1. Background
Migraine is characterized by recurrent moderate to severe debilitating headaches. Migraine Research Foundation declares that migraine headaches are the third most common disease in the world. Despite such a high prevalence, there is limited understanding of its symptoms, causes, and treatment (1), and brain and neurological disorders are among the most common reasons individuals refer to outpatient clinics. It appears due to the dilation of the vessels enclosing the brain and pulsating on one side of the head, accompanied by nausea and vomiting, which might be aggravated by daily activities. Women suffer from migraines three times more often than men. Additionally, women experience longer attacks that are more debilitating (2).
It is known that headache in patients with migraine plays an important role in their quality of life. Accordingly, greater pain intensity leads to a decrease in performance in most components of the mental health scale, including general health, vitality, mental health, and social functioning, and, in general, decreased quality of life in these patients (3). The results of studies show that insomnia is a common symptom in patients with chronic headaches, and sleep complaints are very common among individuals with migraines. Moreover, sleeplessness and oversleeping might also be considered migraine triggers; accordingly, sometimes migraine attacks can be predicted by the length of sleep the night before (4). Sleep is one of the necessities of life, and its deprivation can endanger everyone’s health. It will not be possible to have a good and productive awakening without enough or quality sleep. In order to achieve this goal, it is very important to correctly understand sleep, which occupies about 1.3 of a person’s life (5).
At least over one-third of the adult population suffers from intermittent insomnia; however, 10 - 15% suffer from chronic and persistent sleep problems. Deprivation of sleep or its poor quality causes dysfunctions in the central nervous system. These functions range from the most basic functions, such as appetite regulation and body temperature regulation, to higher-level functions, such as memory and hearing (6). Sleep quality is a complex phenomenon that is difficult to define, and it is subjectively measured (7).
Due to the debilitating nature of migraine, it is very important to treat it and reduce the severity of its symptoms. Drug treatments and different types of psychotherapy are used in this regard. Extensive research shows the effectiveness of psychological treatments in reducing the symptoms of migraine and chronic headaches (8). One of the treatments that has recently received attention is transdiagnostic treatment. This treatment is designed to compensate for the shortcomings of previous treatments and has been relatively successful. Transdiagnostic treatment was developed by Farchione et al. (9). Another treatment that is examined in this study is schema therapy. Schemas are among the basic variables that benefit from high explanatory power because many cognitive processes, coping strategies, and lifestyles of patients are influenced by these basic structures. Schema therapy is a fundamental development in cognitive therapy (10).
Generally speaking, transdiagnostic treatments and schema therapy are considered new and effective treatments for psychological problems and disorders. These two types of third-generation treatments, whose effectiveness has been confirmed in emotional regulation, reducing anxiety, depression, and increasing physical health, can be more economical and effective than traditional cognitive behavioral treatments while being more effective in comorbidity psychological disorders, which are also common in migraine (11), than usual treatments, and this makes the use of non-pharmacological methods in the form of therapeutic supplements more obvious. On the other hand, the use of such strategies enables patients to play an active role in their care and treatment and to effectively control the disease. Due to the importance of recognizing psychological factors as related and effective factors of physical condition and symptoms of migraine and limitations in generalizing the results abroad due to cultural differences, the importance of the current study is felt more than ever.
2. Objectives
According to the materials and studies, this study aimed to compare the effectiveness of transdiagnostic treatment and schema therapy in sleep quality and clinical symptoms of migraine in women with migraine in 2022.
3. Methods
This study is one of the semi-experimental designs with pre-test, mid-test, post-test, and follow-up with a control group. Its statistical population included all women aged 20 to 40 years with migraine diagnosis in Shahrekord, Iran, in 2022. From the women referring to specialized clinics in Shahrekord using the available sampling method and taking into account the inclusion criteria, a total of 45 women were selected as a sample and randomly assigned by lottery to two experimental groups and a control group (15 individuals per group). The inclusion criteria were (1) consent to participate in the study and permission to withdraw at any stage of the research; (2) obtaining a higher than average score in the migraine clinical symptoms questionnaire and sleep quality; (3) minimum diploma literacy to understand the items of the questionnaires; (4) age range of 20 - 40 years; (5) at least 6 months being passed since the diagnosis of migraine; (6) not being in any medical and psychological treatment at the same time; and (7) not suffering from physical and mental diseases that lead to interference with the research variables. Moreover, the exclusion criteria were (1) dissatisfaction with continuing to cooperate in the study; (2) failure to answer all the research questions; and (3) the absence of more than two sessions in treatment sessions. After obtaining the code of ethics (IR.IAU.AHVAZ.REC.1401.103), Approval of the proposal in the Research Council of the Faculty of Human Sciences of Ahvaz Islamic Azad University, and coordination with the clinics of Shahrekord and upon obtaining the sample group and assigning them to 3 groups randomly, the pre-test phase was carried out on all three experimental and control groups before starting the treatment courses. Then, two experimental groups were subjected to the specified treatments, and the control group did not receive any treatment. Then, at the end of the treatment periods, the post-test phase was performed on all three groups.
