1. Background
With ever-increasing incidence in developing countries, colorectal cancer is now ranked the third cause of death from cancer worldwide (1). The incidence rate of colorectal cancer is closely correlated with economic development. In fact, it tends to increase constantly as the human development index (HDI) increases in developing countries. This phenomenon can be justified by lifestyle changes, e.g., increased carnivore diets and reduced physical activities, ensuing from socioeconomic development and acting as risk factors in the prevalence of this type of cancer (2)). Despite the high prevalence of colorectal cancer in developed countries, early diagnosis and appropriate treatment can lead to a relatively better prognosis. Surviving a kind of cancer is accompanied by substantial levels of emotional distress (3). The awareness of the risk of death from cancer, the physical impacts of cancer and relevant treatments, and the consequent pressure on personal relationships are all among the stressful factors experienced by a patient that survives cancer. These factors can affect the quality of life (4).
Modern treatments for colorectal cancer allow patients to live longer. However, patients may experience different outcomes from these treatments, such as post-surgery pain, colorectal dysfunction, and body image disorder (5). Body image is considered a major factor in diseases that affect the physical appearance of patients. By definition, body image is an abstract word referring to people’s attitudes toward their bodies viewed as concrete concepts (6). Everyone has a mental image of his/her body, which is the main element of his personality. A body image represents a person’s attitude toward himself/herself, along with the thoughts, beliefs, behaviors, and feelings that can positively or negatively change his/her behavior in various conditions (7, 8). In patients suffering from cancer, body dysmorphic disorder (BDD) is defined as the perceived change in appearance and the consequent dissatisfaction and mental distress. Different types of cancer and relevant treatments are quite devastating, for they can lead to the loss of a body part, lesions, hair loss, dysmorphic features, weight changes, and functional limitations. They can also affect a patient’s self-perception and result in body dysmorphic disorder (BDD) (9). Patients with cancer who need surgery or radiation therapy are more worried about body image than others (10). In addition, worries about body image often lead to poor self-confidence, sexual dysfunction, depression, and social anxiety, problems that can affect the quality of life, personal identity, and personal emotions (11).
Analysis of emotional processing can greatly help perceive the detrimental experience of cancer in people (12). Based on the nature of emotional phenomena and necessary attempts at their expansion, emotional processing can be considered along a continuum ranging from an implicit (or unconscious) level to a specific (conscious) level. The implicit processing of emotions is an automated, procedural, and non-conceptual process that does not need conscious access for execution. Instead, conscious processing needs a declarative assessment and includes higher cognitive sources to define conscious, sensitive states (13). In emotional processing, emotions are experienced, perceived, and expressed actively, intrinsically, and extrinsically (14). Moreover, emotional processing is directly correlated with health improvement in cancer survivors. Two aspects of emotional processing are emotional awareness and acceptance of emotions. Emotional awareness increases when physical feelings or the physically experienced knowledge of unconsciousness can turn into clear thoughts (15). There is a great deal of evidence that emotional processing plays a key role in coping with stress in chronic conditions (13). According to Stanton et al. (16), processing and expressing emotions can improve the adaptability and health of patients with cancer.
Colorectal cancer affects the patient’s mental life due to physical problems and psychological consequences, and even economic problems. Also, throughout the course of the cancer disease, especially during the treatment period, due to the side effects of the drug, there is a possibility of physical changes (3). The changes created can affect the patient’s self-awareness, self-respect, and the patient’s sense of worth and acceptability. The various physical effects of cancer can affect the psychological and social aspects of patients’ lives. In addition to medical and pharmaceutical intervention and support, patients with colorectal cancer also need psychological intervention (4). Psychological techniques can be effective in reducing the physical and medical problems of cancer patients and the complications of its difficult treatments and increasing coping skills with the problems caused by the disease.
Mindfulness-based stress reduction (MBSR) training is among the most widely used and evaluated treatments. In fact, MBSR was primarily designed to help patients with chronic medical conditions reduce stress and enhance their quality of life through concentration, meditation, cognitive rehabilitation, and adaptive learning techniques (17). The results of employing this method proved its effects on the reduction of mental tension and stress correlated with physical symptoms in patients with cancer and other physical diseases (18). In mindfulness training, patients are instructed in formal and informal exercises so that they can participate mentally in ordinary tasks without thinking (19). In this regard, some studies reported the effects of MBSR on the outcomes of cancer (20). According to Wu et al. (21), training an experimental group in MBSR led to a substantial reduction of feelings in response to negative emotional stimuli, reaction time for emotional memory, and duration of the tendency to consider negative emotional stimuli.
