1. Background
Chronic kidney disease (CKD) is defined by a glomerular filtration rate (GFR) of less than 60 mL/min/1.73 m2, albuminuria of at least 30 mg per 24 hours, or markers of kidney damage (e.g., hematuria or structural abnormalities, such as polycystic or dysplastic kidneys) persisting for more than 3 months (1). A permanent defect in the function or structure of the kidneys is known as end-stage renal disease (ESRD) and requires renal replacement therapies (2). Hemodialysis is a treatment to filter wastes and fluid from the blood, as kidneys did, which is performed on fistula, graft, or catheter forms. Hemodialysis is performed in more than 90% of ESRD patients in the hospital setting (3). Typically, hemodialysis is performed for 3 to 4 hours per week in each session (4).
The incidence of ESRD is increasing substantially; it has increased 10-fold over a short period in the United States (5, 6). Based on the published literature from Iran, the age-adjusted prevalence of CKD is 14.9% in Iran. It has become an important health problem associated with morbidity and mortality and decreased quality of life (7). According to recent evidence, the annual incidence and prevalence of ESRD in Iran were 66 and 169 per million, respectively. Based on the epidemiologic evidence, about 54% of ESRD patients in Iran receive hemodialysis, and the rest undergo a kidney transplant (8). The estimated cost of each hemodialysis session was about 74 US dollars, by which an annual cost of $1,1549 could be estimated for each patient (9). Despite the high cost of treatment, these patients suffer from depression, stress, and familial and personal problems (10).
In the United States, the 1-year and 5-year survival rates of peritoneal dialysis patients are 87% and 35%, respectively, and for hemodialysis patients, they are 79% and 34% (11). In the limited studies in Iran, for example, in the north, the 1-year and 5-year survival rates of hemodialysis patients were 75% and 23%, respectively (12). According to a study conducted in southern provinces, the 1- and 5-year survival rate of hemodialysis patients was 89.2% and 46.8%, respectively (13). The survival rate of patients with vascular access type at hemodialysis was significantly higher than those with vascular access through graft (14). Several factors contribute to high mortality in these patients, including age and sex. Moreover, patients with diabetes mellitus, polycystic kidney disease, hypertension, infections, glomerulonephritis, low body mass index (BMI), levels of serum cholesterol, homocysteine, creatinine, albumin, hemoglobin, history of stroke, dialysis adequacy, and renal replacement therapy had a greater risk of death (15-21). Among all the aforementioned factors, cardiovascular disease is the main cause of mortality in ESRD patients (4).
Although there is growing evidence of hemodialysis patients' survival in developed countries, there is limited evidence in developing countries. Many researchers believe that there is substantial variability in mortality rates of dialysis patients across the world, which is possibly attributable to the variability in the population's background, genetics, and environmental factors (22).
2. Objectives
Therefore, this study aimed to assess the survival rate and associated risk factors in hemodialysis patients from a southwestern region of Iran. Knowing the survival rate and associated risk factors in patients on hemodialysis could help predict and apply solutions for their quality of life and life expectancy. In other words, increasing the quality of life of CKD patients requires knowledge of their survival rate with the current state of service provision, as well as effective factors.
3. Methods
This was a retrospective study of ESRD patients who underwent dialysis therapy at the dialysis department of teaching hospitals affiliated with the Faculty of Medicine at Abadan University of Medical Sciences (AUMS; Khuzestan Province, Iran) from January 2002, who were followed up until December 2017. The study protocol was approved by the Institutional Review Board of AUMS. Renal transplant patients, patients undergoing periodic dialysis, or those who were excluded from the study (due to immigration or reluctance to continue treatment) were considered censorship cases. The survival time of the patients was calculated from the time of dialysis until treatment discontinuation or migration. Overall, 389 patients with hospital records were included. Thirty-three patients did not follow the treatment and dialysis process, and 15 patients migrated during the study. Finally, 341 patients (87.7%) were included throughout the study period.