Two months after the follow-up phase, all three groups were tested again. In order not to violate the rights of the individuals in the control group, after the follow-up phase, intensive treatment courses were implemented for them. Then, the data were collected and prepared for final analysis in SPSS software (version 27). Some of the ethical considerations considered in this study were as follows:
(1) The researcher would explain all the steps of the research honestly and clearly and get the opinion of the candidates to participate in the test.
(2) All individuals participating in this study before answering the questions of the tests would sign a consent form to participate in the study and could withdraw at any stage.
(3) The researcher is committed to keeping all the information of the candidates confidential.
(4) The researcher morally respects each person involved in the research process and avoids discrimination between ethnicities, genders, and social and economic status.
3.1. Data Collection Tools Are as Follows
3.1.1. Ahvaz Migraine Questionnaire
This questionnaire was created and validated by Najarian (12). Najarian used 382 students from Shahid Chamran University and Ahvaz Islamic Azad University, Ahvaz, Iran, to design this questionnaire. Its initial form had 58 items. Its final form, which is used in this study, has 25 items. This self-report questionnaire has one factor, and its answer options include never, rarely, sometimes, and most of the time and it is scored based on values (1), (2), (3), and (4) respectively; therefore, the minimum and maximum scores are 25 and 100, respectively. An example of its items is: “Do you experience worrying mood changes related to your headaches?”. Its concurrent validity with the Hospital Anxiety and Depression Scale (13) and three small clinical scales of hysteric, hypochondriac, and anxiety and depression states of the Minnesota Multiphasic Personality Inventory (MMPI) short form (14) was high and significant. Azizi and Shahbaziyan (15) reported the reliability of this questionnaire using Cronbach’s alpha coefficient of 0.72. The reliability coefficient of this test in the present study was calculated and reported using Cronbach’s alpha of 0.81.
3.1.2. Sleep Quality Scale
This questionnaire was created by Buysse et al. (16) and examines the attitude of individuals regarding the quality of sleep in the last month. This tool has 7 subscales, which are seven scores for the general description scales of the person’s quality of sleep, delay in falling asleep, duration of useful sleep, adequacy of sleep (calculated based on the ratio of the duration of useful sleep to the total time spent in bed), sleep disorders (measured as the person waking up at night), the number of sleeping pills consumed, and morning performance (defined as the problems caused by poor sleep experienced by the person during the day). In scoring this questionnaire, 7 components should be reviewed. The minimum and maximum scores for each component are from 0 (no problem) to 3 (very serious problem). Finally, the scores of each component are added together and converted into a total score (0 to 21). A high score in each component or in the overall score indicates poor sleep quality. Scores 0, 1, 2, and 3 on each scale indicate a normal state and the presence of mild, moderate, and severe problems, respectively. The sum of scores of the seven scales forms the total score, which ranges from 0 to 21. A total score of 6 or more means that the quality of sleep is inappropriate. Buysse et al. (16) reported the reliability and validity of the Pittsburgh Sleep Quality Questionnaire as 0.89 and 0.86, respectively. Furthermore, in Iran, Zargar et al. (17) calculated the validity of this questionnaire as 0.68 by correlating the total score of the questionnaire with a general question that encompasses the content of this questionnaire. Additionally, they calculated the reliability of this questionnaire using Cronbach’s alpha coefficient as 0.74. The reliability coefficient of this test in the present study was calculated using Cronbach’s alpha as 0.79.
