1. Background
Chronic low back pain (CLBP) is the most common musculoskeletal disorder of different ages, especially in adults and the elderly (1, 2), and approximately 577 million people worldwide suffer from it. The prevalence of this disorder is reported to be about 80% in studies (1, 3). This disease often starts from the third decade of life and increases until the age of 60 and leads to functional disability (4, 5). In Iran, one third of disabilities in the age group of 16 to 68 years have been observed as a result of this injury (6), which has a bad effect on people's health at some point in their life (7). The disability caused by this disorder leads to an increase in socio-economic burden, increase in costs, physical-psychological problem (8). Despite the use of various methods to reduce pain and functional disability caused by this disorder (9), such as the use of painkillers (10), physiotherapy, exercise (11), periods of absolute rest (12), acupuncture (13), Pilates (14), TENS (15) and even surgery (16), the primary objective of all treatments is to reduce costs and complications. However, a specific superior method has not yet been identified (8). Currently, treatments such as mirror therapy (MT) are recommended as a novel approach that focuses on pain-free movements of the limbs. This method was initially used by Rogers Ramachandran to address phantom limbs and paralysis (17, 18). Mirror therapy stabilizes limb movement and enhances the range of motion by modulating the excitability of the motor cortex (19). It relies on the illusion and mental training of body movements, aiding individuals in visualizing their phantom body in a healthy and reversed state (20). Another mechanism involves the visual nervous system, which stimulates neurons categorized as visual-motor, enabling individuals to acquire new skills through observed movements (20-23). Mirror therapy is a patient-centered approach (20), and in addition to being accessible and simple, it is cost-effective, allowing patients to continue the technique at home once they have learned the procedure (21). Available evidence highlights the effectiveness of this method in improving performance and reducing upper limb pain and false pain in amputees (21, 22).
The primary responsibility of student nurses is to provide care for patients and their families. Despite the prevalence of back pain in different ages and people's acceptance of non-pharmacological and surgical methods, the research conducted on the effect of mirror therapy is limited to the motor organs, especially the upper limbs. A review study revealed a limited number of nursing studies on the application of MT in nursing practice, indicating the interdisciplinary nature of this approach and the need for further research in the field (23). However, nurses have recently started exploring the effectiveness of MT in specific contexts, such as mastectomy patients (24) and the elderly (25). In this study, the impact of MT on the management of lower back pain was investigated, and the results are discussed from the perspective of clinical practice and nursing care. It is worth noting that the implementation of such care patterns in nursing has been limited thus far.
2. Objectives
This study investigated the effect of the MT technique on the nature of pain and movement correction in patients with chronic back pain.
3. Methods
3.1. Study Design
This study was a randomized controlled clinical trial. The intervention group participated in movement correction exercises using mirrors, whereas the control group performed the same exercises without the use of mirrors. This article is a part of a clinical trial (code: IRCT20160726029086N4). The study and all associated procedures received approval from the Faculty of Physiotherapy at Jundishapur University of Medical Sciences, Ahvaz, and were conducted between December 2017 and June 2018.
3.2. Study Population
The research population included all patients with non-specific chronic back pain who were referred using a simple random sampling method. The samples were divided into 2 groups. In this process, the number zero was excluded, and numbers 2 and 1 were assigned to the MT group, while numbers 3 and 4 were assigned to the training group. Number 7 was not assigned to any group. Written informed consent was obtained from each patient.
3.3. Data Collection
The study population was selected based on specific inclusion criteria, which included having non-specific chronic back pain for a minimum of 3 months, being between the ages of 20 and 60, having a minimum pain intensity score of 3 on the Numerical Rating Scale (NRS), and experiencing mild or moderate functional disability based on the Oswestry disability questionnaire. Participants were also required to demonstrate satisfaction with cooperation and provide written informed consent.
