1. Background
Bipolar II disorder (BD-II) is one of the most debilitating brain disorders and a chronic mental illness characterized by recurrent episodes of depression, mania, and hypomania (1). Major symptoms of BD include emotional instability, irritability, impulsivity, disturbed interpersonal relationships, poor performance, cognitive impairment, psychotic symptoms, decreased quality of life, and rising suicide rates (2). Emotional disorders, such as psychological distress, are quite common among bipolar patients (3). Psychological distress is a mental health indicator that includes a set of psychological, physiological, and behavioral symptoms, such as anxiety, depression, agitation, and decreased cognitive functioning, characterized by negative, exhausting, irritating, and distressing feelings (4, 5). Psychological distress is a special discomfort and emotional state that individuals experience temporarily or permanently in response to harmful tensions and experiences, and negatively affects their social functioning and daily lives (6, 7). Instead of expressing their feelings when facing stressful situations, individuals with low levels of psychological distress tolerance usually display avoidance behaviors (8).
Cognitive-behavioral avoidance, another common problem faced by bipolar patients (9), is a defective cognitive, affective, and behavioral system that reinforces the underlying factors of worry and stress and sets the stage for the initiation, exacerbation, and continuation of anxiety disorders (9, 10). Mesri et al. (11) reported that cognitive avoidance entails different strategies, such as distraction, worry, and thought suppression, that patients with panic disorder and agoraphobia adopt to avoid facing negative thoughts and unwanted problems. Behavioral avoidance, on the other hand, refers to the process of avoiding or abandoning an action, person, or object to reduce anxiety and distress. Avoidance coping is a coping mechanism for controlling and managing internal and external situations and reduces anxiety disorders in the short term; however, it maintains and exacerbates these disorders in the long term (12, 13).
Cognitive-behavioral avoidance is an inefficient strategy that increases the adoption of maladaptive behaviors, weakens the ability to manage the employment of effective responses to stimuli, and weakens the management of emotions (14). Individuals who adopt cognitive-behavioral avoidance strategies avoid participating in pleasurable activities, which makes them feel anxious, depressed, and sad, and these feelings further disconnect them from the real world (15, 16).
Research suggests that Emotional Schema Therapy (EST) and Dialectical Behavior Therapy (DBT) are among the methods that can improve emotional and psychological states in patients with irritable bowel syndrome (17) and borderline personality disorder (18). Emotional Schema Therapy is a new approach that addresses emotional issues and problems. It was designed by Leahy (19) based on the concept of emotional processing and inspired by the metacognitive model of emotions. According to this approach, emotional disorders are the result of individuals’ emotional schemas (i.e., beliefs), interpretations, and the strategies they use to deal with emotions (20).
Everybody experiences difficult and inappropriate emotions in their lives; however, their interpretations of and reactions to these emotions vary. Therefore, individuals have different schemas about their emotions that reflect how they experience their emotions (21). Patients with BD-II differ in how they interpret and evaluate their emotional experiences; therefore, they might use different strategies (e.g., experiential avoidance, ineffective or maladaptive cognitive strategies, social support-seeking strategies, and adaptive cognitive strategies) to cope with their emotions (22).
Dialectical Behavior Therapy was designed based on cognitive-behavioral therapy (CBT), dialectical philosophy, and mindfulness exercises (23). The four components of DBT include mindfulness, distress tolerance (acceptance components), emotion regulation, and interpersonal effectiveness (change components) (24). Dialectical Behavior Therapy provides clients with a comprehensive and multidimensional approach by combining their acceptance and empathy, resolving their cognitive-behavioral problems, and teaching them social and mindfulness skills (25). The main assumption of this approach is that individuals with poor cognitive emotion regulation skills suffer from deep pain and increased problems as they lack the required skills for solving problems and challenges (26). Dialectical Behavior Therapy initially tries to control the individuals’ activities and then teaches them the necessary behavioral skills to improve their health and well-being and overcome life problems and challenges in order to find pleasure and achieve success (27).
2. Objectives
Based on the issues outlined in the background, the present study aimed to investigate the effects of EST and DBT on psychological distress and cognitive-behavioral avoidance in patients with BD-II.