3.2. Intervention
In order to carry out the study, the necessary coordination was performed with the Specialized Clinic of Imam Ali in Ahvaz. The implementation method was such that after coordinating with the clinic officials and providing information about the desired sample (e.g., age), the sample group was provided to the researcher. After selecting the sample subjects, the subject, treatment courses, and their goals were explained to the subjects, and they were told that participation in the treatment courses was voluntary and with the consent of the individual, and there was no compulsion to participate in the courses. The content of the interventions is shown in Table 1 and 2.
| Sessions | Description of Sessions |
|---|---|
| First | Establishing a therapeutic relationship, familiarizing the members with each other, increasing motivation, motivational interviewing for patients’ participation and involvement during treatment, providing treatment logic, and determining treatment goals |
| Second | Providing psychological training, recognizing emotions and tracking emotional experiences, and teaching the three-component model of emotional experiences |
| Third | Teaching emotional awareness, learning to observe emotional experiences (emotions and emotional reactions), especially using mindfulness techniques |
| Fourth | Cognitive re-evaluation, building awareness of the effect of mutual communication between thoughts and emotions, identifying inconsistent automatic evaluations, and increasing flexibility in thinking |
| Fifth | Identifying emotion avoidance patterns, getting familiar with different emotion avoidance strategies and their effect on emotional experiences, and finding out about the contradictory effects of emotion avoidance |
| Sixth | Examining behaviors caused by emotions, familiarizing and identifying behaviors caused by emotions and understanding their impact on emotional experiences, and creating alternative action tendencies by confronting behaviors |
| Seventh | Awareness and tolerance of physical feelings, increasing awareness of the role of physical feelings in emotional experiences, performing exposure exercises, and visceral confrontation. |
| Eighth | Coping with situation-based emotion, teaching how to prepare the hierarchy of fear and avoidance, and designing emotional coping exercises |
| Sessions | Objectives and Interventions |
|---|---|
| First | Familiarization and introduction of the program and implementation of the pre-test |
| Second | Definition of schema therapy and familiarity with schema concepts |
| Third | Education and recognition of primary incompatible schemas |
| Fourth | Introduction of the domains of primary incompatible schemas |
| Fifth | Teaching and understanding the concept of cognitive coordination and ineffective coping responses |
| Sixth | Schema therapy evaluation and training stage |
| Seventh | Using cognitive strategies and experimental schema therapy strategies |
| Eighth | Teaching methods of pattern breaking and post-test implementation and summarizing sessions and post-test implementation |
For data analysis, multivariate and univariate covariance analysis and the assumptions of linearity, multiple collinearity, homogeneity of variances, homogeneity of covariances, homogeneity of regression slopes, normality of distribution of variables, and Bonferroni post hoc test were used. SPSS software (version 27) was used to analyze the research data. In addition, the significance level in this study was considered α = 0.05.