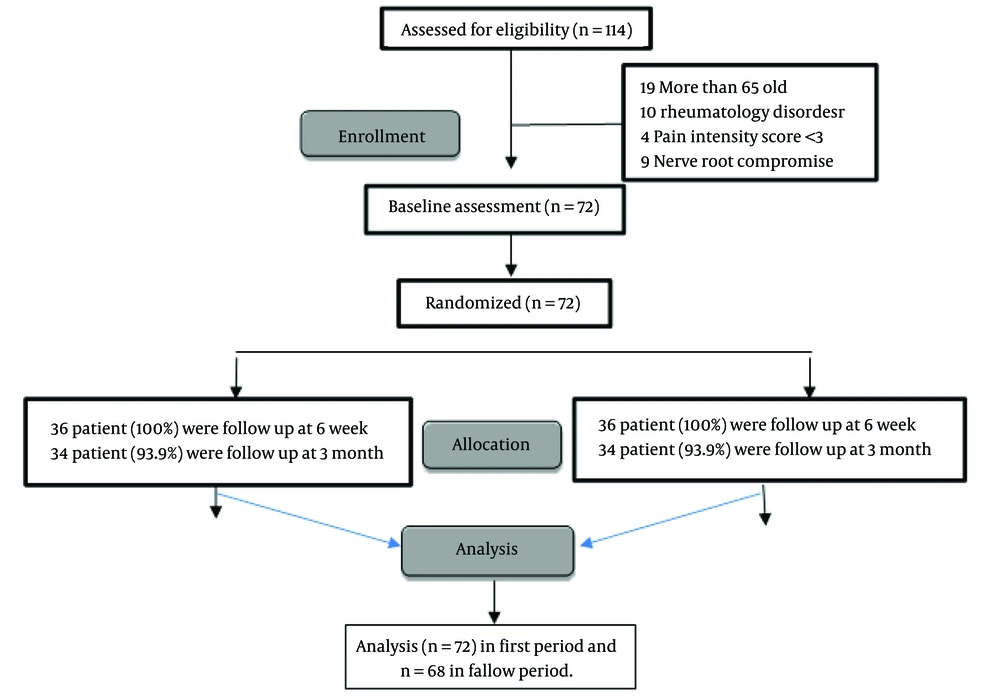
The exclusion criteria included the occurrence of critical conditions if a participant missed 5 out of 30 sessions or if they were absent for 3 consecutive sessions. They were randomly assigned to the 2 study groups, following predetermined, computer-generated randomization sequences prepared by a statistician who was not involved in participant recruitment. The randomization program was accessible only to 2 statisticians and the primary researchers.
According to Samadi et al.'s study (26), the following parameters and the following formula for determining the sample size:
A power of 95% was achieved when 32 patients were allocated to each group. However, to account for a potential dropout rate of 10%, 36 patients were assigned to each group.
3.4. Blinding
Due to the nature of the therapeutic exercises and evaluations, it was not feasible to blind the participants and therapists. The evaluation was conducted in 3 phases: on the day of admission, 6 weeks after discharge from the intervention, and at 3 months of follow-up. All measurements were performed by a trained researcher. The statisticians were unaware of the group assignments until the completion of the data analysis.
3.5. Exercise Protocol
The participants performed each exercise for 30 to 60 min, three times a week, over a duration of 10 weeks. The exercises were conducted under the supervision of trained female and male nurses who received guidance from physiotherapists and occupational therapists. The exercise protocol was the same for both groups, with the only difference being the use of mirrors in the test group. The exercises included: (1) spine stabilization exercise while sitting on the ball, (2) spine stabilization exercise without the ball, and (3) standing spine stabilization exercise (Table 1) (11, 22).
