1. Background
The COVID-19 pandemic has caused widespread distress and mental disorders in society, in addition to causing numerous deaths (1-3). The fear and anxiety resulting from the spread of the infection are common and understandable reactions that anyone, regardless of social class, age group, or gender, can experience (4). Adolescents, who are undergoing a challenging phase of life, are among the most vulnerable groups affected by the COVID-19 pandemic (2, 3, 5). Adolescence is marked by significant physical, mental, and social changes and represents a critical period in an individual's life that lays the foundation for mental health in adulthood. During this period, individuals undergo extensive cognitive, neurological, biological, and psychosocial changes (6, 7). With the outbreak of COVID-19 and its rapid spread in Iran, leading to general quarantine, teenagers shifted to online education, and all activities were confined to the home, isolated from society.
Fears of contracting the disease or loved ones becoming infected, the dread of death, travel restrictions, diminished social interactions, feelings of hopelessness, boredom, frustration, economic concerns, stress about the family's financial future, acute and chronic stress, depression, limitations on physical and social activities due to home quarantine, abrupt lifestyle changes, prolonged school closures, and many other stressors are currently affecting adolescents' health, mental well-being, and adaptability (3, 8), casting a shadow over these aspects of their lives (1). An increase in anxiety levels is one of the most significant negative psychological impacts of the pandemic (8, 9). COVID-related anxiety, stemming from the possibility of infection and fear of the unknown, can weaken the immune system, increasing susceptibility to diseases like COVID-19 (9). Adolescents with chronic diseases are particularly vulnerable and at higher risk of contracting the disease (6). The presence of any disease, especially chronic conditions, can exacerbate the challenges of this life stage and significantly affect adolescents’ health (10).
Throughout life, individuals undergo numerous changes and transformations that can precede various mental problems and disorders (11). Spirituality and personal beliefs play a crucial role in helping individuals cope with difficulties and imbue their lives with meaning (12). Spiritual health, a personal aspect of health, is related to the concept of self-transcendence, reflecting an individual's value system and possibly connected to belief in supernatural or natural phenomena (13). Numerous studies have shown that spiritual health can mitigate adverse conditions in difficult times, and the spread of diseases, as in the current situation, can benefit from the positive influences of this fundamental factor (14). The findings from the study by Khairy et al. suggest that cancer patients exhibit high levels of spiritual health. Results from many studies have demonstrated that individuals and patients with spiritual health lead healthier lifestyles, are more hopeful, possess greater psychological stability, and are more satisfied with their lives (15).
Despite extensive research on spiritual health across various age groups, including adolescents with chronic diseases, there has been no study on the impact of the coronavirus pandemic on the spiritual health of adolescents with chronic diseases in Iran, especially when compared to the mental health of healthy adolescents.
2. Objectives
Therefore, this study aims to assess and compare spiritual well-being and the anxiety caused by the COVID-19 pandemic among healthy adolescents and those with chronic diseases.
3. Methods
3.1. Study Design and Participants
This study is a comparative descriptive investigation targeting two groups of adolescents aged 15 to 19 years. The first group comprised adolescents with chronic diseases such as cancer, diabetes mellitus, advanced respiratory diseases (including bronchiectasis, cystic fibrosis, tuberculosis, asthma, and chronic obstructive pulmonary diseases), and autoimmune diseases (such as lupus and rheumatoid arthritis) who were hospitalized in various departments of educational hospitals or attended oncology, respiratory, rheumatology, and endocrinology clinics in Tehran, Iran, from January to April 2021. The second group consisted of adolescents without chronic diseases, specifically students from public high schools in Tehran, who were confirmed to be disease-free according to the school's health records. Inclusion criteria for adolescents with chronic diseases were the absence of mental illness according to self-report, having a known chronic illness for at least 6 months as per medical records, and not being in the terminal stages of the disease. For adolescents without chronic diseases, the criteria included no mental disorders based on self-report and no chronic illnesses. The sample size was determined with an alpha error probability of 0.05 and a power of 0.95 using the following sample size formula:
Sampling among adolescents with chronic diseases was conducted using a convenience sampling method, focusing on those attending Mofid Hospital, one of the largest specialized educational and therapeutic centers for children and adolescents (85 individuals). Sampling from the population of adolescents without chronic diseases involved cluster and random sampling from high schools in one of Tehran's educational districts. Each school was considered a cluster, and participants were randomly selected using a table of random numbers based on the number of students in each school who met the study's entry conditions (80 individuals).
