1. Background
Asthma is a global chronic health issue in children (1). Approximately 300 million people worldwide have asthma, and it is estimated that by 2025, another 100 million will be affected (2). Asthma is one of the most common chronic and noncommunicable diseases in children, and its prevalence is changing globally. The prevalence of asthma symptoms, such as wheezing, varies from 0.8% in China to 36.6% in New Zealand among children aged 13 - 14 years and from 2.4% in India to 37.6% in Costa Rica among children aged 6 - 7 years (3). Additionally, based on a meta-analysis study by Hassanzadeh et al., the prevalence of asthma in Iranian children ranges from 1.26% to 11.6% (4).
Asthma has a significant impact on the quality of life of affected individuals (5). Elzoghby et al. demonstrated that childhood asthma has a significant and negative effect on the quality of life of children (6). Inadequate management and poor control of asthma limit children's physical, social, and educational performance and reduce their quality of life (7). Previous studies have shown that poor quality of life is significantly associated with the severity of childhood asthma (8, 9), uncontrolled asthma, and hospitalization for asthma (8). Therefore, effective asthma management improves the quality of life of children (10). Asthma imposes a significant burden on families, children, and the healthcare system, and measuring quality of life helps evaluate the effectiveness of clinical interventions in children with asthma (11). It is recommended to assess the quality of life during children's clinic visits to achieve a comprehensive and effective treatment approach (12).
One of the alternative treatments, particularly for chronic diseases, that is popular worldwide is yoga. Some studies have confirmed the positive effects of yoga on children's health (13, 14). Yoga/pranayama breathing exercises are among the nonpharmacological methods that play a special role in the treatment of asthma (15, 16), and they are currently a preferred alternative treatment for asthma globally (17). Yoga helps reduce bronchospasm and breathlessness by modifying the breathing pattern, reducing hyperventilation, and normalizing CO2 levels (18). Hyperventilation adversely affects lung function, asthma symptoms, and the comfort status of individuals with asthma (19). Therefore, children with asthma can benefit from proper breathing techniques.
The effects of yoga on asthma have been under research for an extended period. One of the pioneering clinical trials conducted by Nagarathna and Nagendra involved 106 patients aged 9 - 47 years with bronchial asthma. Their study revealed that yoga appears to reduce vagal efferent reactivity by inducing relaxation in both the body and mind. It is considered a mediator of the psychosomatic factor in asthma (20). In a systematic review by Das et al., it was suggested that breathing exercises and yoga/pranayama may be beneficial in treating asthma in children. However, further studies with more homogeneous and higher-quality designs are required to provide conclusive evidence regarding the use of these alternative/complementary therapies in children with asthma (16). Since yoga, as a complementary treatment, aligns with nursing interventions and theories (21) and holds promise as a nursing intervention to enhance the health of children at various ages (22), conducting this research is important in the field of child care.
2. Objectives
This study aimed to investigate the impact of yoga breathing exercises on the quality of life of children with asthma.
3. Methods
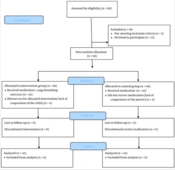
This quasi-experimental study involved both control and intervention groups in 2 stages: Before and after the intervention. Initially, 110 children with asthma were recruited from the asthma clinic at one of the children's hospitals affiliated with Iran University of Medical Sciences and assessed for eligibility. Eventually, 84 eligible children aged 5 - 11 years were included in the study, with 42 in the intervention group and 42 in the control group (Figure 1).
Eighty-four children participated in the study through a continuous sampling method, spanning from May to November 2018. These participants were nonrandomly allocated to the intervention (n = 42) and control (n = 42) groups. To prevent the potential sharing of information, we assigned eligible children admitted to the clinic to the intervention and control groups on separate days. The sample size was determined based on a confidence level of 95%, test power of 80%, d = 0.7, a standard deviation of 1.1, and an attrition rate of 20%.
All parents provided written informed consent before the study, and the children also gave their verbal consent. The inclusion criteria were as follows: Diagnosis of intermittent asthma, mild persistent asthma, or moderate persistent asthma in school-age children aged 5 - 11 years, based on a physician's diagnosis and following the Global Initiative for Asthma (GINA) guidelines (23, 24). Additionally, children were required to have had asthma for at least 6 months. Exclusion criteria for children included taking anti-depressants or anti-anxiety medications, having physical illnesses such as cardiovascular and musculoskeletal disorders, acute and infectious diseases, tuberculosis, noncooperation in home exercises, a history of participating in yoga classes or other complementary therapies in the past year (for both children and parents), and unexpected events during the study such as exacerbation of asthma attacks, the death of the child, parents, or siblings.