| Duration | Steps of the Education |
|---|---|
| ~ 5 min | (1) Preparation of the environment for MT. Minimize external stimulants (television, noise, etc) as much as possible. If the patient agrees, ask for the collaboration with a relative who can support the patient physically and emotionally. Ensure that the patient is in a comfortable position. Encourage the patient to ask questions and answer all questions carefully. |
| ~ 20 - 30 min | (2) Practical teaching of MT. Evaluate the severity of current pain with 0 to 10 (Numeric Pain Intensity Scale). Explain the basic rules that the patient needs to follow during MT: Eyes should always be focused on the reflection in the mirror. The patient is free to decide which movement he/she will repeat in front of the mirror, and how long he/she will continue with 1 movement. If the patient feels comfortable, repeat only 1 movement; this is also acceptable. Mirror therapy should be practiced every day, at least once a day. It should be underlined that continuation of the therapy is very important to achieve the expected benefits. There is no maximum number of repetitions per day. It is recommended that each MT session should last at least 20 minutes.Watch the patients for 5-10 min and evaluate the application of these rules carefully. |
| ~ 5 min | (3) Ending MT. Evaluate the severity of current pain with 0 to 10 (Numeric Pain Intensity Scale). Answer any questions of the patient and relative. End the training process when the patient is capable of practicing MT alone. |
3.6. Data Collection Tools
Data collection involved the use of a demographic information questionnaire, Oswestry index, and chronic pain questionnaire.
(1) The Oswestry questionnaire, comprising 10 sections with 6 options, was used to assess the severity of disability experienced by patients. It measures the individual's ability to perform daily activities. A disability index of zero indicates good health and the ability to perform activities without pain. Scores ranging from 0 to 20 indicate low disability, 21 to 40 indicate moderate (mild) disability, 41 to 60 indicate high disability, 61 to 80 indicate severe disability, and 81 to 100 indicate extremely severe disability, where the person is unable to perform any activities. The reliability of this questionnaire was reported as 0.85 (26, 27)
(2) The chronic pain questionnaire, consisting of 25 questions, was used to measure pain intensity and its dimensions (physical-sensory, emotional-emotional, and cognitive-evaluative dimensions). Pain intensity scores were categorized as mild (0 - 42), moderate (42 - 62), and severe (above 62). The reliability of this questionnaire is reported as 0.98, which is significant at the level of 95% (26).
(3) Pain intensity was assessed using NRS, which is an 11-point scale ranging from 0 to 10. A score of 0 on the NRS indicates no pain, while a score of 10 indicates unbearable pain. Participants were asked to rate their pain intensity from 1 week before the intervention to the treatment period (26, 27).
3.7. Statistical Analysis
The statistical analysis was performed using SPSS version 22 (SPSS Inc, Chicago, IL, USA). The normal distribution of data was confirmed through the Kolmogorov-Smirnov test. Descriptive data are presented as mean ± SD or as numbers and percentages (%). The independent t-test was used to compare means between samples, while one-way repeated measures MANOVA was used to examine the effects of treatment, time (baseline, post-treatment, and 3-month follow-up), and the interaction between treatment groups and time. The analysis was conducted on an intention-to-treat basis. A CI of 95% was established, and the significance level was set at P ≤ 0.05 (Figure 1).
4. Results
In this study, a total of 72 participants were included in the analysis. The 2 groups were found to be homogeneous. The average age of the participants was 50.5 years, with 70% of the sample being women. The average Body Mass Index (BMI) was 22.5, and the duration of symptoms was 42 months (Table 2).
| Characteristic | Control Group (n = 36) | MT Group (n = 36) |
|---|---|---|
| Age (y) | 51 ± 8.5 | 50 ± 8.9 |
| Gender | ||
| Male | 10 (30) | 12 (32) |
| Female | 26 (70) | 24 (68) |
| BMI | 23.19 ± 2.86 | 22.94 ± 3.88 |
| Current back pain intensity | ||
| Most serious pain in the previous week | 5.55 ± 1.28 | 5.40 ± 1.49 |
| Average pain in the previous week | 3.96 ± 1.14 | 4.02 ± 1.37 |
| Current pain intensity | 2.70 ± 1.57 | 2.72 ± 1.67 |
| Use of medication | 21 (54) | 18 (54) |
| Duration of symptoms (mon) | 37 ± 32.2 | 47 ± 28.6 |
Abbreviation: BMI, Body Mass Index.
a The categorical variables are expressed as No. (%), and the continuous variables are expressed as mean ± SD; P > 0.05.