After the selection and pairing of groups, sampling permission was obtained from the hospital and schools. Written informed consent was collected from both the adolescents and their parents. Printed questionnaires were then distributed in person, and necessary instructions for completion were provided. The questionnaires were collected after being completed.
3.2. Instruments
The tools for data collection included a demographic characteristics questionnaire, the Paloutzian & Ellison Spiritual Well-Being Scale (SWBS), and the Corona Disease Anxiety Scale (CDAS).
3.2.1. The Demographic Characteristics Questionnaire
The demographic characteristics questionnaire includes information about age, gender, school grade, father's job, mother's job, type of chronic disease, the adolescent’s sources of information about the coronavirus, history of contracting the coronavirus by the adolescent and their family members, and fatal cases in the family due to the coronavirus.
3.2.2. The Paloutzian & Ellison Spiritual Well-Being Scale
The SWBS from 1991 was used to measure spiritual health in both healthy adolescents and those with chronic diseases. This scale consists of 20 items across two dimensions: Religious health and existential health, with each dimension comprising 10 items. Responses are scored on a 6-point Likert scale, ranging from strongly disagree to strongly agree (1 to 6 points). The overall SWBS score, a sum of the scores from both subcategories, ranges from 20 to 120. The scores are classified as follows: 20 - 40 indicates poor spiritual health, 41 - 99 indicates moderate spiritual health and 100 - 120 indicates high spiritual health. Paloutzian and Ellison reported the reliability of this test, as measured by Cronbach's alpha, to be 0.82 (16, 17). In the study conducted by Rezaei et al., the SWBS's validity was established through content validity, and its reliability was confirmed with a Cronbach's alpha coefficient of 0.82 (18, 19).
3.2.3. Corona Disease Anxiety Scale
The CDAS was utilized to assess anxiety related to the coronavirus. Developed by Alipour et al. during the COVID-19 pandemic, this scale comprises 18 items divided into two components: Items 1 to 9 assess mental symptoms, and items 10 to 18 assess physical symptoms. Responses are scored on a 4-point Likert scale (never = 0, sometimes = 1, often = 2, always = 3). The total score for this questionnaire can range from 0 to 54, with higher scores indicating greater levels of COVID-related anxiety. The reliability of this instrument has been confirmed with a Cronbach's alpha of 0.919 for the entire questionnaire, 0.870 for the first component, and 0.861 for the second component. The validity of the questionnaire has been supported through both exploratory and confirmatory factor analysis (9).
In this study, the qualitative content validity of these scales was evaluated, and their reliability was assessed using the internal consistency method (Cronbach’s alpha), which resulted in scores of 0.87 for religious health, 0.9 for existential health, 0.87 for mental and physical anxiety, and 0.89 for the overall scale, respectively.
3.3. Statistical Analysis
Data normality was assessed using the Kolmogorov-Smirnov test. The analysis was conducted using independent t-tests and Mann-Whitney tests for non-normal data, utilizing SPSS 22 software.
4. Results
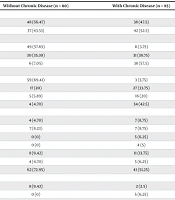
The analysis included 165 completed questionnaires from 80 adolescents without chronic diseases and 85 adolescents with chronic diseases. Of all participants, 47.8% were girls; 13.9% of participants and 47.9% of their family members had contracted the coronavirus. Fatal cases due to the disease were reported at 23%. Other demographic characteristics are presented in Table 1.