3.1. Ethical Considerations
This study complied with the Declaration of Helsinki. In all stages of the study, the confidentiality of the identity was guaranteed. The Research Ethics Committee of AUMS (IR.ABADANUMS.REC.1395.181) waived the need to obtain informed patient consent. (https://ethics.research.ac.ir/)
3.2. Data Collection
Data about all ESRD patients who died and were censored from 2002 to 2017 were collected. All the ESRD patients who initiated chronic hemodialysis programs at the dialysis department of the teaching hospitals affiliated with the Faculty of Medicine (AUMS) during 2002-2017 met the inclusion criteria. Patients with acute renal failure, those under treatment with peritoneal dialysis, patients on transient hemodialysis, and those with incomplete medical records were excluded from the study. We started the associations between dialysis modality and mortality risk using more advanced statistical methods besides the conventional methods of survival analysis, i.e., Kaplan–Meier and Cox proportional hazards models, to reduce the influence of selection bias and confounding. Our study considered a cohort of strictly hemodialysis patients, both living and deceased patients, thereby minimizing the potential for survivor bias.
Information, including the patient's demographic and clinical data, was extracted from the hospital records. The time variable was considered from the onset of the first session of the patient's hemodialysis until the patient's death. The demographic data included age, sex, place of residence (city or village), education (illiterate, elementary school, high school, university), history of smoking (at least 2 cigarettes per day, with a history of at least 100 cigarettes per month), and history of drug addiction. Moreover, clinical information, including the blood type and Rh, the onset and stop date of treatment or the date of death, level of hemoglobin, creatinine, and blood urea nitrogen (BUN) before hemodialysis, the number of weekly hemodialysis sessions, vascular access, and associated underlying conditions (such as cardiovascular and renal disease) were collected.
3.3. Statistical Analysis
The continuous variables are reported as mean ± standard deviation (SD) or as medians with total and interquartile ranges (25th-75th percentiles). Categorical variables are expressed as frequencies (percentages). The normality of continuous variables was examined using the Shapiro-Wilk test.
The 1-, 5-, and 10-year survival rates were calculated by the life-table method. Survival curves were generated according to the Kaplan-Meier method. Risk factors predictive of death outcome were first determined by the univariate proportional hazards Cox model. The results were expressed as the crude hazard ratio (HR) and 95% confidence interval (CI). The proportional hazard assumption was checked using the scaled Schoenfeld residuals. Variables with P < 0.15 at the last step were presented for multivariable proportional hazard Cox regression analysis. The adjusted (HR) and 95% CI were calculated in the multivariable model. All data analyses were performed using the Survival package in R statistical software version 3.4.3. P-values less than 0.05 were considered statistically significant. All the tests were two-tailed.
4. Results
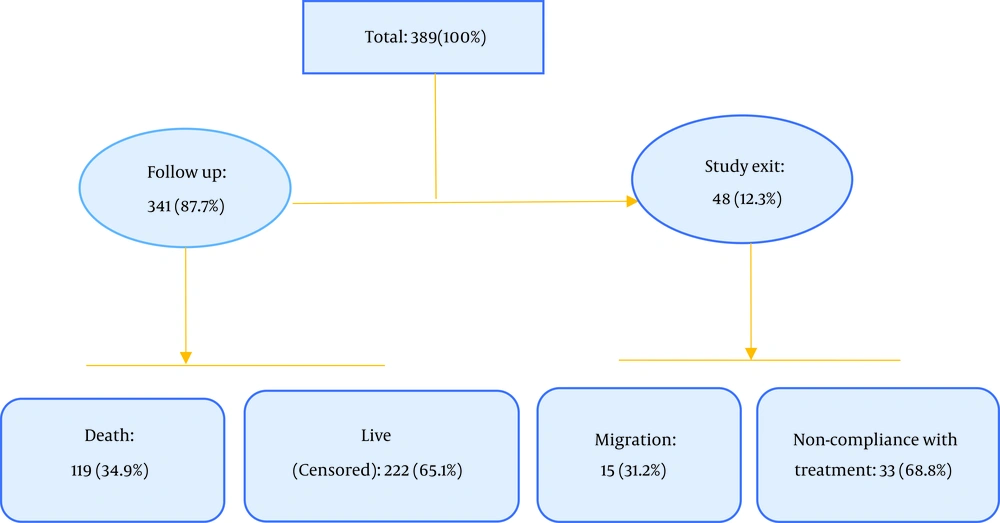
The participants' demographical and clinical information is demonstrated in Tables 1 and 2. Out of 389 patients enrolled in the study, 41 were excluded from the study for a variety of reasons (33 did not follow the treatment and dialysis process, and 15 migrated during the study); finally, 341 patients were present throughout the study period, of whom 119 died during the study (Figure 1).