3. Methods
3.1. Design and Participants
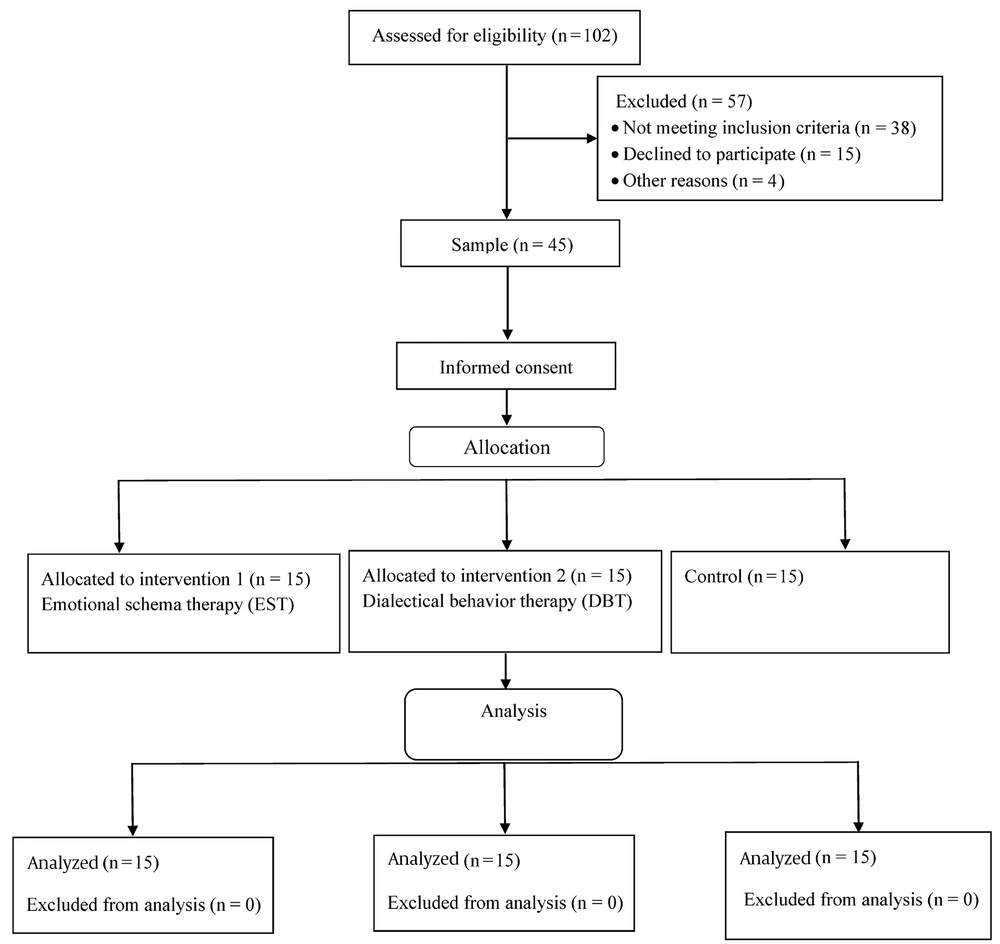
This quasi-experimental study adopted a pretest-posttest and control group design. The statistical population consisted of all patients with BD-II visiting the counseling centers in Dezful, Iran, in 2021. The participants meeting inclusion criteria were then enrolled using purposive sampling. In this study, the estimated minimum sample size was based on previous studies (28), and considering σ = 3.58, d = 4.58, power = 0.90, and α = 0.05, it was 12.82 subjects per group. Then, the final sample size of 15 subjects in each group was determined (taking into account the possibility of dropping participants in each group) (Figure 1).
3.2. Inclusion and Exclusion Criteria
The inclusion criteria included all patients in the 20 - 40 years age group with BD-II (diagnosed by a psychiatrist at least one year ago) who had not attended EST and SBT sessions in the past, with at least a high school diploma, and not receiving any other treatment during the study. The exclusion criteria included absence from more than one session, lack of cooperation in the intervention sessions, and unwillingness to continue research participation. The participants responded to the research scales in two stages, namely pretest and posttest, with the help of the researcher.
3.3. Intervention Programs
The first intervention program consisted of eleven 90-minute sessions of EST. Table 1 shows a summary of the sessions.
