1. Background
In December 2019, a disease caused by a virus was discovered in Wuhan, China. This disease, caused by a novel genetically modified virus from the family of coronaviruses named SARS-COV-2, is known as the coronavirus disease 2019 (COVID-19) (1). The outbreak of a global health emergency on January 30, 2020, and a global pandemic on March 11, 2020, were announced by The World Health Organization (WHO) (2). Unfortunately, as it was highly contagious, COVID-19 quickly spread worldwide and infected millions in less than four months (3).
Due to the ability of the pathogen to cause COVID-19, the speed of spreading this infection, and the death rates caused by it, the mental health of healthcare workers was at risk during the pandemic. One of the most common mental and emotional problems in the current situation is anxiety, a vague unpleasant emotional state. Anxiety is described as a natural response to stress, characterized by worry and tension about an uncertain outcome that may interfere with daily and occupational activities (4). People with high levels of anxiety may imagine getting infected with the virus, which may be an important factor in the exacerbation and chronicity of anxiety during the pandemic (5). Addressing the mental and medical conditions of healthcare providers responsible for treating people infected with COVID-19 is necessary for the continuation of efficient medical services (6).
Spiritual health is one of the crucial dimensions of health that some experts believe it requires due attention. The biological, psychological, and social functions can be impaired with poor spiritual health, and the maximum quality of life cannot be obtained (7). Spiritual health generally provides an integrated relationship and harmony between internal forces. It includes the dimensions of stability in life, peace, proportion, harmony, and a sense of closeness and connection with self, God, community, and the environment (8). Spiritual health can be viewed from two perspectives: Religious health, which focuses on how people perceive health in their spiritual life while connecting with a higher power, and existential health, which discusses how people adapt to themselves, society, or the environment (9). In other words, the integrity of an individual can be determined by spiritual health, and it is considered the only force coordinating the physical, mental, and social dimensions. When an individual's spiritual health is seriously compromised, they may suffer from psychiatric disorders, including loneliness, depression, and loss of meaning in life (8).
Spiritual health plays a significant role in the adaptations to stress and positively impacts improving an individual’s mental health and managing psychiatric disorders. Spirituality and religiosity are significantly associated with mental health symptoms, such as depression, increasing self-confidence, and self-control, and are considered common solutions to problems. Believing that God controls situations and watches over the worshippers can significantly reduce anxiety. Most believers believe that controlling the effect of uncontrollable situations is possible by relying on God (10). Several studies have reported an association between spiritual health and anxiety. In their study, Akhlaghifard and Meraji observed a significant negative correlation between spiritual health and COVID-19-related anxiety in nurses and paramedics (11). Masoumy et al. found that the spiritual health of nurses was promoted by reducing occupational stress, which should be considered by nursing managers (12). Given limited studies conducted on the spiritual health and anxiety of nurses caring for patients with COVID-19 and the importance of religious concepts and spirituality in the beliefs of Iranians (13), which has a long history, as well as the undeniable anxiety caused by the pandemic (14), this study aimed to evaluate the association between spiritual health and anxiety of nurses caring for patients with COVID-19.
2. Objectives
This study aimed to evaluate the association between spiritual health and anxiety of nurses caring for patients with COVID-19.
3. Methods
3.1. Study Design and Setting
A descriptive-correlational study was performed on 153 nurses working at the COVID-19 wards in hospitals affiliated with Alborz University of Medical Sciences (Shahid Madani, Shahid Rajaee, Kosar, Imam Ali) during the COVID-19 pandemic in 2021.
3.2. Sample and Process
The Morgan sampling table (15) for a population of 360 showed that 186 samples were enough for this study. A total of 182 subjects viewed the questionnaires, and 153 completed them. To select the samples, a convenience sampling method was used, and based on the study inclusion criteria, all nurses handling COVID-19 patients who agreed to complete the questionnaires were included in the study. The questionnaires were distributed among the nurses electronically and in absentia on the Porsline platform. They were sent to the channels and groups on WhatsApp and Telegram, and the objectives of the research were explained to them. At the same time, they were assured that all their information would remain confidential. The criteria for entering the study included having contact with patients with COVID-19 for at least 6 months, being of both genders working in hospitals affiliated with Alborz University of Medical Sciences, using WhatsApp and Telegram, having proficiency in the Persian language, and providing written informed consent to take part in the study. Exclusion criteria included having psychiatric disorders, neurological disorders, and an ongoing use of anxiolytics.
