1. Background
Non-communicable diseases, including heart disease, are considered a global health challenge. About 620 million people worldwide live with heart and circulatory diseases. Globally, it is estimated that 1 in 13 people live with heart or circulatory disease (1). In 2019, approximately 17.9 million people died from cardiovascular diseases, accounting for 32% of all global deaths (2). Additionally, cardiac disease is the leading cause of disability-adjusted life years (DALYs) in the world (1). The prevalence of heart disease in the Eastern Mediterranean region is reported to be relatively higher in men than in women across all age groups. The burden of heart diseases in the Eastern Mediterranean region is higher than the global burden, with an increase in age-standardized prevalence and years lived with disability (YLDs) in the countries of the region (3). It is reported that more than three-quarters of deaths from heart disease occur in low- and middle-income countries (4). In the Middle East region, 55% of deaths caused by non-communicable diseases and 28.5% of all deaths are attributed to cardiovascular diseases (5, 6). A cohort study of 9,828 people in Iran showed that the prevalence of cardiovascular diseases in women (16.2%) is higher than in men (12.6%) (7). Additionally, cardiovascular diseases have an increasing trend with age, reaching 27.9% in individuals aged 65 - 70 years (7). The prevalence of cardiac disease may be associated with socio-economic, cultural, and nutritional changes, inadequate physical activity, industrialization, urbanization, increased life expectancy, and increased metabolic and physical risk factors (8).
Researchers and physicians have long sought to reduce the incidence of cardiac disease by taking preventive measures at the primary and secondary levels (e.g., behavioral modification and risk factor elimination) (9). Patients with cardiac disease must be able to actively manage their disease, medication use, and symptoms and properly take care of themselves. Meanwhile, patient activation is required to convince patients to follow and implement self-management recommendations. The concept of patient activation refers to “an individual’s knowledge, skills, and self-confidence in health management and self-care.” It implies that patients must monitor their conditions, modify their lifestyles, and seek professional help whenever needed to solve their problems (10). Patient activation is considered the most valid indicator of willingness and ability to manage health care activities (11, 12). This theory is rooted in the concepts of self-efficacy, belief, skill, and confidence (11). Self-efficacy, derived from Bandura’s social cognitive theory, refers to one’s trust and confidence in oneself to perform tasks and take care of oneself satisfactorily to achieve desirable results (13).
Patients enter the activation process in four stages. In the first stage, people are overwhelmed and must prepare themselves to play an active role in the process. They are prone to receive care but passively. In the second stage, people lack the knowledge and self-confidence required for self-management. In stage 3, people start taking action but still do not have the necessary confidence and skills to support new behaviors. Finally, in the fourth stage, people have enough confidence to display the behavior but may find it difficult to control their nerves under pressure (14). High activation levels have generally been associated with positive clinical outcomes in populations with chronic conditions (15). However, the activation rate of chronic patients is still low (11, 16).
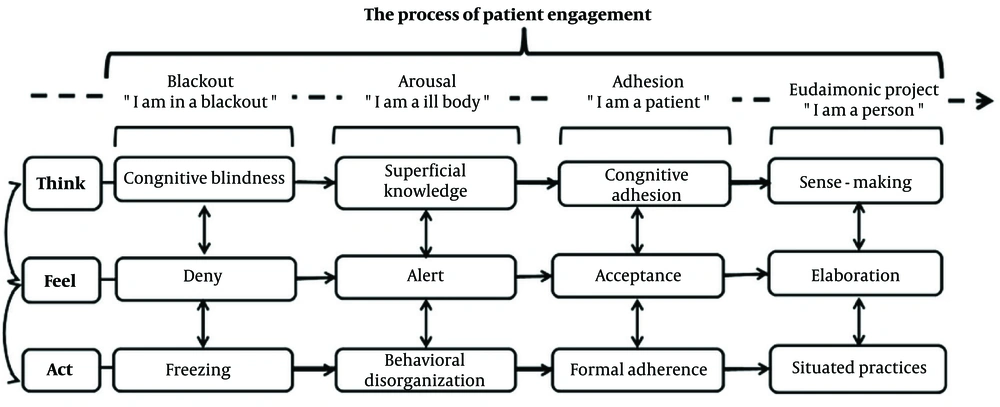
One of the new models that tries to make the patient understand that they should not be passive is the patient health engagement (PHE) model. The PHE model provides a simple and concrete conceptualization of how patients may 'think,' 'feel,' and 'act' in relation to their health conditions, thus constituting how patient engagement may (or may not) be involved. This model describes the engagement of patients in the care process very well (11). The engagement of patients in the care process has become the main pillar of health policies. The PHE model is based on consumer-oriented psychology and refers to the role of emotional maturity as a key factor in enabling patients to adapt to new health conditions (17). The patient should generally feel more positive and experience higher quality patient-doctor-nurse relationships. This model allows doctors, nurses, and healthcare professionals to better understand their patients' experience of chronic health conditions (17).