| Sessions | Content |
|---|---|
| 1 | Introducing the researcher and the participants and establishing a therapeutic relationship with the participants, stating the rules of the sessions, introducing the model of emotional schemas, validating emotions, explaining emotional, cognitive, and behavioral symptoms of mental disorders, and teaching participants how to differentiate and distinguish their thoughts, feelings, and behaviors from each other |
| 2 | Making the participants aware of emotional strategies and teaching them to identify their problematic strategies and emotional schemas |
| 3 | Teaching the participants, the techniques of utilizing emotions, using emotional labeling, and observing, describing, and recording emotions |
| 4 | Teaching the participants to use the technique of normalizing emotions, the technique of reducing stress, and the exercise of decreasing stress when stressful events occur |
| 5 | Teaching the participants how to challenge and cope with false beliefs about emotions, the technique of accepting emotions, and the technique of understanding the advantages and disadvantages of emotions and the false beliefs about them |
| 6 | Teaching the participants how to challenge their problematic strategies in order to get rid of them, to tolerate their mixed feelings, and to identify useful strategies for coping with emotions |
| 7 | Advising the participants to continue challenging their problematic strategies, teaching them how to identify their negative beliefs about and interpretations of emotions, and making them aware of their negative emotional schemas |
| 8 | Advising the participants to continue identifying and challenging their negative beliefs about and interpretations of emotions and to encourage them to adopt suitable behaviors for coping with negative beliefs about and interpretations of emotions, such as the feelings of shame and guilt |
| 9 | Advising the participants to continue challenging their negative beliefs about and interpretations of emotions, to use the technique of climbing the ladder of meanings, and to display appropriate and adaptive behaviors when they acquire positive beliefs about and interpretation of emotions, such as higher values |
| 10 | Advising the participants to continue challenging their negative beliefs about and interpretations of emotions, teaching them how to make room for their emotions, and providing them with a hard copy of the techniques and skills |
| 11 | Practicing the skills that were learned in previous sessions and reviewing, summarizing, and summing up the sessions |
A Summary of Emotional Schema Therapy (EST) Sessions
The second intervention program consisted of eleven 90-minute sessions of DBT. Table 2 shows a summary of the sessions.
| Sessions | Content |
|---|---|
| 1 | Introduction, establishing a therapeutic relationship, stating the rules of the sessions, introducing the general principles of Dialectical Behavior Therapy, and introducing the emotional, cognitive, and behavioral symptoms of disorders |
| 2 | Mindfulness training (emotional and wise awareness), attentional shift and distraction skills, and description of emotions without judgment or evaluation |
| 3 | Examining and identifying thoughts and emotions, identifying internalizing and externalizing coping responses, and examining thoughts and feelings that lead to emotional and self-destructive behaviors |
| 4 | Examining and identifying thoughts and feelings that lead to emotional and self-destructive behaviors and recording thoughts and feelings that lead to maladaptation |
| 5 | Distress tolerance and emotional management through mindfulness, relaxation, attentional shift, and distraction |
| 6 | Controlling impulsive behaviors and practicing their control and management |
| 7 | Identifying the consequences of emotion dysregulation, improving the use of emotion regulation processes, and the outcomes of cognitive-behavioral avoidance and planning to prevent them |
| 8 | Monitoring and managing one’s behaviors, identifying self-destructive behaviors and their consequences, reducing cognitive, behavioral, and emotional vulnerability, and increasing positive emotions |
| 9 | Emotion regulation through the identification of emotions themselves, identifying the cause and purpose of emotions, and reducing negative and increasing positive emotions |
| 10 | Providing emotional responses and transforming negative into positive emotions |
| 11 | Increasing the efficiency of interpersonal relationships by improving one’s relations with friends and acquaintances, establishing interest-based relations, practicing the skills taught in previous sessions, and a summary of the sessions |
A Summary of Dialectical Behavior Therapy (DBT) Sessions
3.4. Instruments
Kessler Psychological Distress Scale (K10): This 10-item scale was designed by Kessler et al. (29). The items are scored on a five-point Likert scale, including never (score 0), rarely (score 1), sometimes (score 2), most of the time (score 3), and all of the time (score 4). The sum of scores given to all items determines the total psychological distress score. The total score ranges from 0 to 40, with higher scores indicating greater psychological distress. Mandizadeh and Homaei (30) reported an alpha Cronbach coefficient of 0.95 for the K10. The authors (30) reported the content validity index (CVI) for this scale above 0.90. In the present study, Cronbach’s alpha for the K10 was 0.89.
Cognitive-Behavioral Avoidance Scale: This 31-item tool was developed by Ottenbreit and Dobson (31). The items are scored on a five-point Likert scale, including not at all true (score 1), not true (score 2), somewhat true (score 3), true (score 4), and completely true (score 4). The sum of scores given to all items determines the total cognitive-behavioral avoidance score. The total score ranges from 31 to 155, with higher scores indicating a greater extent of cognitive-behavioral avoidance. The validity and reliability of the Cognitive-Behavioral Avoidance Scale have been deemed optimal by Moloodi et al. (32). The test-retest reliability estimate of the scale was reported to be 0.81. In the present study, Cronbach’s alpha for the Cognitive-Behavioral Avoidance Scale was 0.79.