4. Results
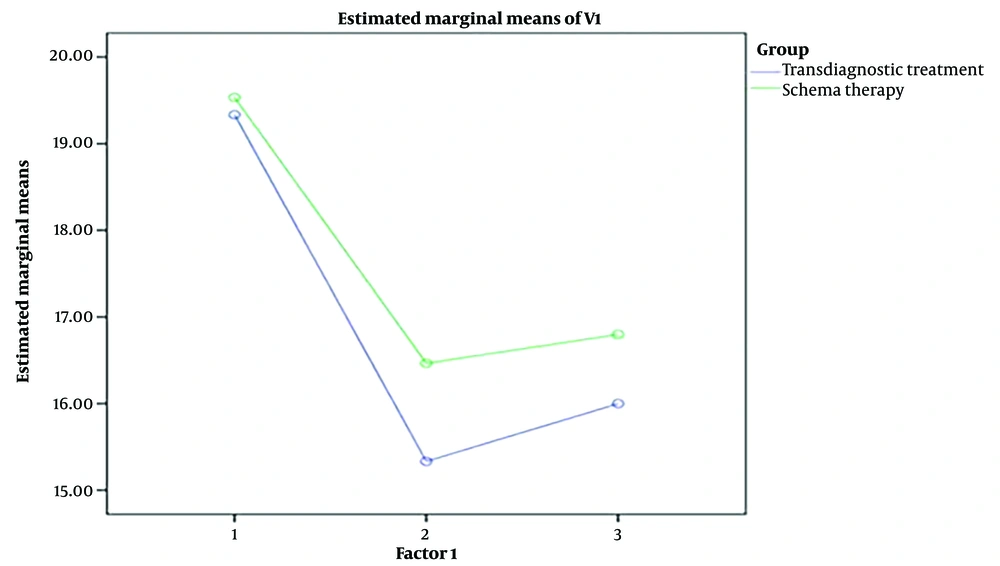
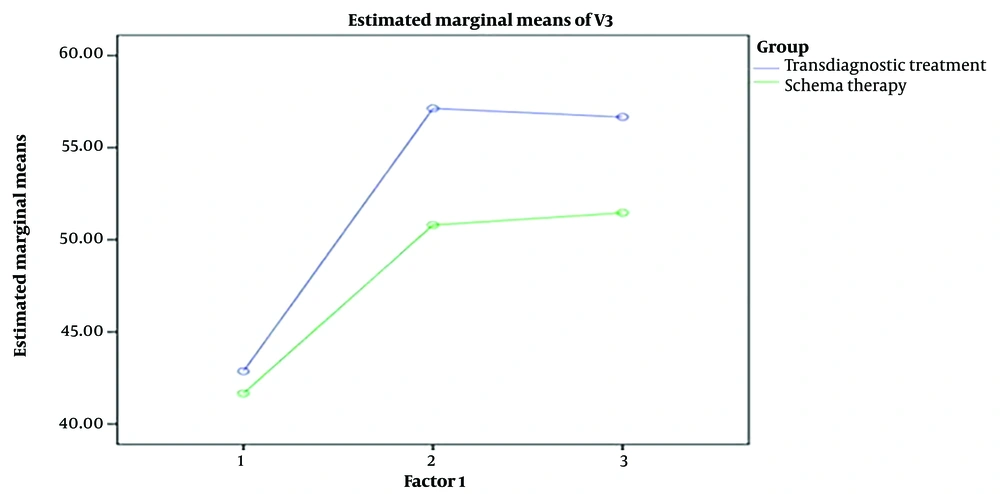
Based on the results listed in the Table 3, it can be described that schema therapy and transdiagnostic treatment increased the quality of sleep of women with migraines. They also reduced the clinical symptoms of migraine in women with migraine.
| Variables and Groups | Mean ± SD | ||
|---|---|---|---|
| Pre-test | Post-test | Follow-up | |
| Sleep quality | |||
| Transdiagnostic treatment | 19.33 ± 2.35 | 15.33 ± 2.29 | 16 ± 1.65 |
| Schema therapy | 19.53 ± 2.17 | 16.47 ± 2.53 | 16.8 ± 2.46 |
| Control | 19.6 ± 1.88 | 19.33 ± 1.95 | 19.47 ± 2.33 |
| Clinical symptoms of migraine | |||
| Transdiagnostic treatment | 42.87 ± 5.9 | 27.13 ± 5.21 | 26.67 ± 5.68 |
| Schema therapy | 41.67 ± 5.64 | 30.8 ± 4.21 | 31.47 ± 4.37 |
| Control | 41.6 ± 4.24 | 39.4 ± 6.97 | 41.13 ± 6.32 |
Abbreviation: SD, standard deviation.
Before performing the repeated measure intergroup analysis of variance, the assumption of normality of the data was performed with the Shapiro-Wilk test. This assumption implied that the observed difference between the distribution of scores of the sample group and the normal distribution in the population was equal to 0. The results of this test showed that all the variables followed the normal distribution in the pre-test, post-test, and follow-up. Additionally, in order to check the assumption of uniformity of covariances or equality of covariances with the total covariance, Mauchly’s sphericity test was used. If the significance in Mauchly’s sphericity test is higher than 0.05, the sphericity assumption test is usually used, and if it is not confirmed, the conservative Greenhouse-Geisser test is used for repeated measure variance analysis. In this study, the results of the Mauchly test of the research variables were not valid (P < 0.05). Therefore, the results of the repeated measures analysis of variance to compare two groups regarding sleep quality variables and clinical symptoms of migraine in the three stages of pre-test, post-test, and follow-up based on Greenhouse-Geisser correction are reported in Table 4.
| Sources and Variables | F | Sig | Eta Coefficient |
|---|---|---|---|
| Within subjects | |||
| Time | |||
| Sleep quality | 59.46 | 0.001 | 0.68 |
| Clinical symptoms of migraine | 0.91 | 0.4 | 0.13 |
| The interaction of time and group | |||
| Sleep quality | 0.98 | 0.33 | 0.23 |
| Clinical symptoms of migraine | 92.39 | 0.001 | 0.77 |
| Between subjects | |||
| Group effect | |||
| Sleep quality | 3.95 | 0.03 | 0.17 |
| Clinical symptoms of migraine | 7.86 | 0.01 | 0.22 |
In Table 4, the results of the analysis of variance with repeated measurements are presented to investigate the intra-test and inter-test effects. According to the results of the F test, the group effect and the time effect were significant for sleep quality variables and migraine clinical symptoms (P < 0.001). There was a difference between the three stages of pre-test, post-test, and follow-up in these variables in the experimental and control groups (P < 0.001). Additionally, the results of Table 4 indicated that there was an interaction between the effect of group and time in sleep quality variables and clinical symptoms of migraine (P < 0.001), which shows the effectiveness of transdiagnostic treatment and schema therapy in sleep quality variables and clinical symptoms of migraine (Figures 1 and 2).