The PHE model consists of four situations. In the first situation (blackout), distressed patients need to receive support from others (1). These patients cannot understand and accept their health conditions and disease. In the second stage (arousal), patients are alert to any symptom in their body. Clinical symptoms act like alarms that warn patients about their conditions. In the third stage (adhesion), patients develop extensive health literacy (18). In addition, healthcare professionals help patients increase their confidence to better deal with the disease (17). In the eudaimonic project (stage 4), patients become more active in the disease management process and tend to share their healthcare experiences with others (1). After discovering the identity of their disease, patients fully accept their health conditions. Illness becomes a part of their lives, and despite their conditions, they continue to live their normal lives and play their social roles with a healthy lifestyle (18). In this stage, patients manage their disease and control their health conditions in all situations, achieving a better quality of life (2).
The PHE model has been introduced in recent years, and studies using this model are still few. However, Graffigna et al. showed that the PHE model sheds light on the possible psychological roots of patient motivation for self-management. The role of the PHE model in determining patient activation and clinical performance seems promising (18). Another study showed that the PHE scale can predict social support, self-efficacy, quality of life, and all its dimensions in chronic patients and is the strongest predictor of understanding and participation in care (19). There are very few studies based on a framework designed solely for chronic patients, and the PHE model may be the first model created for self-management and control of health conditions in non-communicable diseases.
2. Objectives
Considering the situation of chronic diseases in Khuzestan province and the necessity of disease management, this study assessed relationships of PHE with self-efficacy and activation in cardiac disease patients (Figure 1).
3. Methods
Study Design and Sample: This descriptive-analytical study is cross-sectional. Subjects were cardiovascular patients referred to a public hospital in the southern cities of Abadan and Khoramshahr in Iran during the year 2020. Inclusion criteria were: Having cardiovascular disease, having a minimum literacy level, and willingness to participate in the research (Table 1). Exclusion criteria included incomplete responses to the questionnaire. The sample size was calculated as 173 using the following formula (α = 0.05; 95% confidence level; P = 35.6; d = 0.1p). The final size was then determined (n = 207) by considering a loss to follow-up of 20% (20).
The random sampling method was simple. Patients were selected based on the registry of patients' names and were included in the study after obtaining informed consent.
3.1. Data Collection Tools
Patient activation measurement (PAM-19): This tool uses a 5-point Likert Scale (strongly disagree to strongly agree) and includes four dimensions: Belief (2 questions), knowledge to action, confidence (10 questions), active involvement (5 questions), and continuity under pressure (2 questions). The validity and reliability of this questionnaire were confirmed in the study by Ramezani et al. (CVR = 1, CVI = 0.89, Cronbach's alpha = 0.78) (21).
Health promotion strategies (SUPPH): This consists of 29 items on a Likert Scale and includes three subscales: Stress reduction (10 questions), decision making (3 questions), and positive attitude (16 questions). Each question is scored from 1 to 5, with a Cronbach's alpha of 0.94 (16).
