1. Background
The intensive care unit (ICU) is where the most critically sick patients are cared for and treated by the most skilled nurses, physicians, and other staff in the finest possible circumstances using the most up-to-date and well-equipped equipment (1, 2). According to the statistics of the United States, annually, about 5.6 million individuals are hospitalized in the ICU, with a cost of $7.81 billion (3). This statistic is more than double in developing countries, including Iran. The only cost of antibiotic consumption in ICUs is reported as 3153845 million Rials (4). In 1400, 41360000 Rials were set for the ICU beds. Although patients with various medical diagnoses are admitted to the ICU, respiratory disorders are their most important problem, which requires mechanical ventilation as a supportive treatment (5, 6).
Mechanical ventilation not only has negative effects on different body systems, such as cardiovascular, respiratory, gastrointestinal, musculoskeletal, and other systems (7, 8) but also increases the length of stay in the hospital and the costs of treatment and mortality (2, 9, 10). On the other hand, early extubation and failed re-intubation have many complications, potentially causing airway trauma, aspiration, and acute lung injury (7, 11). The results of some studies show that re-intubation increases the risk of pneumonia by 8 times, the mortality rate by 6 - 12 times, the probability of hospitalization or re-hospitalization in the next 14 days by 31 times, and the costs, compared to the first time. Additionally, problems requiring tracheostomy, pulmonary infections, and lung damage in terms of mechanical ventilation have also been reported (6, 12). According to the articles reviewed in recent years, the average rate of successful intubation is 73.4% (8), and the rate of unsuccessful intubation is 22-4.9% (2, 13). Therefore, one of the most important challenges of the care system in the ICU is the timely and successful extubations of patients (1, 12, 13).
On the other hand, to achieve successful extubation, the process of deciding to remove the endotracheal tube (ETT) at a safe and appropriate time should be diagnosed under the supervision of the treatment team; according to the patient’s symptoms, the doctor orders extubations, and the nurse performs according to her knowledge and experience (14, 15). Delays or mistakes in the decision of each member of the treatment team can lead to inappropriate consequences, such as increasing the duration of mechanical ventilation, costs, and patient death (14, 16). Nurses’ decisions to remove the tracheal tube on time and correctly are associated with positive consequences, such as speeding up the treatment process, which reduces the cost and duration of the patient’s hospitalization (17-19). Nevertheless, the lack of correct and timely decisions by nurses will cause long-term treatment and care (14, 16, 19). According to a study conducted in UK hospitals, 34% of the errors that occur in the patient’s case are due to incorrect decision-making by nurses, which leads to disability or death (18)).
Various factors influence individual and group clinical decision-making (10, 15, 20). Therefore, it is necessary to find effective solutions, including education (11, 20). The results of different studies about the effectiveness of training in clinical decision-making indicated the effectiveness of training and enhancement in clinical decision-making (11, 21). Additionally, some studies emphasized that designing appropriate training programs is necessary to enhance nurses’ decision-making skills and clinical competence (11, 20, 22, 23).
Currently, the interactive educational method is used to improve the knowledge and skills of learners concerning skills that require creativity and critical thinking, in which, more than any other training, learners’ information and experiences are used. In addition, the method will help students to take positive action to protect, enhance, and advocate their own and others’ health, well-being, and safety. The most popular methods are role plays, brainstorming, case-study method, presentations, and discussions. They develop communicative skills, logical thinking, and different types of intellectual activity, such as analysis, synthesis, comparison, and generalization (24, 25).
In order to achieve successful extubations, the interaction and participation of the treatment team are necessary. The results of the studies indicate that the participation of nurses is often neglected (26). Nurses in Iran identified the two main obstacles to participation in the extubations of patients in special departments, including organizational and professional obstacles. Professional obstacles include the lack of ability to exercise professional independence and lack of knowledge. The identified organizational obstacles included role ambiguity, an unsupportive work environment, and a lack of support and encouragement from managers (27, 28). This paper reports the findings of a study that investigated the effects of an interactive training program on critical care nurses’ ability to perform successful extubations. In addition, the opinion of ICU nurses was evaluated regarding the usefulness of the interaction-based training program in improving the extubation care of patients.