Psychodynamic group psychotherapy (PGP) is known as a common treatment for alleviating cognitive distress, enhancing physical performance, and mitigating physical pain in patients with chronic conditions. In this approach, treatment is administered through group discussions (22). The group process should be organized and planned to achieve predetermined objectives in a specific theoretical framework for treatment. The analytical group treatment is aimed at improving interactions between the group members and raising awareness about the group's dynamism and their intrinsic psychological conflicts (23). In this approach, the presence of other members can increase the chance of disclosure and provide an opportunity to observe intrinsic problems (24). According to Pugliese et al. (25), the integrated psychodynamic intervention was efficient in alleviating anxiety and depression in addition to improving interpersonal relationships and self-care of patients with colorectal cancer. Furthermore, Rayska (26) reported that PGP reduced the negative body image of patients with cancer after chemotherapy sessions.
2. Objectives
According to the research literature, few systematic reviews have been conducted on the effects of PGP on body image and emotional processing in patients with colorectal cancer in comparison with MBSR. Considering this research gap and the need to address the psychological aspect of patients with colon cancer, this research seeks to find a scientific answer to the fundamental question, which treatment is more effective in patients with colorectal cancer? Based on the issues outlined in the background, the present study aimed to investigate the effects of PGP and MBSR on body image and emotional processing in patients with colorectal cancer.
3. Methods
This quasi-experimental research adopted a pre-test/post-test control group design with a 45-day follow-up period. The statistical population included all men and women with colorectal cancer visiting Poursina Hakim Health Centers of Isfahan in 2022. The convenience sampling method was adopted to select 42 patients, who were then randomly assigned to two experimental groups of PGP and MBSR and one control group (14 participants per group). G-Power software estimated sample size adequacy with ɑ = 0.05, effect size = 1.18, and power test = 0.90. To randomize the participants, based on the table of random numbers, 28 patients with colorectal cancer were randomly assigned to the experimental group and 14 patients to the control group. Then, the patients in the experimental groups were again randomly divided into PGP and MBSR groups. The inclusion criteria were as follows: having colorectal cancer diagnosed by a specialist, having a medical case at Poursina Hakim Health Center, being aged 18 and older, experiencing the second stage of colorectal cancer and higher, having the minimum literacy of junior high school, giving consent for participation in the research, and participating in the intervention. The exclusion criteria were as follows: having acute physical conditions due to cancer or treatment (e.g., chemotherapy and radiation therapy), having acute psychological disorders causing the inability to respond to questions, and being absent from treatment for more than two sessions. The MBSR group received eight 150-minute in-person sessions per week, whereas the PGP group received fourteen 120-minute in-person two sessions a week. However, the control group did not receive any interventions. Treatment intervention sessions in PGP and MBSR groups were conducted by the first author at Poursina Hakim Health Centers in Isfahan. She had attended specialized courses and workshops on PGP and MBSR interventions. The participants filled out the questionnaires on body image and emotional processing in the pre-test, post-test, and follow-up stages.
3.1. Research Instruments
3.1.1. Multidimensional Body-Self-Relations Questionnaire
The 68-item Multidimensional Body-Self-Relations Questionnaire (MBSRQ) was designed by Cash to evaluate people’s attitudes toward different dimensions of body image structure. This questionnaire includes 10 scales called appearance evaluation, appearance orientation, fitness orientation, health evaluation, health orientation, disease orientation, body areas satisfaction, mental weight, and overweight preoccupation. Each scale is scored from 1 for “completely disagree” to 5 for “completely agree”. Higher scores indicate higher levels of satisfaction with body parts and conditions (27). The validity and reliability of the MBSRQ have been deemed optimal by Shemshadi et al. (28).
Emotional Processing Scale: The 25-item Emotional Processing Scale was introduced by Baker et al. (29). It includes five subscales called suppression, unpleasant emotion experience, emotion control, avoidance, and signs of unprocessed emotions. The questionnaire is scored on a five-point Likert scale ranging from 1 for “completely disagree” to 5 for “completely agree”. The minimum and maximum scores are 25 and 125, respectively. Higher scores indicate lower levels of emotional information processing. The validity and reliability of this scale have been deemed optimal by Kharamin et al. (30).