Patient Health Engagement Scale: This scale is developed based on the PHE model with an ordinal structure, including five items and four main scores. Factor loadings from categorical principal component analysis (CATPCA) for PHE items in the present study were: Item 1 = 0.737, Item 2 = 0.803, Item 3 = 0.798, Item 4 = 0.850, and Item 5 = 0.821. The initial analysis yielded one factor with an eigenvalue of 3.22, which is above the Kaiser Criterion of 1, explaining 64.41% of the total variance. All subjects were in the third stage of the PHE model. The internal consistency showed an average inter-item polychoric correlation of 0.55, indicating a moderate correlation between items. Cronbach's alpha was 0.97.
Statistical analysis: The Kolmogorov-Smirnov test was used to determine the normality of the data. Data were analyzed using descriptive tests, linear regression, optimal scaling, correlation tests, and CATPCA.
4. Results
Out of the 204 subjects, 52.5% (107) were male and 47.5% (97) were female. The minimum and maximum weights were 53 kg and 123 kg, respectively. The blood pressure ranges were 160 - 190 mm Hg for systolic and 100 - 120 mm Hg for diastolic. In addition to cardiovascular disease, 38.2% (78) had high blood pressure, 20.1% (41) had diabetes, 17.6% (36) had both hypertension and diabetes, 9.3% (19) had lung disease, 3.9% (8) had cancer, and 3.9% (8) were depressed. Based on the PHE scale score, the median was 3. The results of the retest showed a positive correlation (P > 0.124, r = 0.287). Among the subjects, 27.5% (56) smoked cigarettes, 2.5% (5) used opium, and 8.3% (17) smoked hookah.
| Variables | Values |
|---|---|
| Education | |
| Primary school | 48 (23.5) |
| Junior high school | 39 (19.1) |
| High school | 64 (31.4) |
| College education | 53 (26) |
| Job | |
| Unemployed | 29 (14.2) |
| Retired | 47 (23) |
| Self-employment | 45 (22.1) |
| Employee | 44 (21.2) |
| Housewife | 39 (19.1) |
| Age | 47.24 ± 14.72 |
| Weight | 75.33 ± 12.44 |
| Systolic BP | 135.77 ± 24.29 |
| Diastolic BP | 84.59 ± 16.97 |
a Values are expressed as No. (%) or mean ± SD.
The mean and standard deviation of the self-efficacy score (SUPPH Health Promotion Strategies) and the PAM-19 scale and its dimensions are presented in Table 2.
| Variables | Mean ± SD | Min - Max |
|---|---|---|
| SUPPH | 82.18 ± 15.67 | 33 - 125 |
| PAM | 69.09 ± 9.57 | 41 - 95 |
| (PAM construct) believe | 8.39 ± 1.34 | 4 - 10 |
| (PAM construct) knowledge to action, confidence | 35.73 ± 5.77 | 18 - 52 |
| (PAM construct) active involvement | 18.64 ± 3.17 | 9 - 25 |
| (PAM construct) continuity under pressure | 6.37 ± 1.81 | 2 - 10 |
Abbreviations: PAM, patient activation measurement; SUPPH, health promotion strategies.
The chi-square test showed a significant relationship between the PHE model scale and variables such as sex, job, and smoking. According to the levels of the model, women had more unpleasant feelings than men (56.4% vs. 43.6%), but men had more awareness and information about the disease than women (64.2% vs. 35.8%). Education was not associated with any levels of the PHE model (P > 0.05). Job was related to all four levels of the model. According to the model, retired people, self-employed individuals, and housewives felt more alert and worried about their illness (25.5%). Moreover, 28.3% of retirees had more information and awareness about their disease. However, employees felt more positive and had a better ability to manage the disease (45.5%). Unemployed people were more worried about the new symptoms of their disease than others (26.1%). Having some diseases showed a significant relationship with the model, particularly high blood pressure and diabetes (P < 0.05). The chi-square test showed that all four levels of the PHE model are related to smoking and were more prevalent in people who did not smoke (P < 0.05).