| Variables | Censored | Dead | Total |
|---|---|---|---|
| Age, y | 56 (44.00 – 66.25) | 62 (23.00 – 92.00) | 59 (47.00 – 68.25) |
| Sex | |||
| Male | 153 (56.7) | 63 (52.9) | 216 (55.5) |
| Female | 117 (43.3) | 56 (47.1) | 173 (44.5) |
| Weight, kg | 64.00 (55.75 – 75.00) | 63.00 (57.00 –71.00) | 63.50 (56.00 – 73.50) |
| Marital status | |||
| Single | 60 (23.1) | 20 (16.9) | 80 (21.2) |
| Married | 200 (76.9) | 98 (83.1) | 298 (78.8) |
| Education | |||
| Illiterate | 142 (54.0) | 87 (73.7) | 229 (60.1) |
| High school | 69 (26.2) | 19 (16.1) | 88 (23.1) |
| Above high school | 52 (19.8) | 12 (10.2) | 64 (16.8) |
| Job | |||
| Unemployed | 156 (61.9) | 65 (56.0) | 221 (60.1) |
| Employed | 96 (38.1) | 51 (44.0) | 147 (39.9) |
| Location | |||
| Urban | 151 (61.9) | 64 (53.8) | 215 (59.2) |
| Rural | 93 (38.1) | 55 (46.2) | 148 (40.8) |
| Smoking | |||
| No | 217 (83.1) | 95 (79.8) | 312 (82.1) |
| Yes | 44 (16.9) | 24 (20.2) | 68 (17.9) |
| Addiction | |||
| No | 254 (98.1) | 115 (96.6) | 369 (97.6) |
| Yes | 5 (1.9) | 4 (3.4) | 9 (2.4) |
Demographic Information of Hemodialysis Patients in the Hospitals of Abadan (2002 - 2017) a
| Variables | Censored | Dead | Total |
|---|---|---|---|
| ESRD cause | |||
| Diabetes | 82 (37.4) | 54 (51.9) | 136 (42.1) |
| Urological problems | 77 (35.2) | 21 (20.2) | 98 (30.3) |
| Polycystic kidney | 7 (3.2) | 4 (3.8) | 11 (3.4) |
| Glomerulonephritis | 21 (9.6) | 11 (10.6) | 32 (9.9) |
| Hypertension | 32 (14.6) | 14 (13.5) | 46 (14.2) |
| Hypertension | |||
| No | 92 (35.0) | 59 (49.6) | 151 (39.5) |
| Yes | 171 (65.0) | 60 (50.4) | 231 (60.5) |
| Dialysis duration, h | 12.00 (9.90 – 12.00) | 12.00 (10.50 – 12.00) | 12.00 (10.50 – 12.00) |
| Vascular access | |||
| Vascular catheter | 73 (27.5) | 32 (26.9) | 105 (27.3) |
| Permanent catheter | 27 (10.2) | 26 (21.8) | 53 (13.8) |
| Fistula | 130 (49.1) | 45 (37.8) | 175 (45.6) |
| Graft | 35 (13.2) | 16 (13.4) | 51 (13.3) |
| Laboratory measures | |||
| Serum creatinine, mg/dL | 10.00 (6.70 – 13.00) | 8.30 (5.80 – 10.90) | 9.25 (6.40 – 12.00) |
| Hemoglobin, g/dL | 10.30 (9.10 – 11.30) | 10.00 (9.30 – 11.00) | 10.15 (9.17 – 11.22) |
| BUN | 50.00 (35.00 – 74.00) | 43.00 (32.00 – 56.20) | 48.00 (35.00 – 69.00) |
| Viral marker | |||
| HIV / HBV / HCV | 15 (5.6) | 5 (4.2) | 20 (5.2) |
| None | 254 (94.4) | 114 (95.8) | 368 (94.8) |
| Blood group | |||
| O+ | 96 (36.6) | 32 (26.9) | 128 (33.6) |
| O- | 14 (5.3) | 9 (7.6) | 23 (6.0) |
| AB- | 10 (3.8) | 5 (4.2) | 15 (3.9) |
| AB+ | 42 (16.0) | 28 (23.5) | 70 (18.4) |
| A- | 5 (1.9) | 5 (4.2) | 10 (2.6) |
| A+ | 48 (18.3) | 29 (24.4) | 77 (20.2) |
| B- | 5 (1.9) | 3 (2.5) | 8 (2.1) |
| B+ | 42 (16.0) | 8 (6.7) | 50 (13.1) |
Clinical Characteristics of Hemodialysis Patients in the Hospitals of Abadan (2002 - 2017) a
Of these, 216 (55.5%) were males and 215 (59.2%) were city-dwellers. Besides, 298 patients (78.8%) were married, and 229 (60.1%) patients were illiterate. The mean, mode, and median of the patients' age were 59, 59, and 57.02 years, respectively.