3.3. Instrument and Data Gathering
The data were collected using the demographic characteristics questionnaire, Beck Anxiety Inventory (BAI), and the Spiritual Well-Being Scale (SWBS) (Paloutzian & Ellison, 1982).
3.3.1. Demographic Questionnaire
The demographic characteristics included age, gender, education, employment status, number of shifts, and work experience in nursing.
3.3.2. Beck Anxiety Inventory
The BAI is a self-report tool used in both the general and patient populations. The total score of the questionnaire (consisting of 21 statements, each of which is scored from 0 to 3) ranges from 0 to 63. The validity and reliability of the Persian version of BAI were 0.72 and 0.83, respectively. The scores for different levels of anxiety were calculated as normal (0 to 7), mild (8 to 15), moderate (16 to 25), and severe (26 to 63) (16).
3.3.3. Spiritual Well-Being Scale
The SWBS consists of 20 items, 10 assessing religious health and the other ten questions evaluating existential health. The score of spiritual health, the sum of these two sub-groups, ranges from 20 to 120. The items are rated on a 6-point Likert scale, ranging from completely disagree to completely agree. In the end, the scores obtained for individuals’ spiritual health are divided into three categories: Low (20 - 40), medium (41 - 99), and high (100 - 120) (17). The scores obtained from each of the religious and existential dimensions are divided into three categories: Low (10 - 20), medium (21 - 49), and high (50 - 60) (13). In questions 3, 4, 7, 8, 10, 11, 14, 15, 17, 19, and 20, I completely disagree, is scored 1, and in questions 1, 2, 5, 6, 9, 12, 13, 16 and 18, I completely disagree, is scored 6. Cronbach's alpha of the original version of the SWBS was 0.91, 0.91, and 0.93 for religious health, existential health, and full scale, respectively. The internal consistency of the Persian version of SWBS was 0.82, 0.87, and 0.90 for religious health, existential health, and the whole scale, respectively (18).
3.4. Ethical Considerations
This study was approved under the ethical approval code of IR.ABZUMS.REC.1399.296 at Alborz University of Medical Sciences.
3.5. Statistical Analysis
After coding, we entered the data into SPSS (IBM, USA) version 26. Descriptive and inferential statistics were employed to analyze the data. In the part of descriptive statistics, the data were summarized using mean and standard deviation and frequency distribution tables (frequency and frequency percentage). In the inferential statistics part, after assessing the normality of the quantitative variables (using the Kolmogorov–Smirnov test), Pearson and Spearman correlations (according to the normality of the variables) and multiple regression were applied to analyze the data. A P-value less than 0.05 was regarded as statistically significant.
4. Results
The study population consisted of 153 nurses working at COVID-19 wards in hospitals affiliated with Alborz University of Medical Sciences during the COVID-19 pandemic, while 139 participants (90.8%) were women, and 14 (9.2%) were men. One-hundred-forty participants (91.5%) had a bachelor's degree, and 13 (8.5%) had a master's degree. Other demographic variables are shown in Table 1.
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 14 (9.2) |
| Female | 139 (90.8) |
| Age (y) | |
| Under 25 | 16 (10.5) |
| 26 – 30 | 57 (37.3) |
| 31 – 35 | 29 (19.0) |
| 36 - 40 | 23 (15.0) |
| Upper 40 | 28 (18.3) |
| Education | |
| Bachelor | 140 (91.5) |
| Master | 13 (8.5) |
| Number of shifts | |
| Single turn | 2 (1.3) |
| Double shift | 3 (2.0) |
| Three turns | 15 (9.8) |
| Employment status | |
| Official | 54 (35.3) |
| Internship | 33 (21.6) |
| Contractual | 28 (18.3) |
| Conventional | 11 (7.2) |
| Corporate force | 27 (17.6) |
| Work experience (y) | |
| Under 5 | 57 (37.3) |
| 5 - 15 | 67 (43.8) |
| 16 - 20 | 17 (11.1) |
| Upper 20 | 12 (7.8) |
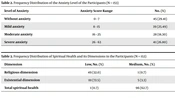
Our results demonstrated that most nurses (54.9%) had no or mild anxiety, 18.3% had moderate anxiety, and 26.8% had severe anxiety (Table 2).