After the children were examined by a physician and their clinical condition was confirmed to be stable, the intervention, which consisted of yoga breathing exercises, was individually taught to the children and their parents by the researcher in a room near the examination area. The researcher encouraged both children and parents to perform the breathing exercises in her presence. The duration of training varied from 45 to 60 minutes. To prevent anxiety and boredom in the children, the researcher organized the sessions so that the children could rest and play during the exercises. Following the training, parents and children were advised to repeat these exercises twice a day at home (in the morning and evening) for 10 - 15 minutes each time, with each yogic breathing exercise lasting approximately 30 - 45 seconds. They were also provided with a booklet on yoga breathing exercises. During the subsequent clinic visit after 2 weeks, children were assessed for exercise performance, and if a child did not perform the exercises correctly, the researcher provided further instruction. Over the 2-month follow-up period, the researcher regularly communicated with the parents via phone to ensure that the children were consistently performing the exercises at home. Children and parents were also asked to document the frequency and timing of exercises daily using a provided form. It is important to note that both groups received medical treatment from a physician. The control group did not receive any yoga intervention and solely received medical treatment. The breathing exercises encompassed the following techniques:
- Yogic Complete Breathing: This technique comprises 3 types of breathing: (1) Abdominal, (2) intercostal, and (3) clavicle. It starts with a deep, extended exhalation to empty the lungs as much as possible. Next, the abdominal muscles are extended, and inhalation continues with the intercostal muscles, allowing the chest to move forward and upward. Inhalation continues until the shoulders move up and slightly back. The breath is briefly held before being exhaled. During exhalation, the abdominal wall slowly contracts, followed by the chest, and finally, the shoulders and neck muscles are relaxed.
- Nadi Shodhana Breathing: This method facilitates the rinsing and cleansing of the airways and increases physical energy. The left nostril is completely blocked using the little and ring fingers of the right hand, and inhalation is gradually and continuously completed through the right nostril. At the end of inhalation, the right thumb blocks the right nostril, and exhalation is gradually and continuously completed through the left nostril. At the end of exhalation, when the lungs are empty, a deep and slow inhalation is performed again through the left nostril. At the end of inhalation, the little and ring fingers block the left nostril, and exhalation is completed through the right nostril.
- Kapalabhati Breathing: This technique is recommended for cleaning the airways and sinuses. In Kapalabhati breathing, inhalation is performed slowly, and then during exhalation, the air is expelled from the nose rapidly (in a blowing manner) while the abdominal muscles contract sharply inward. After the explosive exhalation, the abdominal muscles are released, allowing for spontaneous inhalation (25).
3.1. Study Instruments
The instruments employed in this study included a demographic and disease information form, as well as the Persian version of the Pediatric Quality of Life Inventory 3.0 (PedsQL3.0) Asthma Module. These instruments were completed by children with the assistance of their parents both before and 8 weeks after the intervention. The PedsQL3.0 Asthma Module assesses the health-related quality of life in children with asthma through 4 subscales: asthma symptoms (11 items), treatment problems (11 items), worry (3 items), and communication (3 items). The score for each subscale is calculated by summing up the scores of the items within that specific subscale. The total score is determined by summing up the scores of all 4 subscales. All items are scored in reverse, with 'never' receiving a score of 100, 'rarely' 75, 'sometimes' 50, 'most of the time' 25, and 'always' 0. A higher score indicates a better quality of life. This questionnaire was developed and standardized by Varni et al. to measure the quality of life in children with asthma. Varni et al. reported internal consistency values for the entire scale, asthma symptoms, treatment problems, worry, and communication to be 0.71, 0.85, 0.58, 0.72, and 0.70, respectively (26). In a study by Khoshkhui et al., the English version of the PedsQL3.0 Asthma Module was translated into Persian, and its validity and reliability were assessed. The results of their study demonstrated good psychometric properties for this scale. Specifically, the internal consistency of all subscales was confirmed, with a Cronbach's alpha coefficient greater than 0.7. Additionally, construct validity was evaluated through factor analysis (27).
3.2. Statistical Analysis
Demographic and disease information between the intervention and control groups was compared using the chi-square test and independent t-test. The independent t-test was utilized to compare the quality of life scores between the 2 groups before and after the intervention, as well as to compare the mean differences between the intervention and control groups. The paired samples t-test was employed to compare the quality of life scores within each group before and after the intervention in both the intervention and control groups. Data normality was assessed using the Kolmogorov-Smirnov test, which indicated a normal distribution for all data. The data were analyzed using SPSS v. 16 (SPSS Inc., Chicago, IL, USA).
