1. Background
Otitis media with effusion (OME) is a disease in which fluid presents in the middle ear space with no signs of acute inflammation (1). Otitis media with effusion is the most common reason for hearing loss (HL) in the pediatric population in developed countries; more than 70% of children experience OME infection at least once before school age (2). The prevalence of chronic OME remains rather high in middle- and low-income countries, possibly due to poor hygienic conditions, insufficiencies of public health policies, and restricted access to health services (3).
Otitis media with effusion can occur following an upper respiratory infection due to poor eustachian tube (ECT) function or as an inflammatory reaction after acute otitis media (AOM). Otitis media with effusion mainly affects those aged 1 to 5 years (4). The majority of OME episodes recover spontaneously within 3 months; however, nearly 30 - 40% of pediatric patients have repeated OME episodes, and 5 - 10% of episodes last one ear (1).
Persistent middle ear fluid following OME leads to reduced mobility of the tympanic membrane (TM) and seriously influences sound transmission. Chronic OME might be associated with HL or balance disturbances. The HL resulting from OME has been reported to have an impact on a child’s functional listening abilities, auditory perception, behavior, and attention (5-8). This puts children at risk of poor academic performance, language, and speech developmental delay, and reduced cognitive skills (9, 10).
Otitis media with effusion has an obvious effect on a child’s quality of life (QoL), both from direct impacts of persistent middle ear fluid and from a rate of AOM that is up to five times greater than when fluid is absorbed (11, 12). It has been estimated that direct costs associated with otitis media are $3 - 5 billion annually in healthcare expenditure, and the true economic effect is likely greater because indirect costs are considerable yet difficult to estimate (13).
2. Objectives
The high prevalence of OME, along with difficulties in its diagnosis and significant practice variation in its management, makes OME a serious disorder in pediatric population. The present study aimed to determine audiologic findings and the intraoperative and postoperative findings in a large number of children with chronic OME who were candidates for tympanostomy tube placement.
3. Methods
3.1. Study Design
The current project was conducted on children with chronic OME who were candidates for surgical intervention.
3.2. Study Population
Children aged from 8 to 84 months who were diagnosed with chronic OME and scheduled for tympanostomy tube placement were assessed between October 2020 and November 2022. All children were recruited from the Department of Otology, Imam Khomeini Hospital, Ahvaz, Iran. Subjects with a history of otitis externa, TM perforation, previous ear surgery, or ventilation tubes in situ were excluded.
Children who attended the clinic were selected using a consecutive sampling method. A sample size of > 256 subjects was calculated to achieve a power of 80% (Z1-β = 0.84) and a significance level of 5% (Zα/2 = 1.96) for detecting an effect size of 0.28 between pairs.
3.3. Audiologic Assessment
A portable otoscope (Riester-2010, Germany) was utilized to assess the clinical signs of chronic OME. Pure-tone audiometry was conducted on the subjects by a calibrated audiometer (AC40 model, Interacoustics, Denmark). Three pure-tone averages (PTA) at 500, 1000, and 2000 Hz were determined for each participant. Briefly, the PTA values of 0 - 25 dB indicated normal hearing, 26 - 40 dB indicated mild HL, 41 - 55 dB indicated moderate HL, 56 - 70 dB indicated moderate to severe HL, 71 - 90 dB indicated severe HL, and > 90 dB indicated profound HL.
A 226 Hz tympanometer (Titan model, Interacoustics, Denmark) was used to assess middle ear function. Type A tympanogram with peak pressures within + 50 to - 100 daPa and static compliance of 0.23 to 1.5 cc was regarded as the normal value since it is a normal curve where the middle ear space pressure corresponds to the atmospheric pressure and the external auditory meatus. Type C2 tympanogram (admittance peak shifted to - 200 daPa or less) and Type B tympanogram (flattened curve without prominent peak) were considered to be consistent with OME.
3.4. Statistical Analysis
Descriptive data are expressed as frequency (or percentage) for categorical variables and mean ± standard deviation (SD) for numerical variables. The comparisons of demographic and clinical features between participants with/without HL were evaluated using the chi-square test. The paired sample t-test was utilized to compare mean PTA values between pre- and postoperative conditions. The association between gender and age factors was assessed using the chi-square test. A P-value < 0.05 was regarded as a statistically significant level. SPSS software 24.0 (SPSS Co., Chicago, IL, USA) was used for statistical analysis.