According to the results of Table 4, the F value calculated at the 0.05 level for the clinical symptoms of migraine was significant for the intergroup factor (P < 0.05). As a result, there was a significant difference between the overall mean scores of migraine clinical symptoms and sleep quality in the two groups of transdiagnostic treatment and schema therapy. In general, it can be concluded that the transdiagnostic treatment method had a greater effect on the clinical symptom scores of migraine and sleep quality than on schema therapy.
5. Discussion
The present study aimed to compare the effectiveness of transdiagnostic treatment and schema therapy in sleep quality and clinical symptoms in women with migraines. No study was found to compare the alignment and non-alignment of this study’s results regarding the present hypothesis.
Bullis et al. (20), in their study titled “effectiveness of transdiagnostic treatment on disorders affected by emotion”, conducted on 50 patients with psychosomatic disorders, examined and confirmed the effectiveness of transdiagnostic treatment in reducing the symptoms of emotional disorders. Varkovitzky et al. (21), in their study titled “evaluation of the effectiveness of treatment based on the transdiagnostic approach in improving emotional disorders in trauma patients”, conducted on 30 patients, showed that transdiagnostic treatment improved the emotional disorders of individuals with post-traumatic stress disorder (PTSD). In explaining this finding, it should be said that the transdiagnostic approach, emphasizing the cognitive and behavioral processes of migraine patients, tries to reanalyze the patient’s anxiety control and the response to pain anxiety from a cognitive and emotional point of view and help resolve the patient’s cognitive and behavioral errors (22).
In this regard, avoiding, suppressing emotions, and not accepting them are important criteria for anxiety disorders. Avoidance plays a very important role in emotional disorders both in terms of diagnostic criteria (23) and as a perpetuating factor in pathological conditions (24). Integrated transdiagnostic treatment is designed to target the factors causing emotional distress, and its main emphasis is on control and emotional responses of individuals suffering from emotional distress, including migraine patients. Integrated transdiagnostic treatment uses maladaptive emotional regulation strategies, such as avoidance and suppression and hiding or ignoring emotions. Attempting to control and suppress emotions increases and perpetuates the emotions that a person tries to reduce. Integrated transdiagnostic therapy teaches patients how to face their unpleasant emotions and respond to them more adaptively; that is, it teaches how to rationally evaluate emotional situations for migraine sufferers and, in this way, help regulate their emotions effectively. This reduces the absorption of negative emotions and develops positive emotions (18).
Transdiagnostic treatment is an emotion-based therapeutic approach. Therefore, through some techniques, such as emotional awareness training, re-evaluation of emotions, awareness of the negative effects of avoiding emotions, identifying behaviors caused by emotions, and dealing with emotions based on the situation, it has been possible to reduce negative emotions and cognitive errors that are seen in individuals with migraines. Carlucci et al. (25), In their study, they showed that transdiagnostic intervention is effective for the treatment of negative emotions. Findings show that transdiagnostic group therapy has the potential to help improve mental health outcomes, especially anxiety, and depression.
Sauer-Zavala et al. (26), in their study titled “effectiveness of transdiagnostic treatment in reducing anxiety and improving emotion dysregulation in migraine patients”, showed that transdiagnostic treatment reduced anxiety in migraine patients and improved their emotion regulation. Saariaho et al. (27), in their study entitled “early maladaptive schemas in Finnish adult chronic male and female pain patients”, showed that self-sacrifice schema in women and emotional deprivation schema in the total sample predicted pain disability, as did pain intensity and the number of pain locations. This study suggested that a remarkable number of chronic pain patients might suffer from early maladaptive schemas, which have an effect on their current pain situation and might reflect underlying early emotional maltreatment.