In this study, half of the subjects had moderate self-efficacy, and the other half had good self-efficacy (49.5%). Additionally, 58.5% had a moderate activation score, and only 39.7% had a good activation score. Correlation test analysis showed a significant relationship between demographic variables and PAM and SUPPH. The chi-square test showed that age has a significant relationship with the levels of the PHE model (P < 0.001, df = 57, F = 1.88), but no significant relationship was found between weight, systolic, and diastolic blood pressure with the four levels of the PHE model (Table 3).
| Variables and Sex | Values |
|---|---|
| PAM | |
| Male | 69.6 ± 9.2 |
| Female | 68.4 ± 9.9 |
| P | 0.01 a |
| SUPPH | |
| Male | 84.01 ± 17.08 |
| Female | 81.8 ± 17.3 |
| P | < 0.001 a |
| PHE-S | |
| P | 0.005 a |
| Education level | |
| PAM | P = 0.003 b; r = 0.21 |
| SUPPH | P = 0.79 b; r = 0.01 |
| PHE-S | P = 0.01 a |
| Job | |
| PAM | P = 0.70 b; r = 0.026 |
| SUPPH | P < 0.01 b; r = -0.18 |
| PHE-S | P < 0.001 a |
| Age (mean ± SD) | |
| Male | 47.4 ± 13.8 |
| Female | 47.01 ± 15.6 |
| PAM | P = 0.16 b; r = -0.09 |
| SUPPH | P = 0.26 b; r = -0.07 |
| PHE-S | P < 0.001 a |
| Weight | |
| Male | 77.2 ± 12.3 |
| Female | 73.1 ± 9.7 |
| PAM | P = 0.005 b; r = 0.194 |
| SUPPH | P = 0.18 b; r = -0.09 |
| PHE-S | P = 0.19 a |
| Smoking | |
| PAM | P = 0.03 a |
| SUPPH | P = 0.42 |
| PHE-S | P = 0.01 a |
| Systolic BP | |
| PAM | P = 0. 81 b; r = 0.01 |
| SUPPH | P = 0.87 b; r = 0.01 |
| Phe-scale | P = 0.06 |
| Diastolic BP | |
| PAM | P = 0.21 b; r = 0.08 |
| SUPPH | P = 0.78; r = 0.01 |
| PHE-S | P = 0.24 |
| Disease | |
| PAM | P < 0.001 a |
| SUPPH | P < 0.006 a |
| PHE-S | P < 0.001 a |
Abbreviations: PHE-S, Patient Health Engagement Scale; PAM, patient activation measurement; SUPPH, health promotion strategies.
a Chi-square test.
b Correlation test.
The Spearman correlation test showed that self-efficacy (SUPPH) had a positive and significant correlation with the overall patient activation score and its dimensions. This correlation in the active participation dimension is greater than in other dimensions (Table 4).
| Variable | PAM | Believe | Knowledge to Action, Confidence | Active Involvement | Continuity Under Pressure |
|---|---|---|---|---|---|
| SUPPH | |||||
| r | 0.535 | 0.336 | 0.433 | 0.549 | 0.291 |
| P-value | < 0.001 | < 0.001 | < 0 .001 | < 0 .001 | < 0 .001 |
Abbreviations: PAM, patient activation measurement; SUPPH, health promotion strategies.
The linear regression test showed that demographic variables predict 11% variance of patient activation (R square = 0.110, adjusted R square = 0.069, df = 9, F = 2.66, confidence interval (CI) = 0.312 - 2.978, P = 0.006), but education level was a stronger predictor for patient activation (β = 1.645, t = 2.43, P = 0.016). However, demographic variables were not predictors of self-efficacy (R square = 0.049, adjusted R square = 0.005, df = 9, F = 1.11, P = 0.355). The optimal scaling regression (categorical regression) test showed that the PHE scale predicted 26.4% variance of self-efficacy and 25.2% variance of patient activation (PAM) (Table 5).
| Variables | Multiple R | R Square | Adjusted R Square | df | F | β | P-Value |
|---|---|---|---|---|---|---|---|
| SUPPH | 0.514 | 0.264 | 0.238 | 7 | 10.06 | 0.205 | < 0.001 |
| PAM | 0.502 | 0.252 | 0.213 | 10 | 6.48 | 0.289 | < 0.001 |
| Belief (PAM) | 0.386 | 0.149 | 0.105 | 10 | 3.37 | 0.207 | < 0.001 |
| Knowledge to action, confidence | 0.454 | 0.206 | 0.161 | 11 | 4.53 | 0.246 | < 0.001 |
| Active participation | 0.471 | 0.222 | 0.182 | 10 | 5.05 | 0.289 | < 0.001 |
| Continuity under pressure | 0.364 | 0.133 | 0.082 | 11 | 2.65 | 0.284 | 0.003 |
Abbreviations: PAM, patient activation measurement; SUPPH, health promotion strategies.