2. Objectives
This study aimed to determine the effect of clinical decision-making based on interactive education on the successful extubations of patients in the ICU.
3. Methods
3.1. Design
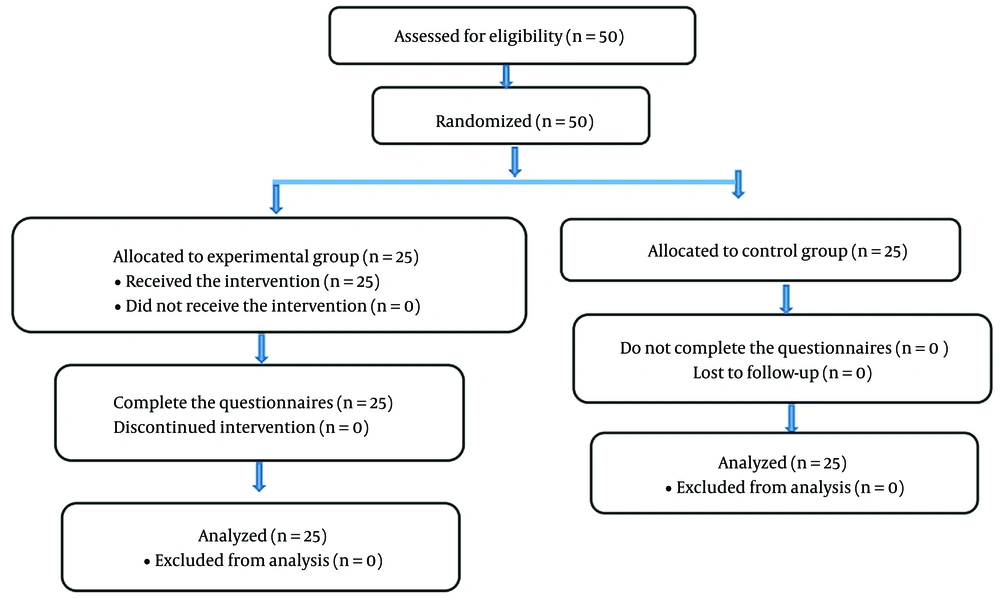
This quasi-experimental study with a pretest-posttest design and a comparison group was conducted on nurses working in Ganjavian Hospital, Dezful, Iran, within August-December 2021.
3.2. Sample
The convenience sampling method was used in this study, and the subjects were divided into two groups by simple random sampling. The sample size based on a study by Mahdiyoun et al. (29) at a 95% confidence level with 90% test power was equal to 21, including 20% drop-out, resulting in 25 in each group with a total of 50. The sample size was calculated based on a statistical formula. After holding training sessions and intervention, 50 individuals participated in all training sessions.
The nurses and physicians, according to inclusion criteria, entered the study from the study population and gave informed consent. The inclusion criteria included employment in the ICU for at least 6 months, a bachelor’s degree or higher, and written consent for cooperation. The exclusion criteria included not attending more than one session in the intervention group, not completing questionnaires, and transferring from the ward or hospital.