4. Results
There were 420 (63.34%) males and 243 (36.66%) females with a M: F ratio of 1.7: 1. The mean age of participants was 45 ± 9.61 months. The most frequent age groups affected by OME were 12 - 36 months (33.48%) and 36 - 72 months (31.67%) (see Table 1). The association between the gender and age of participants was not statistically significant (chi-square test; P > 0.05). The majority of children undergoing myringotomy had persistent effusion for 6 - 12 months (53.39%), followed by those who had it for more than one year (26.70%).
| Variables | Frequency (%) |
|---|---|
| Age (mo) | |
| < 12 | 75 (11.31) |
| 12 - 36 | 222 (33.48) |
| 36 - 72 | 210 (31.67) |
| > 72 | 156 (23.54) |
| Gender | |
| Female | 420 (63.34) |
| Male | 243 (36.66) |
| Duration of symptoms (mo) | |
| < 6 | 132 (19.91) |
| 6 - 12 | 354 (53.39) |
| > 12 | 177 (26.70) |
| Preoperative degree of hearing loss | |
| Mild | 405 (61.08) |
| Moderate | 179 (26.99) |
| Severe | 79 (11.93) |
Demographic Characteristics and Duration of Symptoms in Children with Otitis Media with Effusion (N = 663)
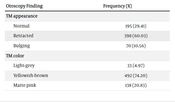
Table 2 results showed that the majority (n = 398, 60.03%) of children indicated retracted TM; nevertheless, 195 children (29.41%) indicated normal TM appearance. The most common TM color was yellowish-brown color (74.20%), followed by matte pink color (20.83%).
| Otoscopy Finding | Frequency (%) |
|---|---|
| TM appearance | |
| Normal | 195 (29.41) |
| Retracted | 398 (60.03) |
| Bulging | 70 (10.56) |
| TM color | |
| Light-grey | 33 (4.97) |
| Yellowish-brown | 492 (74.20) |
| Matte pink | 138 (20.83) |
Frequency of Status and Color of Tympanic Membrane (TM) in Children with Otitis Media with Effusion (N = 663)
According to the obtained data, 489 (73.75%), 139 (20.96%), and 35 (5.27%) children showed Type B, Type C, and Type A tympanograms, respectively. It was also observed that 405 (61.08%) and 179 (26.99%) children exhibited mild and moderate conductive hearing loss (CHL), respectively. Only 79 children (11.93 %) revealed severe CHL (Table 1).
The mean PTA before surgery was 45.23 ± 23.25 dB HL, reduced to 27.83 ± 15.86 dB HL after surgery (the paired sample t-test, P = 0.001). This improvement was about 18 and 17 dB in the right and left ears, respectively. Hearing thresholds returned to normal levels in 487 children (73.45%). However, 19.31% and 7.24% of patients still experienced mild and moderate degrees of CHL 2 months after surgery, respectively.
Table 3 shows the middle ear findings during surgery. It can be seen that the myringotomy site in 408 (61.53%) of the operated children was in the anterior-inferior area. In addition, serous and mucoid secretions were observed in 64.71% and 31.22% of participants, respectively.
| Variables | Frequency (%) |
|---|---|
| Myringotomy site | |
| Anterior-inferior | 408 (61.53) |
| Anterior-superior | 255 (38.47) |
| Middle ear secretion | |
| Serous | 429 (64.71) |
| Mucus | 207 (31.22) |
| Pus | 27 (4.07) |
Middle Ear Findings During Surgery (N = 663)
Table 4 shows postoperative findings in affected patients. In 574 children (86.57%), a ventilation tube was used, and in 89 children, T-tube insertion was performed.
| Variables | Frequency (%) |
|---|---|
| Degree of hearing loss | |
| Normal | 487 (73.45) |
| Mild | 128 (19.31) |
| Moderate | 48 (7.24) |
| Tympanostomy tube | |
| Ventilation tube | 574 (86.57) |
| T-tube | 89 (13.42) |
| Otorrhea | |
| Yes | 69 (10.40) |
| No | 594 (89.60) |
| Time of otorrhea | |
| First week | 12 (17.39) |
| Between 2 - 3 weeks | 45 (65.21) |
| Between 3 - 4 weeks | 6 (8.7) |
| > 4 weeks | 6 (8.7) |
Postoperative Findings in Children with Otitis Media with Effusion (N = 663)
5. Discussion
Otitis media with effusion is the most common bacterial infection in children and the most common indication for antibiotics or surgery (1). The HL resulting from OME might be associated with reduced vocabulary, delayed response to auditory input, and attentional disturbances in children. Otitis media with effusion might also be related to being less capable of independent classroom work and less task-oriented (14).