5. Discussion
Patient engagement is an international issue from the point of view of the World Health Organization and other institutions in nursing care and is necessary and important. Patient engagement in nursing care has good benefits, including effective healthcare services, decision-making in treatment, improvement of patient safety, improvement of quality of care, fewer medication errors, and more adherence to medication and diet (22). In PHE, an effective health relationship between nurse and patient is formed according to the cultural context and the conditions of society, where nurses are encouraged to educate patients so that they can actively participate in self-care (22). The present study can be considered one of the first studies with the PHE model in people with a history of heart disease. Doctors, nurses, and healthcare providers should promote patient participation at a higher level of self-efficacy and activation using health engagement models. In the present study we examined the effect of the PHE model on patient self-efficacy and activation. For more certainty, we re-evaluated the Persian version of the PHE-scale despite the previous validation (23). Data analysis showed that the findings were similar to other studies in terms of internal consistency and reliability (24). The mean activation score in this study was 69.09, which is similar to Skolaski et al.'s and Wang et al.'s studies but contradictory to Hendrick and Rademakers (14, 25, 26). Maybe the reason is the average age of the respondents and their ability. We found that some of the patients were at the fourth PAM level and most of them at the third PAM level. These results once again confirm the validity of PAM to measure the knowledge required for self-management of the disease. Therefore, the level of patient activation measured may reflect people's knowledge about health and healthcare for health management (14). Self-management of these patients can be substantially improved by enhancing their activation levels (26). Mirmazhari et al. found that most dialysis patients were at activation level 1 and only 28.9% were at activation level four (27). The results show that patients with low activation have almost twice the risk of reusing hospital services one month after discharge compared to patients with higher activation, and these patients are more likely to return to the hospital (28). Also, the patient activation score of female patients was lower than that of male patients, which aligns with the Dutch study of Rademakers et al. (29). Our findings showed no evidence for an association between age and patient activation. This result is similar to that of Wilkins et al. and inconsistent with the findings of Zimbudzi et al. (29-31). This may be due to the presence of different age groups in this study. Young people seem to be more active in their treatment and care process (31). However, the chronic conditions of older people can reduce their active engagement in the disease management process (32). In the present study, we found that patient activation was related to education level and weight. It seems that individual characteristics, including patient activation, can play a role in physical, mental, and behavioral functions (self-confidence and communicating with doctors and nurses) in primary care for people with chronic diseases (33). However, in the study by Chang et al., no significant difference was found between patient activation and weight (34). Experience shows that people with greater education levels and better health knowledge are more actively involved in their treatment and care process (14, 28, 35). Our findings showed a significant relationship between depression and patient activation. A cohort study in the United Kingdom among all patients found that depression had the strongest relationship with patient activation, consistent with the findings of the present study (35). In general, poor concentration, insomnia, anorexia, and lack of motivation can adversely affect patients' confidence and decisions and reduce their participation in disease management (36). In the present study, systolic and diastolic blood pressure scores were not related to patient activation, self-efficacy, and the PHE model. A bivariate analysis in another study found no statistically significant association between patient activation and systolic or diastolic blood pressure (3). Overall, while some studies support a positive relationship between patient activation and blood pressure control, the evidence is not entirely consistent (31). However, further research may be needed to fully understand the impact of patient activation on blood pressure and related health outcomes. The total self-efficacy score of half of the participants was moderate, similar to the study of Nuraeni et al. (37). In the present study, the self-efficacy scores of men were generally higher than those of women. Other research supports our findings (38, 39). We found a relationship between self-efficacy, sex, and job. Our findings are consistent with the research of Khairy et al. (40). Self-efficacy was correlated with patient activation. However, it predicted a small percentage of activation. Mirmazhari et al. confirmed our findings (27). Patient activation can improve the ability to manage chronic conditions through