3.3. Instruments
The tools used in this study included a demographic information questionnaire, Clinical Decision-Making Questionnaire by Lauri and Salantera (30), and extubation checklist. The demographic information questionnaire, including age, gender, level of education, type of employment, marital status, general work experience as a nurse and work experience in the ICU, and interest in working in the ICU, was completed by all the nurses participating in the project. Lauri and Salantera (30) Clinical Decision-Making Questionnaire has 24 items that measure nurses’ clinical decision-making ability with a positive and negative semantic load on a 5-point Likert scale. The items with a positive semantic load are scored from 5 (always) to 1 (never), and vice versa for items with a negative semantic load. The inverse items of this questionnaire are 1, 3, 5, 7, 9, 11, 13, 15, 17, 19, 21, and 23 (1 = always to 5 = never). Based on extensive research, the tool structure was prepared based on four stages of the decision-making process, including (1) data collection; (2) data analysis and problem statement; (3) problem planning; and (4) project implementation, follow-up, and evaluation. The participants in this study can obtain a score of 24 - 120; a score below 68 indicates systematic analytical decision-making, a score within the range of 68 - 78 indicates the second level of decision-making (i.e., intuitive analysis), and a score above 78 indicates the third level of clinical decision-making (i.e., interpretive intuition). The tool used to categorize nurse decisions follows one of three models, namely analytical, analytical-intuitive, or intuitive. There is analytical and intuitive decision-making on opposite ends of the choice range. Clinical decision-making is divided into two parts, intuitive decision-making, which is based on the senses and information gathered from multiple previous and current sources, and rational decision-making, which is based on the relationship between previous learning and current perceptions about a clinical situation. The analytical process, on the other hand, is a linear approach to deciding on an issue. It is conceivable that throughout the analytical process, a person does not consider his/her own ideas and values while making decisions (30). The validity and reliability of the tool were confirmed, and the internal consistency was reported to be 0.73 (19).
3.4. Intervention
After obtaining the necessary approval from the Ethics Committee and Vice-Chancellor for Research of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran (ref. ID: IR.AJUMS.REC.1399.688), the main researcher (RP) attended the research environment, the ICUs of Ganjavian Hospital. The researcher introduced herself to the hospital officials by presenting a letter of introduction and providing a complete and accurate explanation of the research objectives. Before each intervention, the questionnaire of demographic information and clinical decision-making, the evaluation form of knowledge, and the performance of the samples based on the training workshop were completed for the control and intervention groups.
After completing the questionnaire by the nurses in the control and experimental groups, for the experimental group, interactive training was provided in seven classes, including a researcher, an ICU physician, and five nurses, in five sessions of 2 hours during a month. The time and place of the meeting were determined by the opinion of the group in the training room or based on the case at the patient’s bedside.
The method will be described in this section. After introducing, stating the objective of the classes, and explaining interactive training, the first session was dedicated to clinical decision-making. The second session was for data collection. The third session was for data analysis and problem statements. The fourth session was to plan for problem-solving. The fifth session was to plan, follow up, and evaluate. The participants were asked to bring at least one instance of a successful or failed extubation to the sessions. The participants were then questioned about the right and incorrect instances of care, the researcher and an ICU physician offered training, and the participants submitted their content and justifications to be debated in the group, according to the subject of each session. The topic of each session was summarized at the conclusion. Considering that the sessions were sometimes held at the patient’s bedside, the context was provided for the use of information and experiences of other medical teams, including other physicians, interns, and residents who participated in the discussion and the cases in the ICU. Moreover, direct examination and observation of the patient and the documents in the file, such as tests, medical history, and computed tomography scans, were used. In some cases, nurses expressed their experiences and treatment process to clarify the case and remind colleagues. In some cases, conflicts were raised. Finally, if the explanation was inadequate in the opinion of anyone, the group searched for information from valid sources.
The educational content of the classes was developed via interviews with physicians and nurses working in the ICU based on real rare cases and medical and nursing guidelines and books for the ICU. After 1 month, the questionnaire was again completed by the nurses in the two experimental and control groups at the same time. Moreover, the number of successful and unsuccessful extubations in the experimental and control groups before and after interactive training was recorded according to the extubation checklist based on the assessment of the patient’s physiological parameters, including systolic and diastolic blood pressure, heart rate per minute, respiration rate, temperature, arterial blood oxygen saturation, arterial dioxide pressure, and Glasgow Coma Scale (GCS), the content validity and reliability of which were confirmed by 10 faculty members of the School of Nursing and Midwifery of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran, anesthesiologists and professors of statistics. Programmed extubations of over 18-year-old patients were monitored at least 48 hours after intubation and ventilation, according to the extubations checklist, physiological parameters, and GCS before extubations and 48 hours after ETT removal, first 1 - 2 and 1 - 4 hours, then 2 - 12 hours, and finally 4 - 48 hours. If the patient’s condition was satisfactory and there were no adverse changes in the above-mentioned parameters, the patient was not intubated and did not die, and the extubation was considered successful and otherwise unsuccessful (29, 31).
