1. Background
Mood disorders are among the most serious and most important mental diseases, ranging from major depression to bipolar disorder. These are debilitating disorders due to their recurring nature, inevitable complications, and heavy costs (1-3) and affect one in every four persons during their lifetime (1). In a study performed in six European countries, mood disorders were ranked second among debilitating mental diseases. According to DSM-5, mood disorders are divided into two categories: depressive disorders and bipolar disorders. Depressive disorders have the highest prevalence among psychiatric diseases (about 17%), and bipolar disorders have an annual incidence rate of about 1% (3, 4). These disorders are frequently treated with long-term psychotherapy and pharmacotherapy. Pharmacotherapy is the first-line treatment suggested for young patients with bipolar disorders. In this regard, continuous adherence to pharmacotherapy is associated with better psychological health in young patients with bipolar disorder or those suffering from recurrent major depression (5). Therefore, treatment adherence has an essential role in the improvement of such disorders. In addition, treatment adherence can significantly affect patients’ quality of life and social performance, resulting in family stability, satisfaction, and independency (6, 7).
Treatment adherence describes the extent to which a patient follows medical advice and includes behavioral modifications, following a diet, or correcting lifestyle (8). Therefore, treatment adherence is known as the main key to disease management (9). Studies have shown that non-adherence to treatment can result in increased length of hospital stay, rehospitalization, disease exacerbation, and increased care costs. Therefore, a lack of attention to this issue is an obstacle to achieving therapeutic goals (6-8). A report by the World Health Organization (WHO) entitled “adherence to long-term therapies” showed that weak adherence to treatment is one of the causes of adverse clinical outcomes, causing the wastage of health resources and the disruption of the ability of healthcare systems to achieve health goals (10). Although non-adherence to treatment is common in all health disciplines, clinicians dealing with patients suffering from mental disorders face more challenges in this regard (11). Non-adherence to long-term therapies is common among individuals with psychological disorders requiring complex therapeutic regimens (12). Non-adherence to treatment plans and early discontinuation of medications in these patients may lead to complications and, hence, maltreatment of mood disorders (13). Mikaili et al. showed that treatment adherence was low in patients with psychological disorders, and factors, such as patient awareness, could increase the rate of adherence (8). Zeighami et al. stated that about 40% of patients with psychological disorders lacked adherence to treatment (14).
Treatment adherence, especially in clinical psychiatry, is a multi-factorial phenomenon affected by different factors, including patient-centered factors, demographic parameters, therapy-associated determinants, supportive and healthcare system-related factors, the relationship between the patient and the doctor, socioeconomic factors, and social support (8, 15). Studies have highlighted social support as a critical contributor to health outcomes, affirming its association with treatment adherence (16). Providing adequate social support to patients improve their relaxation and motivation to adhere to the therapeutic plan (8). Social support is classified into two categories: Received (or objective) and perceived (or subjective) (17). Perceived (subjective) social support refers to the satisfaction and perception of the individual toward the social support received from others (18). Perceived social support promotes self-care behaviors by the individual; thus, paying attention to the patient’s perception of the social support received may be even more important than the level of the support provided (19). The study by Riahi et al. verified the relationship between perceived social support and mental well-being (20). In another study by Berglund et al., poor emotional and instrumental social support was associated with non-adherence to treatment (16).
Despite the significance of perceived social support and its impact on treatment adherence and functional status in patients with mood disorders, adequate research has not been undertaken in Iran to identify challenges in this area (8).
2. Objectives
This study aimed to evaluate the association between treatment adherence and perceived social support among patients diagnosed with mood disorders. Identifying the factors contributing to this relationship can help health professionals improve the mental health of these patients. Hence, the present study was conducted to determine the level of adherence to treatment and its association with perceived social support in patients with mood disorders in Isfahan, Iran, in 2022.
3. Methods
3.1. Study Design and Setting
This was a cross-sectional correlational study performed on patients with mood disorders referred to the Farabi and Korshid Neuropsychology Hospitals of Isfahan, Iran, in 2022.
3.2. Participants and Eligibility Criteria
The research population included all patients with mood disorders hospitalized in the mentioned hospitals (Farabi and Korshid) in Isfahan (Iran). Inclusion criteria were age ≥ 18 years, established diagnosis of mood disorders (depression or bipolar) by a psychiatrist, and willingness to participate in the study. Patients who refused to participate or did not fill out the questionnaire and those with severe physical problems that would prevent interaction between the researcher and the patient were excluded.
3.3. Sample Size Estimation
We found no previous studies assessing the relationship between adherence to treatment and health literacy in these patients; however, based on a Pearson correlation coefficient of -0.33 between treatment adherence and social support, the sample size was calculated at 54 people using the following formulas. However, the research team enrolled 120 patients with mood disorders to increase the study’s credibility. The participants were selected by the convenience sampling method.