3.2. Interventions
The PGP sessions were adapted from a study by Rutan et al. (24). The first session included introduction with objectives, rules, treatment period, arrangements, members, and their motivations. The second to fourteen sessions were held to work on the resilience of patients to emotional intimacy with the therapist and other members (e.g., fear of privacy violation) in addition to identifying and clarifying defense mechanisms of patients against avoidance of anxiety and feelings of identification by handling anxiety in patients, regulating anxiety, detecting emotions, and experiencing them in the group. The PGP sessions addressed evaluation of people’s attitudes toward their intrinsic psychological problems, which were the PGP objectives. Finally, the post-test was conducted by reviewing and concluding the results. Moreover, the MBSR intervention was adapted from a protocol presented by Kabat-Zinn (31). Table 1 indicates an overview of MBSR sessions.
| Sessions | Contents |
|---|---|
| 1 | Defining mindfulness; presenting rules; introducing participants; practicing mindfulness eating; conducting a body scan; obtaining feedback; and discussing exercises |
| 2 | Body scan; challenge regarding people’s experiences; standup yoga; mindful sitting (brief) |
| 3 | Mindful stretching; mindful sitting |
| 4 | Reporting the status quo of each participant; mindful sitting; standup yoga; bilateral conversations about unpleasant experiences and then group discussions; sitting and concentrating on respiration |
| 5 | Bilateral conversations, mindful walking, mindful sitting |
| 6 | Mindful sitting; discussing exercises; standup yoga; creating challenges through a few questions; sitting for a few minutes |
| 7 | Mindful stretching; mindful sitting; discussing daily exercises; reminding participants of the end of the intervention; creating challenges through a game |
| 8 | Asking whether this is the final session; sitting briefly; conducting a body scan; creating an environment for reviewing and discussing the intervention; creating challenges through a story; discussing how to employ mindfulness exercises in our lifestyles. |
3.3. Data Analysis
The repeated measures ANOVA were employed for data analysis in SPSS 26.
4. Results
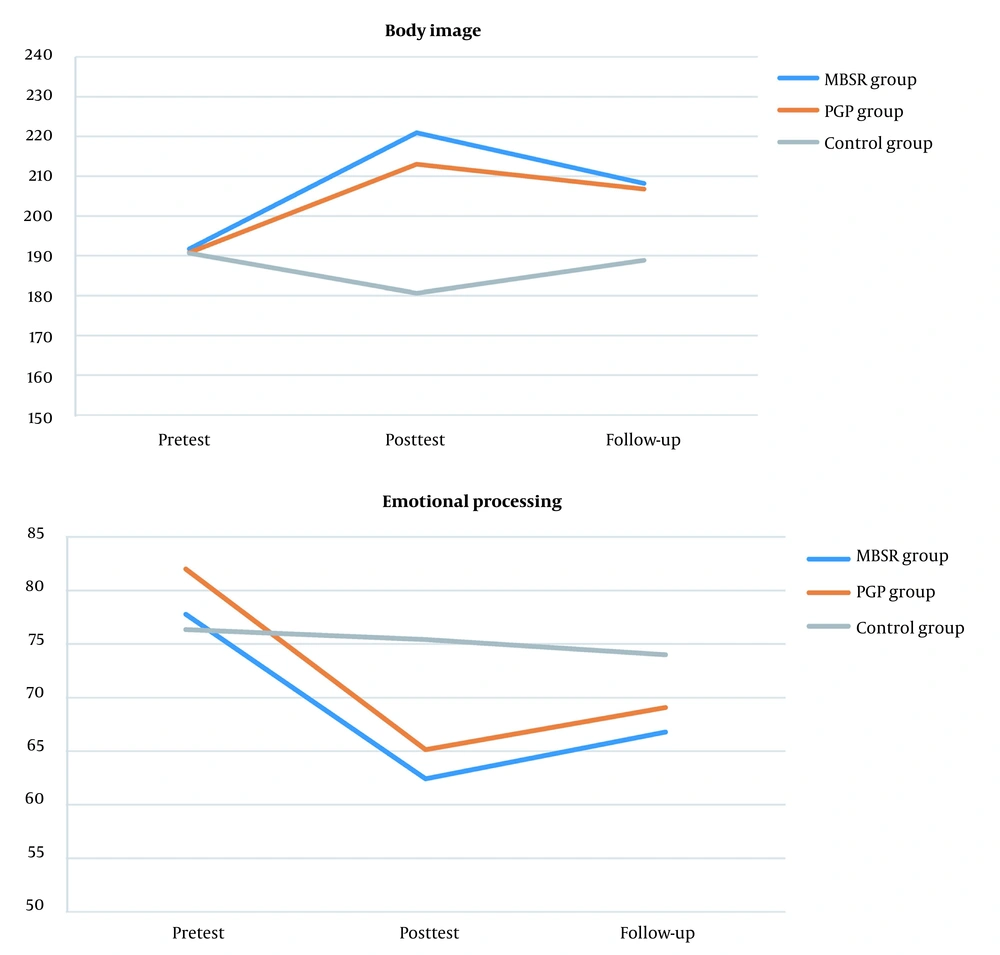
The patients with colorectal cancer were aged 53.64 ± 8.49, 57.07 ± 7.11, and 57.14 ± 8.21 years old on average in control, MBSR, and PGP groups, respectively. Moreover, 33.3% and 66.7% of participants were male and female, respectively. Furthermore, 33.3%, 24.1%, and 42.6% had junior high school, high school, and academic educations. According to Table 2, in the post-test and follow-up stages, there was a significant difference between the experimental and control groups in terms of body image and emotional processing scores in patients with colorectal cancer. The results of descriptive statistics indicated that the mean post-test and follow-up scores of body image increased in both MBSR and PGP groups in comparison to their pre-test scores. However, their mean post-test and follow-up scores of emotional processing decreased (Figure 1).