3.5. Data Analysis
Data analysis was performed using SPSS software (version 24), descriptive statistics (i.e., mean, standard deviation, frequency, and percentage), the independent t-test, the paired t-test, and the chi-square test. In addition, the normality of the data was evaluated using the Kolmogorov-Smirnov test, and the significance level was considered less than 0.05 (Figure 1).
4. Results
According to the study results, most of the participants in this study were female, married, with a bachelor’s degree, contract employment status, and had rotating shifts. Based on statistical results, the two experimental and control groups were not significantly different in terms of demographic information and were homogeneous (P > 0.05) (Table 1).
| Variables and Description | Control Group (n = 21) | Experimental Group (n = 22) | P-Value |
|---|---|---|---|
| Gender | |||
| Female | 18 (83.7) | 22 (100) | |
| Male | 3 (14.3) | 0 (0) | |
| Marital status | |||
| Single | 8 (38.1) | 9 (40.9) | |
| Married | 12 (57.1) | 13 (59.1) | |
| Divorced | 1 (4.8) | 0 (0) | |
| Level of education | |||
| Bachelor | 21 (100) | 21 (95.5) | |
| Master | 0 (0) | 1 (4.5) | |
| Type of employment | |||
| Formal | 4 (19) | 3 (13.6) | |
| Periodical | 6 (28.6) | 6 (27.3) | |
| Contractual | 5 (23.8) | 3 (13.6) | |
| Internship | 6 (28.6) | 10 (45.5) | |
| Position | |||
| Head nurse | 1 (4.8) | 1 (4.5) | |
| Clinical nurse | 20 (95.2) | 21 (95.5) | |
| Work | |||
| Fixed | 1 (4.8) | 1 (4.5) | |
| Shift | 20 (95.2) | 21 (95.5) | |
| Age (y) | 30.19 ± 5.006 | 28.09 ± 4.566 | 0.158 |
| Total work experience (y) | 5.93 ± 4.76 | 4.57 ± 3.75 | 0.303 |
| ICU work experience (y) | 3.50 ± 3.19 | 1.98 ± 2.08 | 0.072 |
Descriptive Results of Demographic Information a
According to Table 2, the mean score of clinical decision-making of the nurses before the educational intervention in the experimental group was less than the control group, although this difference was not statistically significant (P = 0.229). Based on the independent t-test, the mean score of clinical decision-making of the studied nurses after training in the experimental group was higher than the control group, which was statistically significant (P < 0.001). Based on the paired t-test, the mean score of clinical decision-making of the studied nurses in the control and experimental groups increased compared to before the intervention; however, in the control group, this difference was not statistically significant (P = 0.190), and in the experimental group this difference was statistically significant (P < 0.001). The results of Table 3 show that according to the chi-square test, in terms of successful extubations, no statistically significant difference was observed in the control group before and after the intervention (P = 0.744). Therefore, there was a statistically significant difference in the experimental group (P = 0.014).