4. Results
Data from 84 children with asthma were analyzed, and the demographic and disease information of the samples is presented in Table 1. There was no significant difference between the 2 groups in terms of sex, age, asthma severity, and the duration since asthma diagnosis (in years).
| Demographic and Disease Information | Intervention (n = 42) | Control (n = 42) | P-Value |
|---|---|---|---|
| Sex | 0.80 b | ||
| Male | 32 (76.2) | 31 (73.8) | |
| Female | 10 (23.8) | 11 (26.2) | |
| Severity of asthma | 0.80b | ||
| Mild persistent | 30 (71.4) | 31 (73.8) | |
| Moderate persistent | 12 (28.6) | 11 (26.2) | |
| Age (y) | 8.42 ± 1.96 | 8.11 ± 1.8 | 0.45 c |
| The period since asthma diagnosis (y) | 5.14 ± 2 | 4.89 ± 2.6 | 0.64 c |
a Values are expressed as mean ± standard deviation or No. (%).
b P-value is calculated by chi-square test between groups.
c P-value is calculated by independent t-test between two groups.
As shown in Table 2, there was no statistically significant difference in the total mean score of quality of life between the intervention and control groups before the intervention (P = 0.29). However, after the intervention, a statistically significant difference was observed in the total mean score of quality of life between the 2 groups (P = 0.003). After the intervention, the mean scores of the 2 subscales, symptoms and treatment problems, were significantly different between the 2 groups, while the mean scores of the other 2 subscales, worry and communication, were not significantly different (P = 0.057). Table 3 illustrates that the mean differences in quality of life were 10.4 ± 10.3 in the intervention group and 0.69 ± 7.8 in the control group. The changes were significantly higher in the intervention group than in the control group (P < 0.001).
| Quality of Life (Subscales) and Stages of Intervention | Groups | P-Value b | Effect Size (d) c | |
|---|---|---|---|---|
| Intervention (n = 42) | Control (n = 42) | |||
| Asthma symptoms | 0.77 | |||
| Before | 61.5 ± 12.9 | 63.2 ± 11.2 | 0.50 | |
| After | 75.1 ± 10.3 | 66.7 ± 11.4 | 0.001 | |
| Treatment problem | 0.9 | |||
| Before | 72.3 ± 15.6 | 75.8 ± 13.8 | 0.28 | |
| After | 82 ± 9.6 | 72.5 ± 11.4 | < 0.001 | |
| Worry | 0.32 | |||
| Before | 62.1 ± 24.4 | 63.4 ± 25.5 | 0.80 | |
| After | 77.7 ± 14.8 | 71.6 ± 22 | 0.13 | |
| Communication | 0.19 | |||
| Before | 80.1 ± 24.9 | 85.5 ± 17.5 | 0.80 | |
| After | 82.9 ± 14.7 | 79.9 ± 16 | 0.29 | |
| Quality of life (total) | 0.62 | |||
| Before | 69 ± 13.6 | 72 ± 12.2 | 0.29 | |
| After | 79.4 ± 9.1 | 72.7 ± 11.1 | 0.003 | |
a Values are expressed as mean ± standard deviation.
b P-value is calculated by an independent t-test between two groups.
c Cohen effect size: d = 0.2 'small' effect size, d = 0.5 'medium' effect size, and d = 0.8 a 'large' effect size.
| Quality of Life (Subscales) | Groups | P-Value b | |
|---|---|---|---|
| Intervention (n = 42) | Control (n = 42) | ||
| Asthma symptom | 13.62 ± 8.4 | 3.4 ± 9.4 | 0.001 |
| Treatment problem | 9.7 ± 12.9 | -3.2 ± 10.2 | 0.001 |
| Worry | 15.6 ± 21.3 | 8.1 ± 21.1 | 0.10 |
| Communication | 2.7 ± 19.3 | -5.5 ± 11.8 | 0.02 |
| Quality of life (total) | 10.4 ± 10.3 | 0.69 ± 7.8 | 0.001 |
a Values are expressed as mean ± standard deviation.
b P-value is calculated by independent t-test between two groups.
