1. Background
Proper nutrition and nutritional support are among the important aspects of patient care and treatment, especially in those hospitalized in intensive care units (ICUs), who need different strategies to achieve optimal nutritional status. Nutritional therapy should be considered in patients with malnutrition at the time of the onset of mechanical ventilation (MV). Appropriate and timely nutritional support improves the desired outcomes in patients hospitalized in ICUs. (1). There is evidence that the gavage solution prepared in the hospital is not enough to provide the energy and protein needed by patients, and these solutions should be prepared in such a way that they have acceptable or standard carbohydrates, lipids, and proteins (2).
The nutritional needs of patients in ICUs, including energy, are higher than other patients, so malnutrition will be inevitable if proper nutritional care is not provided to them (3). Disease-related malnutrition has detrimental effects on the treatment process and causes an increase in the rate of infections, delayed recovery, prolonged hospital stays, and elevated risk of mortality (4). Various biomarkers, such as low levels of albumin and other plasma proteins, as well as anthropometric measures, such as weight, height, and BMI, are used to define nutritional risk. However, whether or not these biomarkers are directly related to nutritional risk is questionable (5). On the other hand, excessive amounts of nutrients can cause complications such as hyperglycemia, hyperlipidemia, and increased CO2 production, leading to the prolongation of MV (6).
Patients admitted to the ICU present a heterogeneous population suffering from different diseases with varying severities (7). Mechanical ventilation is one of the most common supportive measures delivered to patients with critical conditions during medical care. About 40% of those hospitalized in the ICU require respiratory support with MV (8, 9). Annually, more than 20 million people need admission to the ICU and become dependent on MV (10). Studies show an incidence of up to 60% of malnutrition in patients hospitalized in the ICU, which is considerably higher than in other patients (7).
Long-term ventilation is associated with increased length of hospital stay, hospital costs, and side effects (11). Shortening the hospital stay and dependence on MV in the ICU can significantly help reduce healthcare costs (12). Timely and successful extubation is particularly important to prevent adverse outcomes in the ICU, and early separation of the patient from the MV device can be catastrophic (11), highlighting the role of correct and timely decision-making by nurses in accelerating the patient’s treatment progress, taking better care of them, and reducing hospital costs (13).
In a cohort study assessing the effects of nutritional factors on the duration of MV in critically ill patients, Koontalay et al. showed that nutritional status monitoring and the provision of required calories had a statistically significant positive relationship with the duration of MV (14). Although nutritional support is essential for patients admitted to ICUs, the optimal energy required by them remains unclear (15).
Nurses, as the most important individuals in ICUs, have a key role in starting the process of weaning the patient from the MV device. Studies have shown that nurses can effectively and safely prepare patients for being separated from mechanical ventilators, invoking appropriate tools and protocols (16).
2. Objectives
The primary objective of our study was to determine the effect of the planned use of a standard Entera Meal solution on the duration of weaning patients from MV and the average length of ICU stay. The secondary objective was to determine the effect of scheduled feeding on serum albumin levels in patients admitted to the ICU.