Additionally, the results of this study showed that meta-diagnostic treatment significantly increased sleep quality in the post-test phase. Moreover, according to the logic of the emergence of transdiagnostic treatment, recovery and clinically significant changes in the severity of sleep disorder symptoms of these patients can be due to the targeting of common factors, such as emotion regulation, repetitive thoughts, and negative emotions, which are emphasized in the protocol models. In other words, the reduction in the intensity of the specific symptoms of sleep disorder in migraine patients is probably indirectly due to the changes in common emotional factors; this can be due to the targeting of these common or transdiagnostic factors as the key symptoms of all emotional and sleep disorders through the integration of effective skills and techniques in this protocol.
It can also be said that transdiagnostic treatment is effective in improving the overall quality of sleep and sleep disorders of migraine patients with the help of restriction, mental quality of sleep, delay in falling asleep, sufficient sleep, and useful sleep. An explanatory possibility for the effectiveness of transdiagnostic treatment in reducing the sleep disorders of migraine patients is that it improves the patient’s cognitive errors and appropriate emotional regulation and makes it easier for the patient to fall asleep because, in the problematic beginning of sleep, the patient’s mental and emotional conflicts play an important role. In another explanation, it can be said that another important mechanism in the effect of transdiagnostic treatment on the sleep disorders of migraine patients is based on the awareness of the problem of insomnia and the correction of thoughts by not treating insomnia as a disaster, understanding cognitive errors, and breaking down persistent cognitive factors. The application of homework with therapeutic properties and, ultimately, the hope of recovery lead to the improvement of the sleep quality of migraine patients at the beginning of low sleep tension, proper continuity of sleep, and waking up with a plan and goal.
In explaining the effectiveness of the schema therapy in distress tolerance and sleep quality of migraine sufferers according to Spillman’s model, due to the existence of underlying and perpetuating factors causing primary chronic sleep disorders, some individuals might be highly vulnerable to sleep problems due to having a biological sleep system, which makes them prone to insufficient sleep in the face of stress. In these patients, catastrophic beliefs or self-attributions about pain lead to psychosocial disintegration and affect the quality of a person’s sleep. Johnson et al. (28), in their study entitled “effectiveness of schema therapy on reducing depression caused by illness in patients with chronic pain” in 33 patients with chronic pain, showed that schema therapy was effective in treating depression, and this treatment was known as an antidepressant. Renner et al. (29), in their study entitled “schema therapy for chronic depression: Results of a multiple single case series”, showed that schema therapy might be an effective treatment for patients with chronic depression. Askey-Jones et al. (30), in their study entitled “effectiveness of schema therapy in reducing depression and anxiety in patients with multiple sclerosis (MS)”, concluded on 30 female adult patients with MS concluded that schema therapy could significantly reduce anxiety and depression in MS patients.
Zens (31), in their study entitled “schema therapy for psychosomatic disorders”, showed that schema therapy seems promising for patients with chronic psychosomatic symptoms. Emotional schema therapy techniques with the help of controllability management, empowerment methods based on the psychology of validation, and decision-making techniques based on the psychology of distress intolerance are effective in improving the quality of sleep.
5.1. Study Limitations
Among the limitations of the present study were the short follow-up period and the use of self-report questionnaires. Additionally, the inability to control intervention variables, including demographic variables such as age, gender, economic status, and social welfare level, can be considered one of the major limitations of this study. It is suggested that cognitive behavioral therapy group sessions for migraine patients be held in hospitals, and this program and related techniques help patients’ mental states be taught to nurses and medical staff in the form of knowledge-building workshops. It is also suggested that future studies compare the effectiveness of transdiagnostic treatment with other treatment approaches, including third-wave treatments, such as commitment and acceptance. Finally, it is suggested to perform studies on migraine sufferers from other cities and other chronic patients in the future to generalize the results.
5.2. Conclusions
Migraine is a common, familial disorder characterized by periodic, usually unilateral, often throbbing headaches that begin in childhood, adolescence (often), or early adulthood and become less frequent with age. This debilitating disease, with the severity of clinical symptoms, leads to a decrease in sleep quality in sufferers. This study aimed to compare the effectiveness of transdiagnostic treatment and schema therapy in sleep quality and clinical symptoms in women with migraine, and it was concluded that both transdiagnostic treatment and schema therapy had an effect on reducing clinical symptoms and increasing sleep quality; however, transdiagnostic treatment has a greater effect on migraine clinical symptom scores and sleep quality than the schema therapy. Finally, the results support the effect of transdiagnostic treatment and schema therapy, and paying attention to these two treatment methods is of particular importance for women with migraines. Therefore, the results of this study can become the basis for interventions to help migraine patients.