Table 3 was used to assess pain intensity and the patient's pain status and disability. A significant difference was observed between the groups regarding pain intensity after treatment [CI = 0.4 (-1.7 to 0.8); P < 0.001], and this difference persisted during the follow-up [CI = -0.4 (-1.7 to 0.9); P = 0.003]. There was also a significant difference in chronic pain after treatment [CI = -4.09 (-7.80 to -0.39); P = 0.003], and this difference was maintained at the follow-up [CI = -0.41 (-3.45 to 2.47); P < 0.001]. Additionally, disability remained reduced after treatment [CI = -2.6 (-5.6 to 0.5); P = 0.02], indicating the effectiveness of the intervention (Table 3).
| Outcomes | Control Group (n = 36) | MT Group (n = 36) | Adjusted Between Groups Differences Mean (95% CI) | P-Value | F-Value | P-Value |
|---|---|---|---|---|---|---|
| Pain intensity | < .001 | |||||
| Baseline | 7.9 (1.7) | 7.8 (1.9) | NA | NA | ||
| Post-intervention | 3.8 (2.7) | 4.2 (2.4) | -0.4 (-1.7 to 0.8) | .003 | 12.23 | |
| 3 months | 3.7 (2.7) | 4.1 (2.6) | -0.4 (-1.7 to 0.9) | < .001 | ||
| Chronic pain | < .001 | |||||
| Baseline | 89.17 (12.76) | 92.42 (12.01) | NA | NA | ||
| Post-intervention | 52.05 (8.64) | 42.23 (9.79) | -4.09 (-7.80 to -0.39) | .003 | 5.23 | |
| 3 months | 42.23 (9.79) | 36.13 (7.16) | -0.41 (-3.45 to 2.47) | < .001 | ||
| Disability | ||||||
| Baseline | 13.0 (5.1) | 16.3 (4.8) | ||||
| Post-intervention | 6.1 (5.0) | 8.7 (7.4) | -2.6 (-5.6 to 0.5) | < .001 | ||
| 3 months | 8.4 (7.3) | 7.5 (7.1) | 0.9 (-2.6 to 4.5) | 0.02 |
Abbreviation: MT, mirror therapy.
5. Discussion
The present study is the first clinical trial conducted to investigate the relative effectiveness of two active treatment methods for CLBP patients. In the routine method, corrective movements are performed to improve back pain without a mirror, and in the second method, using mirror therapy. In this study, the two groups of participants (experimental and control groups) were identical in terms of the investigated variables (P > 0.05).
In our study, we observed a significant difference in pain intensity and disability after 6 weeks and 3 months of follow-up. Patients suffering from pain should receive support from multidisciplinary and interdisciplinary health care teams to develop a comprehensive model of care (23). Ashlahatul et al. previously highlighted the positive effects of the MT intervention in improving motor impairment in the elderly (25). Our findings are consistent with other studies that have demonstrated the beneficial effects of MT on pain and function in patients with upper limb dysfunction and phantom pain (27, 28). Louw et al. (29) and Yıldırım et al. (30) found that using MT lead to reduce pain intensity and fear of movement due to pain after four weeks. In studies similar to the present study, the effectiveness of this method in reducing pain and improving organ function has been emphasized. Research evidence shows that a treatment period of at least four weeks can reduces chronic pain, reintegrates the sensorimotor system, reflects the body image and controls the fear of movement, improving the function of organs. This cheap treatment method is safe and easy for the patient (31).
In this sense, the interventions need to be carried out by qualified professionals, which interfere both in the care and in the health of the patient (31, 32). Systematized activities, with good communication and evaluation of the behaviors established to the patient, as well as satisfaction regarding the care, guide improvements and benefits both the team and the patient (32).
5.1. Conclusions
The MT technique, being a therapeutic approach that targets the central nervous system (20), has the potential to improve disability levels and pain intensity in patients with organ dysfunction. However, there is limited information regarding which patients are most likely to benefit from MT and the optimal application of this technique. The findings of this study revealed that MT effectively reduces disability and pain intensity in patients suffering from chronic back pain. Consequently, considering its accessibility, ease of use, and low cost, patients can be trained to perform this technique at home and incorporate it into their routine.
5.2. Limitations
One limitation of this study is that it did not examine other health indicators of the participants.