3.5. Data Analysis
The data were analyzed in SPSS software (version 26) using descriptive statistics (mean and standard deviation [SD]) and inferential statistics (analysis of covariance [ANCOVA]). The Kolmogorov-Smirnov test was used to assess the normality of data distribution. In addition, the Bonferroni post hoc test was used to compare the effects of interventions on the dependent variables. The significance level of the study was considered to be α = 0.05.
4. Results
The mean and SD of the participants’ age in the EST, DBT, and control groups were 30.27 ± 6.84, 29.71 ± 7.11, and 28.87 ± 7.30 years, respectively. In addition, the duration of the disease of the participants in the EST, DBT, and control groups was 4.18 ± 2.39, 3.75 ± 2.09, and 4.48 ± 2.41 years, respectively. Table 3 shows the mean (SD) of the pretest and posttest scores of the psychological distress and cognitive-behavioral avoidance in the EST, DBT, and control groups.
| Variables | Phases | Mean ± SD | ||
|---|---|---|---|---|
| EST Group | DBT Group | Control Group | ||
| Psychological distress | Pretest | 15.53 ± 3.09 | 16.64 ± 2.82 | 15.40 ± 2.66 |
| Posttest | 11.40 ± 2.41 | 12.26 ± 2.28 | 15.73 ± 2.73 | |
| Cognitive-behavioral avoidance | Pretest | 87.53 ± 10.58 | 85.73 ± 8.45 | 89.66 ± 8.66 |
| Posttest | 79.73 ± 10.68 | 78.20 ± 8.05 | 90.26 ± 8.72 | |
Mean and Standard Deviation (SD) of Psychological Distress and Cognitive-Behavioral Avoidance in the Experimental and Control Groups
The Kolmogorov-Smirnov test results confirmed the normality of data distributions for psychological distress and cognitive-behavioral avoidance before and after the intervention. After the intervention, significant differences were observed among the three groups in variables of psychological distress (F = 97.22, P < 0.001, Eta = 0.84) and cognitive-behavioral avoidance (F = 165.77, P < 0.001, Eta = 0.90) (Table 4).
| Variables | Source | SS | df | MS | F | P | η2 | Power |
|---|---|---|---|---|---|---|---|---|
| Psychological distress | Pretest | 206.62 | 1 | 206.62 | 231.67 | 0.001 | 0.86 | 1.00 |
| Group | 173.42 | 2 | 86.71 | 97.22 | 0.001 | 0.84 | 1.00 | |
| Error | 33.89 | 38 | 0.89 | |||||
| Cognitive-behavioralavoidance | Pretest | 3375.82 | 1 | 3375.82 | 1808.01 | 0.001 | 0.98 | 1.00 |
| Group | 619.02 | 2 | 309.51 | 165.77 | 0.001 | 0.90 | 1.00 | |
| Error | 70.95 | 38 | 1.87 |
Results of Analysis of Covariance to Determine Effectiveness of Interventions in Psychological Distress and Cognitive-Behavioral Avoidance
Table 5 shows the results of the Bonferroni post hoc test performed to compare the effects of each intervention approach on the dependent variables (psychological distress and cognitive-behavioral avoidance) in patients with BD-II. The comparison of the means of the EST and DBT groups showed that the two approaches were almost equally effective in reducing psychological distress and cognitive-behavioral avoidance in patients with BD-II (P < 0.001). In addition, as shown in Table 5, there was no significant difference between EST and DBT approaches in reducing psychological distress and cognitive-behavioral avoidance in patients with BD-II.
| Variables | Groups | Mean Difference | SE | P |
|---|---|---|---|---|
| Psychological distress | EST-DBT | - 0.09 | 0.36 | 0.999 |
| EST-Control | - 4.44 | 0.36 | 0.001 | |
| DBT-Control | - 4.34 | 0.37 | 0.001 | |
| Cognitive-behavioral avoidance | EST-DBT | - 0.55 | 0.52 | 0.883 |
| EST-Control | - 8.55 | 0.52 | 0.001 | |
| DBT-Control | - 7.99 | 0.53 | 0.001 |
Bonferroni Post Hoc Test for Paired Comparison of Psychological Distress and Cognitive-Behavioral Avoidance
5. Discussion
The present study aimed to investigate the effects of EST and DBT on psychological distress and cognitive-behavioral avoidance in patients with BD-II. Both EST and DBT approaches significantly reduced levels of psychological distress and cognitive-behavioral avoidance in patients with BD-II. However, no significant difference was observed between EST and DBT approaches in reducing psychological distress and cognitive-behavioral avoidance in patients with BD-II. In line with the findings of the present study, Erfan et al. (17) showed that EST is an appropriate option for the treatment of patients with irritable bowel syndrome because it is effective in the improvement of emotional schemas and difficulties of emotional regulation. Moreover, Tebbett-Mock et al. (24) reported that DBT reduced aggression and seclusion in adolescents with psychological disorders.