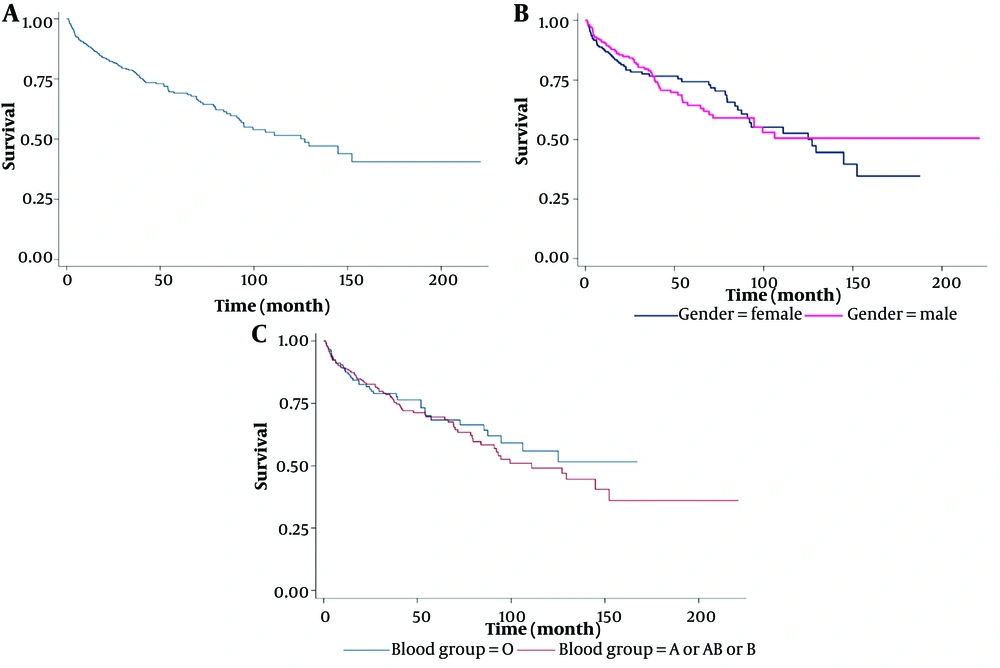
Figure 2A presents the probability of 1-year, 5-year, and 10-year survival rates of patients, which were 0.92, 0.46, and 0.02, respectively. The two sexes had identical survival rates during the first 10 years after the start of renal replacement therapy (Figure 2B). We did not find a significant difference in survival curves based on blood types (Figure 2C).
The univariate effect of various factors on the survival of hemodialysis patients from diagnosis to death is shown in Table 3. We found age, education, residential place, ESRD cause (i.e., urological and urinary problems), dialysis duration, vascular access (i.e., fixed catheter), serum creatinine, and BUN to be significant indicators of HR. For instance, education level was recognized as an effective factor in the survival of dialysis patients; the unadjusted HR among patients who had a higher education was compared with those who were illiterate (0.47 (0.26 - 0.87; P = 0.01).