| Variables and Phases | MBSR Group | PGP Group | Control Group |
|---|---|---|---|
| Body image | |||
| Pre-test | 191.71 ± 23.64 | 190.78 ± 15.53 | 190.64 ± 21.02 |
| Post-test | 220.92 ± 17.49 | 213.00 ± 12.53 | 180.60 ± 9.66 |
| Follow-up | 208.14 ± 16.51 | 206.78 ± 9.95 | 188.85 ± 13.92 |
| Emotional processing | |||
| Pre-test | 77.78 ± 13.49 | 82.00 ± 12.01 | 76.35 ± 9.48 |
| Post-test | 62.42 ± 8.59 | 65.14 ± 10.66 | 75.42 ± 7.40 |
| Follow-up | 66.78 ± 9.33 | 69.07 ± 8.09 | 74.00 ± 9.85 |
Before the mixed ANOVA was conducted, Levene’s test was employed to analyze the presumption of variance homogeneity. Regarding body image (F = 1.63, P = 0.208) and emotional processing (F = 0.83, P = 0.442), the results confirmed the presumption of variance homogeneity in the experimental and the control groups. Moreover, Mauchly’s test of sphericity was conducted before the repeated measures ANOVA was applied to the within-group factor. According to the results, Mauchly’s parameter was not significant in body image and emotional processing, and the sphericity presumption was complied with in those variables.
The ANCOVA was then adopted to analyze the between-group effects by controlling the effect of the pre-test on the post-test and those of follow-up on scores of body image and emotional processing. According to Table 3, there were significant differences in the mean between-group scores of participants in the post-test of body image (F = 30.11, P = 0.001) and emotional processing (F = 7.78, P = 0.001) between the experimental groups and the control group after the pre-test effects were excluded. There were also significant differences in the mean between-group scores of participants in the follow-up of body image (F = 7.60, P = 0.002) and emotional processing (F = 3.35, P = 0.046) between the experimental group and the control group after the pre-test effects were excluded.
| Variables and Phases | SS | df | MS | F | P | η2 |
|---|---|---|---|---|---|---|
| Body image | ||||||
| Post-test | 10424.22 | 2 | 5212.11 | 30.11 | 0.001 | 0.63 |
| Follow-up | 2923.82 | 2 | 1461.91 | 7.60 | 0.002 | 0.30 |
| Emotional processing | ||||||
| Post-test | 1308.44 | 2 | 654.22 | 7.87 | 0.001 | 0.61 |
| Follow-up | 637.09 | 2 | 318.54 | 3.35 | 0.046 | 0.16 |
The repeated measures ANOVA were employed to analyze the within-group effects. With the significant effect of time on body image (F = 8.62, P = 0.001) and emotional processing (F = 16.09, P = 0.001) in groups, the results confirmed that the three measurement attempts were significantly different. The results also confirmed the interactive effect of time on the group with the F-measure calculated for body image (F = 6.17, P = 0.001) and emotional processing (F = 3.14, P = 0.024).