| Variables | Without Chronic Disease (n = 80) | With Chronic Disease (n = 85) |
|---|---|---|
| Gender | ||
| Male | 48 (56.47) | 38 (47.5) |
| Female | 37 (43.53) | 42 (52.5) |
| Age (y) | ||
| 14 - 15 | 49 (57.65) | 11 (3.75) |
| 16 - 17 | 30 (35.30) | 31 (38.75) |
| 18 - 19 | 6 (7.05) | 38 (57.5) |
| Grade | ||
| 9th | 59 (69.41) | 3 (3.75) |
| 10th | 17 (20) | 27 (33.75) |
| 11th | 5 (5.89) | 16 (20) |
| 12th | 4 (4.70) | 34 (42.5) |
| Father’s field of work | ||
| Education | 4 (4.70) | 7 (8.75) |
| Economy | 7 (8.23) | 7 (8.75) |
| Medicine/health | 0 (0) | 5 (6.25) |
| Psychology | 0 (0) | 4 (5) |
| Industry/business | 8 (9.42) | 11 (13.75) |
| Management | 4 (4.70) | 5 (6.25) |
| Others | 62 (72.95) | 41 (51.25) |
| Mother’s field of work | ||
| Education | 8 (9.42) | 2 (2.5) |
| Medicine/health | 0 (0) | 5 (6.25) |
| Psychology | 2 (2.35) | 4 (5) |
| Industry/business | 0 (0) | 1 (1.25) |
| Management | 2 (2.35) | 0 (0) |
| Housewife | 67 (78.83) | 64 (80) |
| Others | 6 (7.05) | 4 (5) |
| Type of chronic disease | ||
| Cancer | 47 (55.29) | - |
| Diabetes mellitus | 25 (29.41) | - |
| Advanced respiratory diseases | 5 (5.89) | - |
| Autoimmune diseases | 8 (9.41) | - |
Demographic and Clinical Characteristics of the Participants (n = 165) a
Based on the results, the adolescents participating in this study demonstrated moderate spiritual well-being, with an average score of 86.10 ± 1.70. The mean scores for the dimensions of “religious health” and “existential health” were 45.48 ± 0.92 and 40.61 ± 0.87, respectively. The comparison of mean scores of spiritual well-being between the two groups revealed that adolescents without chronic diseases had significantly higher levels of spiritual health compared to those with chronic diseases. This finding was consistent across both dimensions of spiritual well-being (Table 2).
| Spiritual Well-being Scale | Adolescents Without Chronic Disease | Adolescents with Chronic Disease | P-Value b |
|---|---|---|---|
| Religious health | 51.25 ± 9.13 | 40.05 ± 11.56 | 0.000 |
| Existential health | 45.42 ± 9.02 | 36.09 ± 11.26 | 0.000 |
| Spiritual well-being | 96.67 ± 16.62 | 76.15 ± 21.58 | 0.000 |
The Mean Score of Spiritual Well-being and Its Dimensions Among Adolescents with and Without Chronic Disease a
Overall, the participants exhibited low levels of COVID-related anxiety, with an average score of 16.19 ± 0.81. The mean score for the “mental anxiety” dimension was 11.60 ± 0.47, while the “physical anxiety” dimension scored an average of 4.58 ± 0.41. Moreover, when comparing the overall mean scores of COVID-related anxiety between the two groups, it was found that adolescents without chronic diseases experienced lower levels of COVID-related anxiety (Table 3).
| Corona Disease Anxiety Scale | Adolescents Without Chronic Disease | Adolescents with Chronic Disease | P-Value b |
|---|---|---|---|
| Mental anxiety | 9.56 ± 4.90 | 13.52 ± 6.42 | 0.000 |
| Physical anxiety | 2.43 ± 2.74 | 6.61 ± 6.21 | 0.000 |
| Corona disease anxiety | 12.00 ± 6.79 | 20.14 ± 11.72 | 0.000 |
The Mean Score of COVID-Related Anxiety and Its Dimensions Among Adolescents with and Without Chronic Disease a
5. Discussion
The findings of this study indicate that the participating adolescents had moderate spiritual well-being, with those without chronic diseases displaying significantly higher levels of spiritual health than their counterparts with chronic diseases. These results align with the findings of Taheri et al., who reported an average spiritual well-being score of 74.2 among adolescents with chronic diseases, and 84% of them had moderate spiritual health. Furthermore, this study found no statistically significant relationship between spiritual well-being and factors such as age, gender, and economic status (20). Ahmadpoori and Motaghi also researched the spiritual health of adolescent students and found their spiritual well-being, including existential and religious health dimensions, to be at a moderate level, corroborating the findings of the current study (18). The use of the same questionnaire across these studies facilitates the comparison of results.
The study by Rubin et al. found no difference in the spiritual well-being of adolescents with chronic diseases compared to healthy adolescents, which contrasts with the findings of the current study (21). Leung et al. assessed the spiritual health of end-of-life cancer patients and found it to be high (22). This may be attributed to the chronic nature of cancer, the different life cycles, and the progression of the disease.
Davis et al. observed that during the COVID-19 pandemic, there was little evidence of significant changes in individuals' mental and spiritual health outcomes. It suggests that pandemics like COVID-19 might not markedly affect the spiritual well-being of vulnerable populations, such as those with chronic illnesses, or might even mildly improve their attitudes and spiritual health (23). This could be due to individuals with chronic illnesses already having adapted to challenging conditions, thereby diminishing the pandemic's impact on their spiritual response. This aligns with the current study's findings and other research indicating a relatively stable spiritual well-being in individuals following disasters (24).