5. Discussion
This study aimed to determine the effect of yoga breathing exercises on the quality of life of children aged 5 - 11 years with asthma. Our study demonstrated that breathing exercises, including yogic complete breathing, Nadi Shodhana, and Pranayama breathing for 10 - 15 minutes twice a day over 8 weeks, improved the quality of life of children in the intervention group, possibly by modifying their breathing patterns. These results align with those of previous studies. For instance, Yadav et al. reported that yoga improved pulmonary function tests and overall quality of life in 140 children aged 10 - 16 years (28). Gupta et al. found that yoga/pranayama breathing exercises as a complementary therapy for 6 weeks improved pulmonary functions in children aged 8 - 14 years (29). Additionally, Pandya indicated that after implementing a yoga education program, children in the intervention group exhibited better asthma control, with lower average pediatric asthma diary (PAD) scores and higher childhood asthma control test (C-ACT) scores compared to the control group (P = 0.00) (30).
Since studies on the effect of yoga on the quality of life in children are limited, it is worth mentioning studies conducted on adults. In a Cochrane review by Yang et al., which included evidence from 15 randomized controlled trials (RCTs) and 1 048 participants, it was found that yoga may improve the quality of life and asthma symptoms (31). Another study by Sodhi et al. involved 120 patients with asthma aged 17 - 50 years, who were randomly divided into group A (yoga group) and group B (control group). Both groups received prescribed medications, while the yoga group practiced yoga breathing exercises for 45 minutes a day for 8 weeks. The results revealed that pranayama yoga breathing exercises improved the "symptoms," "activities," and "environmental" subscales of the Asthma Quality of Life Questionnaire (AQLQ) (32). Jasrotia and Kanchan found that practicing yoga for 45 minutes every day for 3 months resulted in improved pulmonary function in children (33).
In conclusion, based on the results of our study and other referenced studies, it appears that yoga can enhance the quality of life in children by modifying breathing patterns through breathing-regulating mechanisms.
Our study revealed that yoga improved the physical domains of quality of life, specifically symptoms and treatment problems, but did not have a significant impact on the psychological domains, including communication and worry. These findings are consistent with those reported by Yadav et al. and Sodhi et al., where yoga did not show improvements in the emotional subscale (28, 32). Stress and anxiety are common symptoms in children with asthma, which can significantly affect their quality of life. Children with asthma face both physiological stressors, such as wheezing, chest tightness, and coughing during asthma exacerbations, as well as psychological stressors, like feeling different from their classmates, having to use medications, and being hospitalized. Stress can exacerbate asthma by triggering inflammatory responses (34). While we did not find any studies specifically investigating the effect of yoga on psychological aspects like stress and anxiety in children with asthma, a study conducted on healthy school-aged girls demonstrated that yoga helped reduce stress and enhance coping skills (35). Therefore, further research in this area is warranted.
Our results differ from a study by Karam et al., in which a combined respiratory training program, including yoga pranayama techniques, diaphragmatic breathing, and pursed-lip breathing for 10 minutes a day for 1 month, improved asthma control and daily activities and reduced the use of inhalers in patients with persistent asthma aged 18 - 65 years. However, the quality of life was not significantly improved in their study (17). It is possible that longer and more frequent exercise may be necessary to enhance the quality of life, as we observed in our study, where children practiced the exercises for 2 months twice a day. In our study, parents did not report any side effects during or after the yoga exercises, confirming the safety of yoga for children. The researcher who taught the children had completed a yoga training course under the supervision of an instructor from the Sports Federation and received a certificate. Saoji et al. similarly reported that yoga exercises are safe and harmless when practiced under the guidance of a trained coach (36).
The clinical implication of our study is that yoga breathing exercises offer a safe, easy, and cost-effective approach to managing asthma in children. Children with asthma can benefit from these interventions, leading to improved asthma symptoms, reduced school absenteeism, and cost savings related to medication, emergency department visits, hospitalizations, and missed workdays for parents. Additionally, based on our findings, pediatric nurses can play a crucial role in teaching and implementing yoga as a complementary therapy alongside prescribed medications in children with asthma under the supervision of a physician.
Every research study has its limitations. One limitation of our study was the nonrandom allocation of samples to the 2 groups. Since the patients were selected from 1 hospital, we allocated them to the intervention and control groups on separate days to prevent potential information sharing among families. Another limitation was the inclusion of only children with mild to moderate asthma due to concerns about potential complications in severe asthma cases. Consequently, our results may not be applicable to children with severe asthma.
5.1. Conclusions
Yoga breathing exercises demonstrated an improvement in the quality of life among children with asthma. These exercises were also found to be safe for children. Yoga is recommended as a complementary and alternative treatment to enhance the quality of life as a component of childhood asthma management. Further research is required to precisely determine the effects of yoga interventions for children and adolescents with asthma.