The EST approach teaches patients with BD-II to recognize ineffective emotion regulation strategies, points out the temporary nature of the pleasant feeling caused by these strategies, and helps individuals accept their unpleasant emotions (17). In addition, therapists use the emotion normalization technique to help patients feel less distressed after understanding the psychological distress they are currently experiencing and accepting their unpleasant emotions. Moreover, it should be noted that patients with BD-II have different schemas about their emotions, reflecting the way they experience their emotions and how they believe they should deal with their pleasant and unpleasant emotions.
Emotional Schema Therapy precisely targets emotion processing and negative interpretations, thereby encouraging patients to replace ineffective and maladaptive coping strategies with effective strategies when facing pleasant and unpleasant emotions (19). The basic logic behind the EST approach is that emotions are not inherently problematic; nevertheless, individuals’ interpretations of emotions, their emotional reasoning, and the coping strategies they adopt to respond to emotions might cause problems. Emotional Schema Therapy is a third-wave cognitive-behavioral therapy that lowers levels of cognitive-behavioral avoidance by reducing emotional disturbance. Emotional Schema Therapy first helps patients identify their ineffective coping strategies (e.g., getting engaged in post-event processing and using avoidance strategies) and then uses emotion acceptance and mindfulness techniques to reduce their anxiety emotions (20). The mindfulness exercises used in this approach increase patients’ psychological flexibility and, therefore, facilitate their acceptance of emotions, improve their conscious existence, and replace their ineffective coping strategies with effective observation and acceptance techniques (22). Therefore, EST effectively reduced levels of psychological distress and cognitive-behavioral avoidance in patients with BD-II.
Through communication skills, behavior control, optimism, empathy, and decision-making power, the DBT approach can increase health and reduce distress in individuals with anxiety disorders through hopeful and purposeful thinking. In addition, as a therapeutic approach, DBT combines the principles of cognitive-behavioral therapies with the Eastern philosophy of mind, which is based on the principle of acceptance (23). This approach emphasizes controlling tension and moderating behavior by increasing abilities via the provision of facilities required for this increase. In general, the use of the DBT approach increases individuals’ resistance to conflicts and problems and reduces their stressful behaviors, thereby increasing their feelings of trust and continuous and comprehensive dynamism in everyday life (25).
Teaching distress tolerance skills to individuals with anxiety disorders enhances their sense of connectedness and mental strength. These skills teach individuals to cope better with disturbing events (e.g., anxiety) and their annoying symptoms and display fewer avoidance behaviors. In addition, the use of DBT techniques enables individuals to live more peaceful, manageable, and meaningful lives by understanding and accepting the emotions, events, problems, and feelings they experience in their lives (28). In this therapeutic approach, especially due to the mindfulness skills, individuals trained in distress tolerance and interpersonal relation techniques and skills become able to use effective coping strategies in appropriate situations and overcome their disturbing emotions by employing self-talk and self-soothing techniques (27). Therefore, DBT plays an effective role in reducing levels of psychological distress and cognitive-behavioral avoidance in patients with BD-II.
Emotional Schema Therapy generally aims to identify and correct individuals’ incompatible and problematic beliefs and interpretations of their emotional experiences and replace them with new, compatible, and flexible beliefs, interpretations, and strategies. Dialectical Behavior Therapy, in addition, aims to reduce the suffering of individuals with emotional problems, improve their psychological health, decrease their negative emotions and experiences, and increase their positive emotions. Moreover, EST is a holistic approach that improves individuals’ psychological characteristics by combining the strategies of schema therapy, CBT, the metacognitive model of emotions, and emotion-focused therapy.
The limitations of the present study included limiting the study population to patients with BD-II in Dezful, Iran, and selecting the eligible participants using a non-random sampling method. In addition, some demographic characteristics of the participants (e.g., socioeconomic status), which could not be controlled by the researcher, might have affected the final results of the study.
5.1. Conclusions
Emotional Schema Therapy and Dialectical Behavior Therapy, both third-wave cognitive-behavioral therapies with many common principles and advantages, were almost equally effective in reducing psychological distress and cognitive-behavioral avoidance in patients with BD-II. Accordingly, counselors, therapists, and health professionals are recommended to use EST and DBT interventions either alone or together to reduce psychological distress and cognitive-behavioral avoidance or improve other psychological variables in patients with BD-II.