3. Methods
3.1. Study Design, Setting, and Definitions
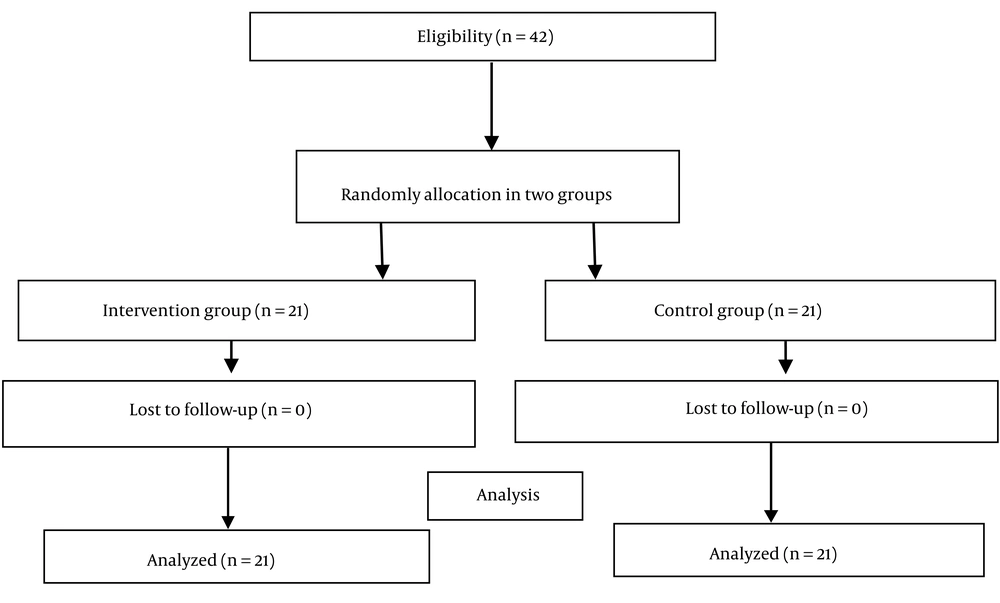
This single-blinded clinical trial was conducted employing a pretest-posttest design and registered at the Iranian Registry for Clinical Trials under the trial registration number IRCT20200813048398N1 on 2020-08-22. The patients admitted to the ICUs of the Imam Khomeini and Golestan hospitals of Ahvaz city, Iran were enrolled. The sample size was calculated according to the results of Jalalian et al.’s study (17), considering the alpha of 5% and beta of 20% and including 10% attrition, using the relevant formula. The sample size in each group was calculated as 21 people.
The study subjects (N = 42) were selected out of patients admitted to ICUs and met our inclusion criteria (i.e., hospitalization in the ICU up to 24 hours after admission to the hospital, age of 18 - 65 years, feeding through an NG tube, being under MV for more than 24 hours, not being pregnant or obese (a body mass index above 40 kg/m2), no liver disease, and no severe infection. Exclusion criteria were a change of feeding type from gavage to complete intravenous feeding and being transferred or discharged from the ICU (Figure 1). Primary outcomes were the duration of connection to the ventilator and the length of ICU stay, and the secondary outcome was serum albumin level.
In order to start the study, informed consent was obtained from the legal guardians of the patients who met the study’s entry criteria. Then, a history was taken from the patients, and a physical examination was performed by an ICU resident specialist. Medical information and patient records were obtained from the notions provided by the treatment team and by reviewing patients' files and recorded in a questionnaire and a checklist. Using a table of random numbers, the participants were randomly assigned to the intervention and control groups. The order of gavage was determined by the attending physician, but its content and amount were determined by a nutritionist.
In the intervention group, a standard Entera Meal solution, the product of Karen’s Pharmaceutical and Vital Food Supplements Company (Iran), was administered as the source of energy. The product was in the powder form, weighing 400 g, and contained 14% energy from a protein with a high biological value (whey) and milk, 32% energy from sunflower and coconut oils (source of MCT), 54% energy from Gluten-free low-lactose carbohydrates (maltodextrin), vitamins, minerals with enzyme complexes, and inulin.
To prepare 150 mL of the solution, 33 g (1 cup) of Entera Meal was added to 120 mL of chilled boiled water, creating a solution with 1 kcal energy per mL. To calculate the energy requirement of the patient, the patient’s ideal weight was determined. For patients appearing to have normal weight, the height was inserted into the formula used for BMI calculation; the BMI value was considered equal to 23 kg/m2, and the ideal weight was calculated. For patients appearing thin, BMI was equal to 18.5 kg/m2, and for those appearing fat, BMI was equal to 25 kg/m2. Accordingly, the energy required was determined. The amount of energy equivalent was considered to be 25 kcal per kg of the body weight for the first week and 30 kcal per kg of the body weight for the second week. Blood albumin levels were measured in both study groups before and after the intervention.
In the control group, a homemade solution prepared in the hospital’s kitchen was used without further interference or processing. Feeding was performed using an NG tube by the bolus infusion method and a 60-mL syringe. The feeding was started with 50 mL and increased up to 30 mL every three hours (6, 9, 12, 15, 18, and 21 hours) to reach the calculated energy within 48-72 hours. Serum albumin level was measured and analyzed before the intervention and at the end of the study period.