| level of Anxiety | Anxiety Score Range | No. (%) | Mean ± SD |
|---|---|---|---|
| Without anxiety | 0 - 7 | 45 (29.41) | 3.26 ± 2.40 |
| Mild anxiety | 8 - 15 | 39 (25.49) | 11.53 ± 2.45 |
| Moderate anxiety | 16 - 25 | 28 (18.30) | 21.03 ± 2.82 |
| Severe anxiety | 26 - 63 | 41 (26.80) | 35.31 ± 8.18 |
Our results indicated that the spiritual health level of 99.3% of nurses was medium and high, and only 0.7% had poor spiritual health (Table 3).
| Dimension | Low, No. (%) | Medium, No. (%) | High, No. (%) | Mean ± SD |
|---|---|---|---|---|
| Religious dimension | 49 (32.0) | 1 (0.7) | 103 (67.3) | 51.13 ± 8.03 |
| Existential dimension | 111 (72.5) | 5 (3.3) | 37 (24.2) | 42.47 ± 9.97 |
| Total spiritual health | 1 (0.7) | 96 (62.7) | 56 (36.6) | 93.60 ± 16.59 |
The results of Spearman's correlation showed a significant inverse relationship between spiritual health and COVID-19-related anxiety among nurses, indicating that higher scores of spiritual health were associated with lower levels of anxiety (P < 0.001, r = -0.464). The results also demonstrated a significant inverse correlation between the religious dimension of spiritual health and the level of COVID-19-related anxiety among nurses (P < 0.001, r = -0.321). Moreover, Pearson's correlation demonstrated a significant inverse relationship between the existential dimension of spiritual health and the level of COVID-19-related anxiety among nurses (P < 0.001, r = -0.496) (Table 4).
Stepwise multiple regression was used to investigate to what extent spiritual health can predict anxiety scores. The results obtained from multiple regression analysis revealed that the level of anxiety could be predicted by spiritual health and its dimensions (Table 5).
| Anxiety | B | Beta | t | Sig |
|---|---|---|---|---|
| Religious dimension | - 0.605 | - 0.364 | - 4.796 | P < 0.001 |
| Existential dimension | - 0.663 | - 0.494 | - 6.991 | P < 0.001 |
| Total spiritual health | - 0.382 | - 0.473 | - 6.603 | P < 0.001 |
5. Discussion
The present study investigated the association between spiritual health and the anxiety of nurses caring for patients with COVID-19. The results demonstrated that higher scores of spiritual health were associated with lower anxiety levels.
Our findings demonstrated that most participants (54.9%) had mild anxiety, which was consistent with the results of a study by Korkmaz et al.’s, demonstrating that the majority of healthcare workers (67%) were without anxiety or had mild anxiety (19). This finding was consistent with the results of Kaveh et al.’s study, reporting that the majority of healthcare workers in Iran (60.4%) were anxiety-free or had mild anxiety (20). This was contrary to the findings of Icten et al., who reported that all healthcare professionals had moderate (28.90%) and severe (71.10%) anxiety levels (21). A possible explanation for this inconsistency could be the differences in the demographic characteristics of the participants, such as work experience, as well as differences in the sample sizes of the two studies. Moreover, this finding is inconsistent with the study by Zheng et al., showing that the prevalence of anxiety was high among nurses during the outbreak of COVID-19 (22). One potential explanation for this inconsistency could be the variations in the participants' demographic traits, such as education level, as well as in the sample sizes.
The finding of the present study also demonstrated that the spiritual health of 99.3% of the participants was medium and high. Only 0.7% had poor spiritual health, which is in agreement with the results of Jafari et al.’s study, showing that the spiritual health of 100 percent of Iranian nursing students was medium and high, a finding consistent with previous studies (23). This finding was contrary to the results of Gaur and Sharma’s, demonstrating that most participants (72.19%) had poor spiritual health (24). A possible reason for this contrast could be differences in the demographic characteristics of the participants, such as cultural elements.