The effect of chronic OME on health-related QoL might be crucial, influencing children and caregivers (1, 3). It has been shown that 33 - 62% of children with OME suffer from speech and hearing problems, 49% from behavioral problems, and 64% from sleep disturbances (1, 15, 16). Otitis media with effusion can also influence the vestibular (balance) system and gross motor performances, and these defects might be reversible once OME has been treated (17, 18).
Several studies have been conducted to determine the risk factors for OME in children. Respiratory tract infections, craniofacial dysmorphology, nasopharynx obstruction, adenoid hypertrophy, and allergies have been proposed as risk factors for OME (1, 2). Other risk factors suggested are socioeconomic status, race, gender, environment, passive smoking, breastfeeding duration, and gastro-oesophageal reflux (2).
The current study indicated a higher prevalence of OME in males (63.34%) than in females. The aforementioned finding is in agreement with Abdullah et al. (9), Kalpna and Chamyal (19), and Aquino et al.’s (20) results, who also reported the prevalence rates of 72%, 62%, and 66% in male patients, respectively. Gates et al. (21) indicated that in certain racial groups, the prevalence of OME is higher than in others. Differences in OME rates among different ethnic groups might indicate differences in access to socioeconomic status or medical services.
In the current study, the association between gender and children’s age was not statistically significant. However, Restuti et al. (2) reported that the prevalence of OME was less in old children (11 - 13 years) than in younger peers (5 - 7 years). Humaid and Abou-Halawa (22) also demonstrated that the prevalence of OME was significantly greater in young children (6 - 7 years) than in older children (8 - 12 years). In the authors’ opinion, these discrepancies could be attributed to differences in the age of participants. For example, the youngest children in Restuti et al.’s (2) study were 5 years; however, about 60% of the present study’s children were < 5 years.
The most common otoscopy findings were retracted TM and the yellowish-brown color of the TM. It seems that the TM color is less important diagnostically than its mobility and position. Tympanic membrane redness alone does not necessarily indicate OME because crying, cerumen removal with associated irritation of the auditory canal, nose blowing, coughing, and fever result in eardrum redness without a middle ear infection. In a similar study, Sharma et al. (23) demonstrated that 74% of ears with OME exhibited dull and retracted TM, 3% had thin and retracted TM, and 21% of ears exhibited normal TM appearance.
In the present study, 73.75% of patients showed a Type B tympanogram with normal external meatus volume, suggesting a middle ear effusion. Sharma et al. (23) demonstrated that 50.17% and 15.33% of children with chronic OME (n = 300, mean age: 5.96 years) indicated Type B and Type C tympanograms, respectively. Sanli et al. (24) also reported a Type B and a Type C tympanogram in 66.15% and 33.85% of 143 children with chronic OME, respectively.
According to the current study’s data, a large number of patients (61.08%) exhibited mild CHL before surgery. However, 179 (26.99%) and 79 (11.93%) children showed moderate and severe CHL, respectively. Rezaei-Tavirani et al. (25) conducted a meta-analysis study on 51 articles with a sample size of 10,675 patients. They reported that the frequency of mild, moderate, and severe CHL in children with otitis media was 22%, 56%, and 37%, respectively.
When the postoperative audiologic profiles of the patients with OME were compared, hearing thresholds in 487 patients (73.45%) returned to normal limits. However, 19.31% and 7.24% of children still had mild and moderate degrees of CHL, respectively.
According to the current study’s results, otorrhea was observed in 10.40% of patients who underwent tube placement. Ah-Tye et al. (26) reported that otorrhea became increasingly prevalent with increasing the tube tenure duration, and 83.0% of the children with tubes that remained in place for 18 months or more developed at least one episode. Saki et al. (27) reported that transient otorrhea happened in 12.5% and delayed otorrhea in 8.2% of children under 6 years.
In the current study, all children were recruited from a referral hospital in southwest Iran. Therefore, the results might not be generalizable to the whole pediatric population in Iran or other developing countries.
5.1. Conclusions
Otitis media with effusion is one of the leading causes of worldwide healthcare visits, and its complications are critical reasons for preventable HL, especially in developing countries. The degree of HL in OME patients varies from case to case and can fluctuate over time, depending on the amount of fluid present in the middle ear space. Therefore, parents and caregivers should work closely with otologists and audiologists to ensure the best management plan for their child’s individual needs. The most common otoscopy findings were retracted TM and the yellowish-brown color of the TM. Audiologically, the degree of HL before the surgery ranged from mild to severe CHL. After surgery, hearing thresholds in the majority of children returned to normal limits.
The audiologic profile of children with chronic OME is characterized by CHL due to the presence of fluid in the middle ear; however, children might experience more significant HL in higher frequencies.