3.4. Sampling Procedure
Sampling was performed by the convenience method. All eligible patients with mood disorders in 2022 entered the study.
3.5. Measures and Outcomes
A three-part questionnaire was applied in this study to measure adherence to treatment and perceived social support in patients with mood disorders. The first part gathered demographic information (age, gender, marital status, and educational level). The second part was derived from the treatment adherence questionnaire developed by Heydari et al., covering three treatment adherence dimensions, including diet adherence (13 items), medication regimen adherence (6 items), and activity pattern (7 items). An overall score of 0 - 33.3 indicated poor adherence; a score of 33.3 - 66.6 indicated moderate adherence, and a score of 66.6 - 100 reflected good adherence. The validity of this questionnaire was assessed by Heydari et al. by calculating its alpha correlation coefficient, which was obtained as 0.86 for diet adherence, 0.91 for medication adherence, and 0.95 for activity pattern (21).
The third part of the questionnaire involved a multidimensional scale for assessing perceived social support. This instrument consisted of 12 items, measuring social support received from three sources, the family (4 items), community (4 items), and friends (4 items), on a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). The minimum and maximum scores of the whole scale were 12 and 84, respectively, a higher score suggesting greater perceived social support. The validity of the multidimensional perceived social support scale was verified using exploratory factor analysis in a study by Besharat. Moreover, Cronbach’s alpha coefficients were determined as 0.91 for the whole scale and 0.87, 0.83, and 0.89 for the sub-scales of family-social support, social support, and friend support, respectively (22).
3.6. Statistical Analysis
The data collected were analyzed in SPSS 16 software at the significance level of P < 0.05 using descriptive indices, Pearson correlation, ANOVA, and independent t-test.
4. Results
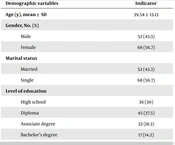
Of the patients studied, 52 were male, and 68 were female, with an overall average age of 39.54 ± 13.13 years. In addition, 52 patients were married (43.3%), and 68 were single (56.7%). Table 1 provides detailed demographic information.
| Demographic Variables | Indicator |
|---|---|
| Age (y) | 39.54 ± 13.13 |
| Gender | |
| Male | 52 (43.3) |
| Female | 68 (56.7) |
| Marital status | |
| Married | 52 (43.3) |
| Single | 68 (56.7) |
| Level of education | |
| High school | 36 (30) |
| Diploma | 45 (37.5) |
| Associate degree | 22 (18.3) |
| Bachelor's degree | 17 (14.2) |
| Employment status | |
| Employed | 11 (9.2) |
| Non-employed | 64 (53.3) |
| Housekeeper | 34 (28.3) |
| Retired | 3 (2.5) |
| Student | 8 (6.7) |
| Source of information | |
| Health care providers | 19 (15.8) |
| Internet | 46 (38.3) |
| TV & radio | 7 (5.8) |
| Friends | 42 (35) |
| Unknown | 6 (5) |
aValues are expressed as Mean ± SD or No. (%).
Pearson correlation indicated a significant association between the treatment adherence level and perceived social support among patients with mood disorders (P < 0.001), indicating that an increase in perceived social support boosted the level of adherence to treatment (Table 2).
| Treatment Adherence | Mean ± SD | Perceived Social Support | Mean ± SD | P-Value a |
|---|---|---|---|---|
| Diet | 29.31 ± 4.99 | Social (important individuals) | 19.74 ± 4.65 | < 0.001* |
| Physical activity | 3.50 ± 2.41 | Familial | 21.48 ± 4.56 | |
| Drug regimen | 18.72 ± 3.91 | Friends | 13.53 ± 6.52 | |
| Total score | 51.53 ± 8.31 | Total score | 54.75 ± 11.23 |
a Pearson's correlation coefficient
Regarding demographic variables, the independent t-test and ANOVA revealed no relationship between the age of patients and their treatment adherence (P = 0.119) and perceived social support (P = 0.081). However, treatment adherence and perceived social support were significantly higher in female patients than in males (P < 0.001). No association was noted between treatment adherence and marital status (P = 0.072); however, the level of perceived social support was significantly higher in married individuals compared to single patients (P = 0.049) (Table 3).
| Variables | Treatment Adherence, Mean ± SD | P-Value | Perceived Social Support, Mean ± SD | P-Value |
|---|---|---|---|---|
| Age (y) | 39.54 ± 13.13 | 0.119 | 39.54 ± 13.13 | 0.081 |
| Gender | < 0.001* | < 0.001* | ||
| Male | 45.17 ± 7.13 | 47.33 ± 8.09 | ||
| Female | 56.40 ± 5.34 | 60.43 ± 9.94 | ||
| Marital status | 0.072 | 0.049* | ||
| Married | 53.10 ± 8.31 | 57.15 ± 11.22 | ||
| Single | 50.34 ± 8.17 | 52.91 ± 10.96 |
We found no significant relationship between the level of education, treatment adherence, and perceived social support. Housewives had significantly higher adherence to treatment compared to students (school/university) and unemployed patients (P < 0.05). Likewise, housewives had significantly higher perceived social support than employed, unemployed, and student (school/university) patients (P < 0.05).