In explaining these two findings, it can be stated that during the COVID-19 pandemic, a new and sudden situation occurred for people, especially nurses, leading to uncomfortable conditions, anxiety, fear of contracting the disease, and uncertainty. This fear can be due to the survival of oneself and the family, financial problems, loneliness, and isolation, among many other things (25). In this study, most participants (54.9%) were anxiety-free or had mild anxiety, and only 0.7% had poor spiritual health, indicating that spiritual health in stressful conditions and situations can strengthen coping strategies (26). Average spiritual health is acceptable in Iran because of very strong religious beliefs (27). Spiritual health is the central core of human health and deserves special attention (25, 28).
Our findings also indicated that spiritual health and its dimensions were inversely correlated with COVID-19-related anxiety in nurses. This was consistent with the results of Talebi’s study, suggesting that COVID-19 was reduced (29). In their study, Putri et al. examined the association between workplace spirituality and the anxiety of nurses during the COVID-19 pandemic in Indonesia. They demonstrated a significant association between workplace spirituality and the anxiety of nurses during the COVID-19 pandemic, which was in agreement with our study (30). This finding is consistent with Najafi et al.’s results, reporting an inverse correlation between the overall score of spiritual health dimensions and stress, anxiety, and depression (31). This finding was consistent with Rias et al.’s study results, demonstrating that spirituality, knowledge, and attitude toward COVID-19 were negatively associated with COVID-19-related anxiety (32). This finding was consistent with the results of González-Sanguino et al.'s study, investigating anxiety-related factors in Spain and reporting that those with a higher spiritual score showed a lower level of COVID-19-related anxiety (33). This finding was consistent with the results of Akanni et al.'s study, evaluating the association between spirituality and anxiety during the COVID-19 pandemic, which reported a strong correlation between spirituality and anxiety. They emphasized the role of spirituality in reducing anxiety levels (34). However, this was contrary to the Dehghan et al. study, which demonstrated no statistically significant association between COVID-19-related anxiety and spiritual health (35). This finding is not consistent with the results of the study of Prazeres et al., who, contrary to expectations, reported that being religious could not reduce anxiety related to COVID-19, and also there was an inconsistency between being religious and fear of COVID-19 (36). The possible reason for this inconsistency could be differences in the demographic characteristics of the participants, such as age, gender, and cultural factors.
In explaining these findings, it can be stated that people tend to turn to spirituality and religion in times of crisis, and the COVID-19 pandemic is no exception. A 10% increase in prayer searches by 2020, especially in Europe and America, confirms this. The results show that religiosity has increased globally due to the pandemic, with long-term consequences, including various socio-economic consequences (37).
Our findings indicated that levels of anxiety could be predicted by spiritual health and its dimensions, which was in line with the results of Kim et al.’s study, reporting that high levels of family functioning, resilience, and spirituality can be predictive of two to six times less stress, anxiety or depression during COVID-19 pandemic (38). This finding was consistent with the results of the study by Rababa et al., reporting that spiritual health was a significant predictor of the fear of death among the elderly during the COVID-19 pandemic (39). This finding is consistent with the study of Tolentino et al., suggesting that spirituality was the most realistic predictor of chronic and acute anxiety in Brazilian healthcare workers during the outbreak of COVID-19 (40).
This study had some limitations. The questionnaires were completed electronically and remotely, and participants without a smartphone or access to WhatsApp or Telegram could not participate in the research. Another limitation was that the large number of items on the instruments could have exhausted the respondents, and the precision might have been compromised.
5.1. Conclusions
Maintaining good spiritual health can help nurses manage their anxiety. Considering the characteristics of COVID-19 affecting nurses’ mental health, proper measures should be taken by hospital managers and officials to promote nurses’ spiritual health and reduce their anxiety. This can assist health guardians in these difficult conditions in hoping and have a better spirit in this critical situation. Considering the cross-sectional design of the current study, it is recommended that future research should be conducted with longitudinal designs or interventions. Moreover, as this was a quantitative study on spiritual health, future researchers can conduct qualitative research on spirituality in nurses caring for COVID-19 patients.