3.2. Data Collection
The data were collected using a demographic and medical information questionnaire, including age, gender, weight, and the type of the underlying disease, as well as a checklist for recording outcomes, including albumin level at the beginning and end of the study, the duration of the patient’s separation from the mechanical ventilator, and length of ICU admission. The validity of the questionnaire and the checklist was confirmed by 15 nursing faculty members.
3.3. Statistical Analysis
Data analysis was conducted using SPSS software version 22. Quantitative variables were reported as mean, and standard deviation, and qualitative variables were reported as frequency and percentage. The independent t-test was used to compare means between the study groups (for data with normal distribution), and the non-parametric Mann-Whitney U test was used for this purpose for variables with non-normal distribution. The chi-square or Fisher’s exact tests were used to compare the distribution of nominal variables between the two groups. In order to compare the means of continuous quantitative variables, first, their normality was checked using the Kolmogorov-Smirnov test, indicating that age and weight had normal distributions in both groups, but other variables (length of ICU hospitalization and serum albumin level before and after the intervention) had non-normal distribution.
4. Results
4.1. Patient Characteristics and Clinical Data
In this clinical trial, 42 eligible people were studied in 2 groups of 21 people. Of the 42 participants in this study, 28 were male, and 14 were female. Hospitalization reasons included head trauma (15, 35.71%), spinal cord injury (6, 14.29%), intracerebral brain hemorrhage (ICH) (6, 14.29%), acute respiratory distress syndrome (ARDS) (7, 16.67%), and cerebral vascular accident (CVA) (8, 19.05%). There was no significant difference in gender distribution between the two groups. The mean ages of the participants in the intervention and control groups were 42.28 ± 12.53 and 54.71 ± 9.21 years, respectively, and this difference was statistically significant (P = 0.001). The mean weight was 77.71 ± 11.10 kg in the intervention group and 74.04 ± 16.63 kg in the control group, but this difference was not statistically significant between the two groups. Underlying diseases did not show a significant difference between the two groups (Table 1).
a Values are expressed as mean ± SD or No. (%).
b Independent t-test
c Chi squared
4.2. Outcomes
The means of the length of ICU stay and serum albumin level before and after the intervention in the two groups have been presented in Table 2. The results showed that the administration of the planned Entera Meal solution significantly reduced the length of ICU stay in the intervention group (9.47 ± 6.72 days) compared to the control group (16.23 ± 8.32 days) (P = 0.004, Table 2).
Abbreviation: ICU, intensive care unit.
a Values are expressed as mean ± SD.
b Independent t-test
c Mann-Whitney test
At the post-test, serum albumin level was slightly higher in the intervention group than in the control group (3.77 ± 0.41 vs. 3.73 ± 0.41 mg/dL), but this difference was not statistically significant (P = 0.42) (Table 2).
Although the duration of patient disconnection from mechanical ventilation was shorter in the intervention group than in the control group, this difference was not statistically significant (5.23 ± 4.77 vs. 7.71 ± 6.14 days, P = 0.15) (Table 2).
Since there was a significant difference between the two studied groups in terms of age, this variable was analyzed in the subcategories of > 50 and < 50 years (Table 3).
| Variables | Duration of Weaning Patients (day) | Length of Stay ICU (day) | Serum Albumin (Pre-test, mg/dL) | Serum Albumin (Post-test, mg/dL) |
|---|---|---|---|---|
| ≤ 50 (year), n = 21 | ||||
| Intervention group | 4.37 ± 2.73 | 8.37 ± 5.07 | 3.69 ± 0.50 | 3.85 ± 0.39 |
| Control group | 7.42 ± 5.50 | 14.71 ± 8.19 | 4.04 ± 1.04 | 3.81 ± 0.25 |
| P-value | 0.40 b | 0.03 c | 0.94 c | 0.06 c |
| > 50 (year), n = 21 | ||||
| Intervention group | 8.00 ± 5.57 | 13.00 ± 10.46 | 3.42 ± 0.22 | 3.50 ± 0.42 |
| Control group | 7.86 ± 4.97 | 17.00 ± 8.35 | 3.44 ± 0.43 | 3.70 ± 0.47 |
| P-value | 0.97 b | 0.63 c | 0.94 c | 0.06 c |
Abbreviation: ICU, intensive care unit.
a Values are expressed as mean ± SD.
b Independent t-test
c Mann-Whitney test
As shown in Table 3, the length of ICU hospitalization was significantly shorter in the younger (≤ 50 years) patients of the intervention group compared to the control group (P = 0.03). In people with age ≤ 50 years, average serum albumin level did not show any significant difference before and after the intervention in both study groups. The mean duration of weaning from the ventilator was 5.9 days in patients equal to or younger than 50 years and 7.9 days in those older than 50 years; however, there was no significant relationship between age and the duration of weaning from the ventilator (Table 3). In people over 50 years of age, there was no significant difference between the two groups regarding the means of the studied variables.