Contrary to some studies (25, 26), the current study found that adolescents, both with and without chronic diseases, experienced low levels of COVID-related anxiety. This discrepancy could be due to the timing of the respective studies. Other research has shown adolescents to perceive high levels of COVID-related anxiety, stemming from direct exposure to the disease, school closures, and quarantine measures leading to restricted social interactions and heightened anxiety.
Lavigne-Cervan et al. reported on the effects of COVID-19 restrictions on anxiety, sleep, and performance among children and adolescents in Spain, revealing that 66.9% and 67.9% of adolescents scored moderate to high levels of anxiety, respectively (27). This is in line with Jiao et al., who identified behavioral-emotional disorders among 320 adolescents aged 13 - 18 during the COVID-19 pandemic, noting common issues like attention problems, irritability, fear of discussing the coronavirus, and clinginess (28). Similarly, a study by Cao et al. on university students in China at the onset of the pandemic found that 24.9% of students experienced moderate to severe levels of COVID-related anxiety, with social support inversely related to anxiety levels (P < 0.001), highlighting the importance of monitoring adolescents during COVID-19 to mitigate the risk of mental health issues (29).
Contrarily, the study by Chen et al. found no significant relationship between anxiety and the COVID-19 pandemic, suggesting that the pandemic did not affect participants' anxiety levels. This conclusion diverges from the findings of the current study and others (1). By examining other research (26, 30) in line with the current study's results, it emerges that insufficient information about the new disease and inadequate knowledge regarding appropriate immunization methods tend to heighten anxiety levels. Conversely, increased awareness, participation, and adherence to health protocols among adolescents and their families can reduce anxiety following news related to COVID-19.
Moreover, adolescents without chronic diseases reported higher spiritual health scores and experienced less anxiety, a trend also observed among adolescents with chronic diseases, albeit to a lesser extent. In other words, adolescents with chronic diseases displayed lower spiritual health levels and experienced greater anxiety during the COVID-19 pandemic. A study in Portugal aiming to explore the impact of religious-spiritual compatibility on fear and COVID-related anxiety levels found that participants with higher scores on the spiritual well-being scale reported lower anxiety levels due to coronavirus (31), echoing the findings of the present study. Supporting these results, Nodoushan et al. investigated the link between spiritual health and stress in pregnant women during the COVID-19 pandemic, discovering that spiritual well-being effectively reduces stress during the crisis, potentially influencing factors related to preterm delivery and unhealthy births (32). However, Blumenthal et al. did not establish a significant connection between spiritual health and heart disease, anxiety, or stress (33). The discrepancies among these findings could be attributed to cultural and religious differences across the study populations, individual beliefs, the type of spirituality enhancement programs, and the sample sizes (34).
These studies suggest that in the face of the COVID-19 pandemic, spirituality could serve as a means to promote health, prevent disease spread, and effectively alleviate stress and COVID-related anxiety while fostering hope and tranquility, thereby enhancing immunity against the virus (35, 36). Since spirituality is linked with life stability, wellness, harmony, and a sense of connection to oneself, the divine, society, and the environment, individuals with higher spiritual health levels tend to be more patient and capable of enduring and managing life's challenges. They view problems from different perspectives, which helps in better coordinating the body's internal mechanisms and reducing dysfunctional thoughts and anxiety compared to those with lower levels of spiritual health (37).
The influence of spiritual well-being in life can serve as a mechanism for coping with anxiety induced by crises. Anxiety related to COVID-19 adversely affects all facets of health, quality of life, and individuals’ outlook on the future, while spiritual well-being can mitigate these adverse effects (36). Studies have indicated that the widespread COVID-19 pandemic, the anticipation of adverse events affecting oneself and one's family, along with the stress and challenges brought about by the pandemic in the country, have negatively impacted adolescents' mental health, elevating their levels of COVID-related anxiety (1). However, a higher sense of spiritual well-being has been associated with reduced levels of COVID-related anxiety among adolescents.
5.1. Limitations
Due to the widespread presence of the disease in Iran and the partial operation of schools during this research, opportunities for face-to-face sampling were limited. Moreover, the comparison samples differed significantly in terms of age and gender, with the group of patients with chronic diseases being significantly younger than the group without chronic diseases. The results of this research are correlational and do not establish causality.
5.2. Conclusions
The findings suggest a significant relationship between spiritual well-being and the level of COVID-related anxiety, showing that spirituality plays a beneficial role in reducing the anxiety provoked by COVID-19. Adolescents with high levels of spiritual well-being during this crisis experienced less COVID-related anxiety. It is thus vital for caregivers and policymakers to focus on enhancing spiritual health and offering planned spiritual care as part of comprehensive services to lessen adolescents' anxiety during this period.