| Variables | Before | After | P-Value |
|---|---|---|---|
| Control group | 69.57 ± 3.88 | 70.38 ± 2.85 | 0.190 |
| Experimental group | 68.23 ± 3.32 | 75.00 ± 3.30 | < 0.001 |
| P-value | 0.229 | < 0.001 |
Comparison of Clinical Decision-making Scores of Nurses Before and After Intervention in Groups a
| Variables and Description | Before the Intervention | After the Intervention | P-Value |
|---|---|---|---|
| Control group | 0.744 | ||
| Extubations | 20 (100) | 20 (100) | |
| Successful extubations | 12 (60) | 13 (65) | |
| Unsuccessful extubations | 8 (40) | 7 (35) | |
| Experimental group | 0.014 | ||
| Extubations | 19 (100) | 23 (100) | |
| Successful extubations | 10 (52.6) | 20 (87) | |
| Unsuccessful extubations | 9 (47.4) | 3 (13) |
Comparison of Successful Extubations Before and After Intervention in Groups a
5. Discussion
The aim of this study was to determine the effect of clinical decision-making based on interactive education on the successful extubations of patients in the ICU. The results showed that clinical decision-making based on interactive education had a significant effect on the successful extubations of patients in the ICU. One goal of most educational programs for nurses is to enhance both cognitive skills and decision-making abilities. Investigated the kind of decisions nurses can make and what kind they want to make. Many studies have been conducted inside and outside Iran on the effect of appropriate and timely clinical decision-making on the improvement of the patient’s condition in different conditions and departments. The results of a study by Shahraki Moghaddam et al. (28) to teach the Ottawa decision-making framework using the standardized interactive teaching method with and without the patient had a positive effect on the clinical decision-making of working nurses. Additionally, the results of Wahl and Thompson's experimental study to determine the effect of a concept map on the development of critical thinking and clinical decision-making skills of novice nurses indicated the positive role of education in clinical decision-making (31).
Studies conducted in the field of interactive education in different ways regarding other diseases, including the use of electronic education in brain death and organ donation (16), the use of video (17), and the use of the SBAR technique in patient safety training, indicate the effectiveness of this method in nurses’ knowledge and decision-making. Accordingly, intuitive decision-making has been improved and upgraded to the level of analytical decision-making (18). In other words, nurses who use analytical decision-making act faster than other nurses, and analytical decision-making reduces mortality. Despite the effective role of interactive training in the significant increase in decision-making scores and the promising clinical results of the present study, none of the nurses in this study achieved analytical, clinical decision-making after the training, and the nurses’ clinical decision-making remained at the intuitive level (21, 22). The reason for this could be the high volume of work and the special conditions of the epidemic during the corona era, which affected nurses’ job stress and appropriate decision-making (6, 13). The results of this study showed that nurses who have more experience in the ICU have better cooperation with doctors and make effective decisions on time. The results of Doherty-King and Bowers’s qualitative study showed that work experience in the ICU is one of the most effective factors in nurses’ clinical decision-making (11).
The results of the present study showed that interactive training improved clinical decision-making by nurses and increased the number of successful extubations. The results of a systematic review also showed that training leads to appropriate decision-making, which results in the success of timely endotracheal extubation of patients (32). Although the intervention method in these studies differed from the present study, which investigated the effect of interactive training, the consistency of the results can indicate the importance of regular and logical education using any educational method or protocol based on scientific principles that affect personnel performance (33). Considering the confirmation of the research hypothesis that interactive training is effective in clinical decision-making, in the case of intubation of patients in the ICU, this method can be used to train other procedures in order to increase the capability of special department personnel.
5.1. Limitations
Considering the results of the present study on decision-making based on the questionnaire and nurses’ self-report and based on the limited behaviors presented in the questionnaire, it might not be possible to provide a true reflection of nurses’ clinical decision-making ability in different clinical situations. In addition, nurses’ use of some of their learning strategies (e.g., using the positive effect of family presence on the patient’s bedside on increasing the success rate of extubations or physiotherapy by a physiotherapist) was not possible due to COVID-19 conditions and hospital policies, which was beyond the control of the researcher.
5.2. Conclusions
The study results showed that interactive training improved nurses’ clinical decision-making and increased nurses’ involvement with physicians in decision-making for patients’ extubations. Therefore, managers should use this method for in-service training. It is suggested to conduct the present study with a larger sample size and for a longer period and prepare a tool tailored to Iran’s cultural and educational background to measure nurses’ decision-making and clinical performance. In addition, it is suggested that future studies investigate the effect of interactive training on the clinical performance of nurses regarding other special nursing care and the effect of interactive training regarding the presence of family on the agitation of patients under ventilators in special care departments.