| Variables | Crude HR (95% CI) | P-value |
|---|---|---|
| Age, y | 1.025 (1.013 – 1.038) | < 0.0001 |
| Sex | ||
| Male | 1.00 | |
| Female | 1.014 (0.707 – 1.456) | 0.940 |
| Weight, kg | 0.997 (0.985 – 1.009) | 0.630 |
| Marital status | ||
| Single | 1.00 | |
| Married | 1.413 (0.873 – 2.286) | 0.159 |
| Education | 0.006 | |
| Illiterate | 1.00 | |
| High school | 0.539 (0.327 - 0.885) | 0.015 |
| Above high-school | 0.477 (0.260 – 0.872) | 0.016 |
| Job | ||
| Unemployed | 1.00 | |
| Employed | 1.141 (0.790 – 1.647) | 0.480 |
| Location | ||
| Urban | 1.00 | |
| Rural | 1.538 (1.071 – 2.208) | 0.020 |
| Smoking | ||
| No | 1.00 | |
| Yes | 0.947(0.604 – 1.483) | 0.810 |
| Addiction | ||
| No | 1.00 | |
| Yes | 1.214 (0.447 – 3.293) | 0.700 |
| ESRD cause | 0.145 | |
| Diabetes | 1.00 | |
| Urological problem | 0.563 (0.340 – 0.933) | 0.026 |
| Polycystic kidney | 0.826 (0.299 – 2.283) | 0.712 |
| Glomerulonephritis | 1.255 (0654 – 2.408) | 0.495 |
| Hypertension | 0.740 (0.411 – 1.334) | 0.317 |
| Hypertension | ||
| No | 1.00 | |
| Yes | 1.35 (1.01 – 1.81) | 0.043 |
| Dialysis duration, h | 0.930 (0.850 – 1.018) | 0.120 |
| Vascular access | < 0.0001 | |
| Fistula | 1.00 | |
| Graft | 1.267 (0.716 – 2.241) | 0.417 |
| Vascular catheter | 1.518 (0.963 – 2.393) | 0.072 |
| Permanent catheter | 2.878 (1.766 – 4.691) | < 0.0001 |
| Laboratory measures | ||
| Serum creatinine, mg/dL | 0.958 (0.922 – 0.994) | 0.024 |
| Hemoglobin, g/dL | 0.951 (0.857 – 1.055) | 0.339 |
| BUN | 0.988 (0.980 – 0.996) | 0.002 |
| Viralmarker | ||
| None | 1.00 | |
| HIV / HBV / HCV | 0.422 (0.171 – 1.038) | 0.060 |
| Blood group | 0.108 | |
| O+ | 1.00 | |
| O- | 1.549 (0.738 – 3.253) | 0.247 |
| AB- | 1.696 (0.660 – 4.358) | 0.273 |
| AB+ | 1.627 (0.979 – 2.705) | 0.060 |
| A- | 1.880 (0.731 – 4.836) | 0.190 |
| A+ | 1.336 (0.807 – 2.211) | 0.260 |
| B- | 2.225 (0.679 – 7.296) | 0.187 |
| B+ | 0.546 (0.252 – 1.186) | 0.127 |
Crude Hazard Ratios for Mortality in Hemodialysis Patients with Associated Variables a
The adjusted HR for significant predictors is depicted in Table 4. For each year of age, the HR in hemodialysis patients increased by 1.02-fold (95% CI, 1.00 - 1.04). We observed that the HR in patients with hypertension was 1.45 (1.29 - 1.65) compared to patients without hypertension. Patients with a vascular accessory of a permanent catheter had a higher adjusted HR compared to patients with a temporary catheter, i.e., 2.806 (1.541 - 5.111).
| Variables | Adjusted HR (95% CI) | P-Value |
|---|---|---|
| Age, y | 1.023 (1.005 – 1.041) | 0.013 |
| Education | 0.896 | |
| Illiterate | 1.00 | |
| High school | 0.899 (0.506 – 1.596) | 0.715 |
| Above high school | 1.064 (0.497 – 2.277) | 0.873 |
| Location | ||
| Urban | 1.00 | |
| Rural | 0.684 (0.441 – 1.061) | 0.090 |
| ESRD cause | 0.702 | |
| Diabetes | 1.00 | |
| Urological and urinary problems | 0.778 (0.435 – 1.390) | 0.396 |
| Polycystic kidney | 0.827 (0.271 – 2.519) | 0.738 |
| Glomerulonephritis | 1.337 (0.646 – 2.767) | 0.433 |
| Hypertension | 1.138 (0.575 – 2.252) | 0.711 |
| Hypertension | ||
| No | 1.00 | |
| Yes | 1.45 (1.29 – 1.65) | <0.0001 |
| Dialysis duration, h | 0.966 (0.831 – 1.123) | 0.654 |
| Vascular access | 0.004 | |
| Fistula | 1.00 | |
| Graft | 1.135 (0.576 – 2.237) | 0.714 |
| Vascular catheter | 1.906 (1.134 – 3.204) | 0.015 |
| Permanent catheter | 2.806 (1.541 – 5.111) | 0.001 |
| Laboratory measures | ||
| Serum creatinine, mg/dL | 0.986 (0.957 – 1.015) | 0.337 |
| BUN | 1.001 (0.991 – 1.010) | 0.910 |
| Blood group | 0.401 | |
| O+ | 1.00 | |
| O- | 1.195 (0.435 – 3.282) | 0.730 |
| AB- | 1.466 (0.539 – 3.989) | 0.453 |
| AB+ | 1.539 (0.854 – 2.774) | 0.152 |
| A- | 0.796 (0.219 – 2.893) | 0.729 |
| A+ | 1.175 (0.668 – 2.067) | 0.576 |
| B- | 1.528 (0.425 – 5.491) | 0.516 |
| B+ | 0.471 (0.184 – 1.205) | 0.116 |
Adjusted Hazard Ratios for Mortality in Hemodialysis Patients with Associated a
5. Discussion