self-efficacy. Reduced perceived stress, fewer symptoms of anxiety and depression, and less severe symptoms are the result of high levels of self-efficacy (14, 41). Playing an active role in healthcare activities is an important aspect of self-efficacy that can be learned and practiced (39). According to Bandura, people with poor self-efficacy cannot do any task perfectly even if they finish it (13). In fact, self-efficacy facilitates healthy behavior by activating patients (41). A study shows that nursing can use perceived self-efficacy with self-management to improve the functional status and quality of life of its patients. Also, nurses can have a significant positive impact on the lives of their patients by reducing the burden of symptoms related to chronic disease and its treatment (42). Based on the PHE Scale, in this study, patients were at the third level. In this stage, patients are prepared to formally display the prescribed behavior and follow the recommendations of healthcare professionals (18). Chi-square tests showed that the PHE Scale had a significant relationship with all demographic variables except weight and blood pressure score. A study highlighted the association between demographic factors and emotional outcomes (43). Linear regression showed that demographic variables predicted 11% of patient activation variance. However, they did not predict health promotion strategies (self-efficacy). The optimal scaling regression indicated the PHE model can predict self-efficacy (26.4%) stronger than patient activation, which is consistent with the study by Changizi et al. (19). The PHE model emphasizes the importance of sustaining collaborative spaces between healthcare professionals and patients, highlighting the role of self-efficacy in patients' meaningful engagement in their own healthcare (11, 18). According to a study, increased patient engagement in the healthcare procedure improves self-efficacy in cardiac patients, and self-efficacy in turn facilitates the management of the treatment process (44). Chen argues that self-efficacy can be improved through successful experience, verbal persuasion, role-playing, and positive emotion via intervention programs (45). Hopeful people feel that they are in control of their lives and that they can reduce their stress and negative emotions. They also think that they can change their living conditions to create a better future; therefore, they want to live (46). In patients with cardiac diseases, improvements in self-efficacy are associated with an improvement in lifestyle (47). However, to provide quality care services, professionals must acquire a deep understanding of patients’ emotional states and their ability to actively engage in the disease management process (18). It seems that providing an opportunity to participate in the care process for chronic patients, such as those with cardiac diseases, may improve the quality of care, self-management, treatment-related decisions, and informed and reciprocal participation (48). Nurses strive to respect patients' perspectives and accept patients as part of the care team. The study showed that healthcare providers who believe in managing the patient's health conditions are more likely to engage with patients who have more collaborative behaviors (49, 50). However, another study showed that younger nurses are not inclined to accept the patient's collaborative role and deal with the patient's active behavior. It may indicate that patient participation behavior requires advanced nursing skills for the optimal implementation of health interventions (51). The PHE model may be considered a lever to strengthen patients' activation and self-efficacy. There are very few studies on the application of the PHE model in Iran. Future research may be useful to increase the ability of nurses to deeply understand the emotional and cognitive experiences of patients and to increase their level of engagement using the theoretical framework for chronic patients in order to effectively manage health conditions. There are some limitations to this study. The results of this study are limited to the geographical area covered. Patients referred to physicians' offices were not included in the study.
5.1. Limitations
One of the limitations of our study was the lack of a focused cardiovascular clinic and low access to patients. However, in our study, the latest instrument was used to measure patient engagement in the health and care process.
5.2. Conclusions
The PHE scale assesses patients’ ability to think about their disease and manage it. The model also targets health behaviors, health promotion strategies, and activation of cardiac patients. Patient activation is slightly related to self-efficacy. However, it is mainly controlled by other factors that should be assessed. The findings confirmed the effect of the PHE model on self-efficacy, and this factor must be further examined in health interventions. An intervention designed based on this theory may facilitate the emotional, psychological, and behavioral processes associated with patient engagement and lifestyle modification. Patient engagement improves clinical outcomes and patients’ post-treatment satisfaction levels, and ultimately, engagement in health management seems to be essential for maintaining an active role in society.