5. Discussion
The present study evaluated the treatment adherence level and its association with perceived social support in patients diagnosed with mood disorder in Isfahan in 2021. Our findings displayed moderate levels of treatment adherence in patients with mood disorders, which was inconsistent with previous studies suggesting low or very low levels of treatment adherence in patients with psychiatric disorders, particularly those suffering from mental disorders, bipolar disorder, and Schizophrenia (6, 8, 14, 23, 24). The observed discrepancy between these results and our observation may be due to differences in the measurement instruments and study populations.
In the current study, the mean score of perceived social support in patients with mood disorders was 54.75 ± 11.23. Despite the lack of adequate studies on perceived social support in patients suffering from mood disorders, it can be stated that the most significant and common sources of perceived social support in patients with chronic conditions (diabetes mellitus, hypertension, and coronary artery diseases) in Iran are spouses, relatives, and friends of the patient (25). In our study, the highest mean score of perceived social support was related to the family dimension. Uygun et al. performed a study on 90 bipolar patients to examine the relationship between perceived social support and psychological resilience and reported the mean score of perceived social support as 54.35 ± 16.09, and the highest mean score was reported for the family dimension (26). Conversely, Kazan Kizilkurt et al. evaluated the effects of perceived social support on improving clinical course and suicidal behavior in 100 bipolar patients. According to their results, patients with bipolar disorder showed higher levels of perceived social support (60.15 ± 15.25), with the family dimension yielding the highest mean score (27). Prabhakaran et al., in India, investigated the association between quality of life and perceived social support among patients with schizophrenia and bipolar disorder during remission and suggested that only 5% of the patients had poor perceived social support (28), which was in contradiction with the present study. This discrepancy between the findings of previous studies and our study can be due to various factors, including differences in the support level provided to patients in various cultural contexts, as well as variations in demographic variables (e.g., occupation, marital status, etc.) and disease stage (remissions, such as Prabhakaran et al.’s study , or active disease). Moreover, given that the family support level is generally desirable in India, it can lead to better treatment outcomes for mental disorders (28).
Based on our findings, there was a significant correlation between the treatment adherence level and perceived social support in patients with mood disorders, where treatment adherence increased with improved perceived social support. In line with our study, Rabinovitch et al. examined the effects of social and family support on medication adherence among 82 patients treated for first-episode psychosis and identified a direct relationship between perceived social support and treatment adherence (29). Uygun et al. noted that perceived social support was correlated with psychological resilience in patients with bipolar disorder (26). The findings of Kazan Kizilkurt et al. also suggested a significant inverse correlation between perceived social support and the duration of untreated period (DUP), suicide attempt, duration of the disorder, and sub-threshold depressive symptoms in patients with bipolar disorder (27). These findings indicate that perceived social support, particularly in the family dimension, may promote treatment adherence among patients with mood disorders.
Our results delineated no relationship between treatment adherence and educational level in patients with mood disorders. However, in Rolnick et al.’s study, a significant direct relationship was found between patients’ adherence to medication regimens and their education level (30). A possible reason for this inconsistency can be due to different studied populations and measurement tools. Our findings revealed no relationship between age and treatment adherence, which agreed with a study by Zeighami et al., who reported no significant association between age and adherence to medications in patients with mental disorders (14). Given the complex interaction between age and patients’ cooperation in treatment (31), more evidence is required to illuminate different aspects of this issue, specifically in patients with mood disorders.
The present study did not show any relationship between age and perceived social support among patients with mood disorders. In corroboration with this finding, Prabhakaran et al. also found no significant association between age and perceived social support in patients with mood disorders (28). Moreover, our results showed no significant difference in the perceived social support of patients based on gender or educational level. In their study, Beyer et al. reported comparable social support scores in patients with mood disorders based on gender, educational level, and age groups (young vs. elderly patients) (32).
5.1. Limitations
The sampling hours coincided with the doctor's visit hours, and the participants were receiving medical treatment at the hospital during that time. Therefore, the research team attempted to adjust the sampling time accordingly.
5.2. Conclusions
Our results suggested a direct and positive association between perceived social support and treatment adherence in patients with mood disorders. However, due to the chronic nature of mood disorders, any inevitable change (such as divorce or loss of loved ones) in the social support received by patients during the lengthy course of treatment, along with other factors, can further influence treatment adherence in these individuals. Moreover, given the paucity of studies on the association between perceived social support and treatment adherence in patients with mood disorders, we could not draw conclusive statements based on comparing our findings in different dimensions with those of previous studies. Thus, further research with larger sample sizes is suggested to more accurately identify the relationship between treatment adherence and perceived social support and the potential confounding factors affecting this association.