This retrospective cohort study was conducted among 389 hemodialysis patients living in the south of Khuzestan Province (2002 - 2017) and aimed to assess the survival rate and factors affecting the mortality of these patients. Most of the patients were male, married, and lived in cities. The most common cause of ESRD was urinary tract problems and discomfort. The most important factors that significantly affected the mortality rate of hemodialysis patients included older age, permanent catheters, and a history of hypertension. The probabilities of 1-, 5-, and 10-year survival were 0.92, 0.46, and 0.02, respectively. In line with our results, several studies have considered the role of vascular access in the survival of hemodialysis patients. In a study in the United States, vascular access by permanent catheter increases the adjusted HR by 1.49-fold in comparison with a vascular catheter (5). Another study in the United States suggests that changing the vascular access method from temporary to permanent catheters also greatly increases the risk of death (3).
Although we did not find BUN to be a significant predictor of HR, the literature indicates that the role of BUN in patients with dialysis is considerable (23-27). A study in the US suggests that the risk of death in dialysis patients with high BUN was much higher than that of other patients. These researchers claimed that the survival rate was slightly lower for patients who started dialysis at higher BUN concentrations (28). In a study by Tanaka et al., every 1 unit of increase in the blood urea nitrogen to creatinine ratio (UCR) level was significantly associated with an increased risk for all-cause mortality (HR 1.07; 95% CI 1.03 - 1.12) (29). Blood urea nitrogen is also used to evaluate kidney function, and an increase in BUN level is often, but not always, the outcome of a reduction in GFR. Some factors increase the production of urea, such as gastrointestinal bleeding, corticosteroids, and high protein diets, and checking the BUN level is an important factor in evaluating renal function (30). A recent study also found that increased BUN levels increased the risk of death in hemodialysis patients.
The present study's univariate analysis showed that the survival rate of hemodialysis patients who lived in rural areas was lower than that of patients living in the city. However, this association vanished in the multivariate analysis. The increased risk of death in these patients could be due to their inadequate, inconvenient, or inappropriate access to treatment centers and, consequently, their poor compliance with the dialysis process and treatment.
A study in an Eastern European country estimated the probability of a 5-year survival rate at 62.8% (31). The difference in survival rates between the cited study and the present study was very high. In the study of Khazaei et al. in the central part of Iran, the probability of the 5-year survival was 40% (32). The estimation of the mentioned study was very close to the survival rate in the present study. The similarity of survival probability in the present study with studies conducted in Iran, as well as its significant difference with studies conducted in developed countries, may be evidence of the need for appropriate healthcare and the high costs of dialysis-related healthcare services in Iran compared to developed countries.
5.1. Limitations and Prospect
Since this study was retrospective (looking back on or dealing with past events), some information was extracted based on the patients' statements and self-report (e.g., addiction, smoking); thus, it may have led to bias. The number of patients was also inadequate and relatively small for clinical and laboratory records. It is possible to resolve these problems by carrying out a prospective study.
5.2. Conclusions
Our study explored the mortality and associated risk factors in Iranian dialysis patients
from the Southwestern region. We found that the cumulative hazard of mortality was significantly higher in hemodialysis patients than in those with other types of renal failure after adjusting for various confounders. Further studies are necessary to devise preventive and national strategies for hemodialysis patients.