5. Discussion
Previous studies have shown that nutritional support is essential for patients under mechanical ventilation. These patients need a regular nutritional program to respond to their energy requirements, as well as to maintain and strengthen their muscles in order to bring forward weaning from MV and reduce the length of ICU admission (14). The respiration process is affected by malnutrition, which affects the structure, elasticity, and function of the lungs, as well as the mass, strength, and endurance of the muscles involved in this process, wasting muscle strength and increasing muscle fatigue (18). However, only low-quality evidence supports the beneficial effects of nutritional support on the mortality rate and the occurrence of serious adverse events in critically ill patients hospitalized in the ICU (5).
In the present study, to clarify the clinical controversies over the role of nutritional support in the outcomes of patients under mechanical ventilation, we investigated the effects of a standard Entera Meal solution on the duration of MV support of patients and their length of hospitalization in the ICU. A comparison of the duration of weaning patients from the ventilator did not show a significant difference between the two study groups; however, this parameter was shorter in the intervention group than in the control group. In a retrospective analytical study on patients under MV, no significant relationship was reported between the nutritional status and the time of separation of patients from MV, suggesting a need for clinical trials in this field to clarify this observation (19).
In a retrospective analytical study in South Korea evaluating the clinical factors predicting weaning failure in patients undergoing MV in the ICU, Shin et al. reported that patients for whom weaning failed were older than those whose weaning was successful. This observation was not in line with the results of the present study, probably due to the difference in methodology, as well as different reasons for which the patients were admitted to the ICU (i.e., most patients in the Shin et al.’s study suffered from respiratory and then cardiac problems; diseases that are significantly associated with increasing age) (20). In the present study, neither age nor gender was significantly associated with the duration of patient disconnection from the mechanical ventilator, which was consistent with the findings of a study by Jalalian et al. (17).
The comparison of the mean length of ICU admission between the two intervention and control groups showed a statistically significant difference. The results of a study by Ostadrahimi et al. on the effect of nutritional support on the length of hospitalization in the victims of traffic accidents admitted due to burns showed that the average length of hospital stay was shorter in patients who consumed standard commercial food than in those who received the hospital’s routine diet (21).
We noticed that among patients younger than 50 years of age, the length of ICU hospitalization was significantly shorter in the intervention group compared to the control group. According to the results of this study, men experienced a shorter length of ICU admission compared to women, which was consistent with the results of a study by Ghanbari et al. (22) but disagreed with the findings of Huang’s study (23). Ma et al. also reported that the duration of MV and the length of ICU hospitalization of younger patients were significantly longer in men than in women, and male gender was independently associated with in-hospital mortality in older patients (24).
Serum albumin level is one of the valuable indicators in predicting the recovery or deterioration of a patient’s health status. Low serum albumin levels may play a role in predicting the recovery or worsening of the condition of patients with serious diseases, and hypoalbuminemia is considered an indication for starting medical treatment (25). The results of the present study showed no statistically significant difference in the serum albumin levels between the intervention and control groups at the end of the study.
5.1. Limitations
The limitations of this study include failure to assess disease severity and a small sample size that may not be representative of all ICU-admitted patients. It is suggested to conduct further studies with larger sample sizes and analyze the underlying causes of ICU admission, as well as the disease severity score (Apache score) and the GCS level.
5.2. Conclusions
The results of this study showed that nutritional support with a standard Entera Meal solution, compared to a routine hospital diet, increased serum albumin levels and shortened the length of ICU hospitalization in patients under the age of 50 years old. However, this nutritional intervention had no significant effect on shortening the duration of connection to a mechanical ventilator in patients hospitalized in the ICU.