considered an innovation and initiative in using CBT to reduce clinical symptoms and fear of negative evaluation of patients with schizophrenia. For this reason, the results of the current research are compared with the results of studies on similar variables and finally explained.
The results of previous studies have shown that CBT reduces the patients’ negative and increases positive symptoms, leading to improving the patients’ cognitive and behavioral performance, while in the control group, no change was observed in any of the scales at the three evaluation stages. The cause of schizophrenia requires a comprehensive treatment plan. Cognitive-behavioral therapy, which is based on sociocultural principles and conditions, can play an effective role in improving cognitive and behavioral performance and reducing disease symptoms (32). Schizophrenia causes a decline and defects in the emotion regulation process in those suffering from this disorder (13). For this reason, the use of some adaptive emotion regulation strategies, such as cognitive re-evaluation in facing anxiety and reducing negative emotions, can increase positive emotions in many cases (34). The emotion regulation ability can be acquired and learned through training and practice. Therefore, CBT effectiveness can be explained by the processes governing it (35). This treatment specifies values and committed actions, and the use of adaptive emotion regulation strategies under stressful situations and negative emotions is an important factor in improving physical and mental health. Therefore, maladaptive emotion regulation strategies lead to increased anxiety and depression (36). However, adaptive regulation strategies, such as acceptance, refocusing on planning, and putting into perspective, will positively affect the individual's social performance and lead to the cognitive reconstruction of the problem and, consequently, improved mental health status. CBT challenges negative thoughts, such as self-blame, and replaces logical thoughts, including positive re-evaluation, and individuals are asked to emphasize, practice, and deepen it.
Therefore, CBT can have a significant effect on improving cognitive emotion regulation (37). Patel et al. showed in their study that CBT was more effective than drug therapy in reducing the severity of schizophrenia symptoms (38). Wykes et al. also found in their study that cognitive rehabilitation therapy effectively improved the cognitive and social functions of individuals with schizophrenia (39). The findings of Sheybani et al. indicated that CBT significantly reduced the negative components of emotion self-regulation, i.e., blaming others, rumination, and catastrophizing, and increased the positive components of emotional regulation, namely, positive attention, positive evaluation, and attention. CBT also was shown to cause the irritability of the sample group to decrease significantly, so it can be concluded that this treatment method can be effective in regulating emotions and reducing the irritability of these patients (40).
5.1. Conclusions
Inhibition and suppression of emotions are among the main causes of pain and various diseases (33), causing psychological distress, so individuals with mental disorders are forced to suppress them due to the reduced ability to identify emotions, thereby increasing subsequent distress, which itself leads to a vicious circle in the patient and his/her attitude toward treatment and disease. It can also be stated that the ability to control psychological pressure in patients with schizophrenia is damaged due to failure to meet their own and others' needs, the feeling of lack of control over life, and excessive distress; therefore, they suppress their emotions more frequently. Finally, it can be stated that CBTs have always been used and effective in treatment, reduction of symptoms, and improvement of emotions and cognitive emotion regulation. In this regard, the results of the present study showed that CBT directly challenged negative thoughts, which could be more effective in using adaptive cognitive emotion regulation strategies.
5.2. Limitations and Suggestions
Some of the limitations of the current research include the self-reporting of the research tool and the lack of a follow-up period. For this reason, and considering that the current research was conducted in a care center for chronic mental patients in the city of Zahedan, it is suggested that the long-term effects of CBT be examined with a follow-up period in future studies. This research should be conducted in other centers, particularly in government hospitals, in the form of a broader demographic study with a larger sample size. Therefore, it is suggested that CBT be taught in counseling centers to reduce the problems of patients with schizophrenia and improve emotional self-regulation.