The Bonferroni post hoc test was then adopted to analyze differences between the means of the experimental groups and the control group in a pairwise manner and to determine the effects of both interventions. Table 4 reports the results, according to which there were significant differences between the control group and the experimental group in terms of post-test and follow-up body image scores and the post-test emotional processing scores (P < 0.01). However, the mean scores of experimental groups showed no significant differences in terms of both dependent variables. The results also indicated that there were significant differences between the control group and the MBSR group in the follow-up of emotional processing, whereas there were no significant differences between the control group and the PGP group in terms of their mean scores. According to the results, MBSR and PGP had equal effects on body image improvement and emotional processing enhancement in patients with colorectal cancer.
| Variables | Phases | Groups | Mean Difference | SE | P |
|---|---|---|---|---|---|
| Body image | Post-test | Control - MBSR | -39.97 | 5.29 | 0.001 |
| Control - PGP | -32.16 | 5.60 | 0.001 | ||
| MBSR - PGP | 7.81 | 5.08 | 0.400 | ||
| Follow-up | Control - MBSR | -19.78 | 5.58 | 0.003 | |
| Control - PGP | -19.72 | 5.90 | 0.006 | ||
| MBSR - PGP | 0.05 | 5.36 | 0.999 | ||
| Emotional processing | Post-test | Control - MBSR | 13.92 | 3.66 | 0.002 |
| Control - PGP | 12.02 | 3.88 | 0.011 | ||
| MBSR - PGP | -1.90 | 3.52 | 0.999 | ||
| Follow-up | Control - MBSR | -9.88 | 3.92 | 0.050 | |
| Control - PGP | 8.08 | 4.14 | 0.177 | ||
| MBSR - PGP | -1.74 | 3.76 | 0.999 |
5. Discussion
The present study aimed to investigate the effects of PGP and MBSR on body image and emotional processing in patients with colorectal cancer. The results indicated that both MBSR and PGP had equal effects on body image improvement in patients with colorectal cancer. The effects remained constant over time. Moreover, both interventions enhanced emotional processing in patients with colorectal cancer; however, only the effects of MBSR remained stable over time. This finding is consistent with the research results of previous studies (32-34). Rahmanian et al. (32) reported that mindfulness intervention reduced the emotional processing emotion processing of women with breast cancer. Chang et al. (33) reported that MBSR is a program that can improve mental health, body image, and self-efficacy in women with breast cancer. Straker (34) reported that PGP is effective as an approach to understanding the psychological conflicts and the psychiatric symptoms of patients with cancer.
To explain the findings about the effects of MBSR on improvement in body image and emotional processing, it can be stated that the participants of the MBSR group were asked to observe their streams of consciousness (i.e., feelings, thoughts, and physical senses that are considered potential sources of anxiety in patients with physical diseases) (17). The main mechanism of mindfulness is the self-control of attention. In other words, focusing attention repeatedly on a neutral stimulus like respiration can create an appropriate environment for attention and prevent preoccupation with threatening thoughts and worries about performance in stressful situations. If a patient gains an accurate perception of his/her subjective responses to intrinsic and extrinsic stimuli, he/she will develop insight in order to improve practical capability in the real world and enhance control over stressful situations (21). Therefore, mindfulness can moderate emotions without any judgments and improve awareness about mental and physical feelings in cancerous patients. It can also help patients clearly see and accept emotions, changes, and physical problems during a disease and a treatment process as they occur.
To explain the findings about the effects of PGP on body image and emotional processing, it can be stated that PGP is a notable technique. Emotional expression includes verbalizing, refining, and confessing to stressful or conflicting events. It means talking about and discharging whatever causes emotional or psychological pain. The in-depth emotional experience and its expression can regulate cognitive processes and stimulation by reducing prohibition, thereby leading to a real self-perception and an understanding of personal capabilities (22). By focusing on a patient's defenses that prevent him/her from sensing real feelings and causing emotional closeness due to negative experiences in the past, the PGP encourages him/her to reach a real self-perception. If a patient's real feelings are easily expressed about the past, present, and future, as well as the therapist and the other group members, he/she will be able to identify unconscious factors and the causes of his/her behavior and feeling. This is the point where a patient can start sensing more genuine experiences and emotions in the real world (24). In fact, the PGP helps a patient face devastating extrinsic facts, physical changes, and unpleasant emotions by challenging destructive defenses without employing repressing defensive mechanisms to suppress or ignore real feelings. As a result, patients can accept physical changes, improve regulation, and process emotional information in colorectal cancer.
This study faced a few limitations. For instance, the results pertain to patients with colorectal cancer; hence, generalization of results to other patients should be done carefully. Other limitations of the present study are the parallelism of performing the study with some medicinal measures and the lack of control over the socioeconomic status of the patients.
5.1. Conclusions
According to the results, MBSR and PGP are considered therapies that may improve body image and emotional processing in patients with colorectal cancer. Hence, they can further enhance the well-being and adaptability of patients. It is recommended that MBSR and PGP courses be held at hospitals, clinics, and health centers to improve the adaptability, mental well-being, and emotional well-being of cancerous patients. For generalization of results, it is recommended to conduct similar studies on patients with special diseases and chronic conditions.