1. Background
Cardiovascular diseases rank as the top cause of death worldwide, affecting an estimated 442.7 million individuals and resulting in approximately 17.9 million deaths annually, which constitutes about 31% of all global mortality (1, 2). Iran exhibits one of the highest age-standardized prevalence rates of cardiovascular diseases, with more than 9,000 cases per 100,000 individuals (3).
Ischemic heart disease (IHD), also known as coronary artery disease and cardiovascular atherosclerotic disease, currently stands as one of the leading causes of death globally (4). In 2019, within the Middle East and North Africa region (including Iran), IHD was the predominant cause of death, accounting for one-quarter of all deaths (799,484.4 deaths). That year, IHD was also recognized as the principal cause of both overall and premature mortality in Iran (5, 6). While a significant reduction in IHD-related mortality has been observed in Western countries due to a focus on primary prevention and advancements in diagnosis and treatment, IHD continues to present new public health challenges in developing nations (7).
Ischemic heart disease (IHD) typically presents clinically as ischemic cardiomyopathy or myocardial infarction. An increasing number of individuals with non-fatal IHD suffer from chronic disabilities and a reduced quality of life (QoL) (6).
Revascularization, or reopening of coronary arteries, is a prevalent treatment for patients with IHD. This approach encompasses 2 primary methods: coronary artery bypass graft (CABG) and percutaneous coronary intervention (PCI) (8). PCI is the most frequently performed procedure for the revascularization of IHD, and significant progress in managing IHD with PCI has been achieved over recent decades (9). The core techniques of PCI include balloon angioplasty and coronary stenting, making it considered less invasive compared to CABG (10). Patients with IHD who undergo PCI often can resume partial normal activities with a low risk of cardiac events (11). However, the probability of requiring repeat angiography and further revascularization is higher in PCI patients than in those who undergo CABG (12).
Numerous studies have underscored the importance of assessing QoL as a crucial outcome measure in the treatment of IHD (13). There is evidence from several studies indicating that treatment for IHD can enhance patients' QoL. For instance, a systematic review and meta-analysis by Kaambwa et al. found that QoL in patients with acute coronary syndrome improves following various treatments, including PCI (14). Nevertheless, research has shown that the QoL for these patients tends to decline over time (15). In a study of Austrian patients with cardiovascular disease who underwent interventions such as PCI, Höfer et al. observed a significant reduction in their QoL two years after completing a cardiac rehabilitation program (16). Similarly, Bahramnezhad et al. reported a decrease in QoL among patients who had undergone balloon angioplasty three months after the procedure (17).
Healthcare professionals, including nurses, are encouraged to implement interventions for post-PCI patients to maintain and improve their QoL (15). Encouraging patients post-PCI to adopt healthy behaviors and self-care practices has been shown to effectively minimize complications and thereby improve their QoL. The information-motivation-behavioral (IMB) model, originally developed by Fisher in 1992 to address AIDS-related risk behaviors, aims to facilitate behavior change by focusing on three essential elements: information, motivation, and behavioral skills (18).
Previous research has shown that interventions based on the Information-Motivation-Behavioral (IMB) model have improved the QoL of patients with type 2 diabetes (19) and enhanced the adherence of patients with chronic obstructive pulmonary disease (COPD) to their inhaler regimens (20). In Iran, 2 studies have demonstrated the efficacy of the IMB model in improving body size in women who have undergone bariatric surgery and in promoting adherence among CABG patients (21, 22). The IMB model suggests that motivation comprises 2 aspects: Belief in the personal benefits of behavioral changes (positive insight) and the perception of social support for engaging in targeted behaviors (social motivation) (23). According to this model, it is crucial to identify and address knowledge, motivation, and behavioral skills gaps in post-PCI patients to enhance their QoL.
The literature review indicates that there has not yet been a study investigating the impact of this model on the QoL of post-PCI patients.
2. Objectives
The present study was undertaken to explore the effectiveness of an educational program based on the IMB model in improving the QoL of patients after PCI.
3. Methods
3.1. Study Design and Participants
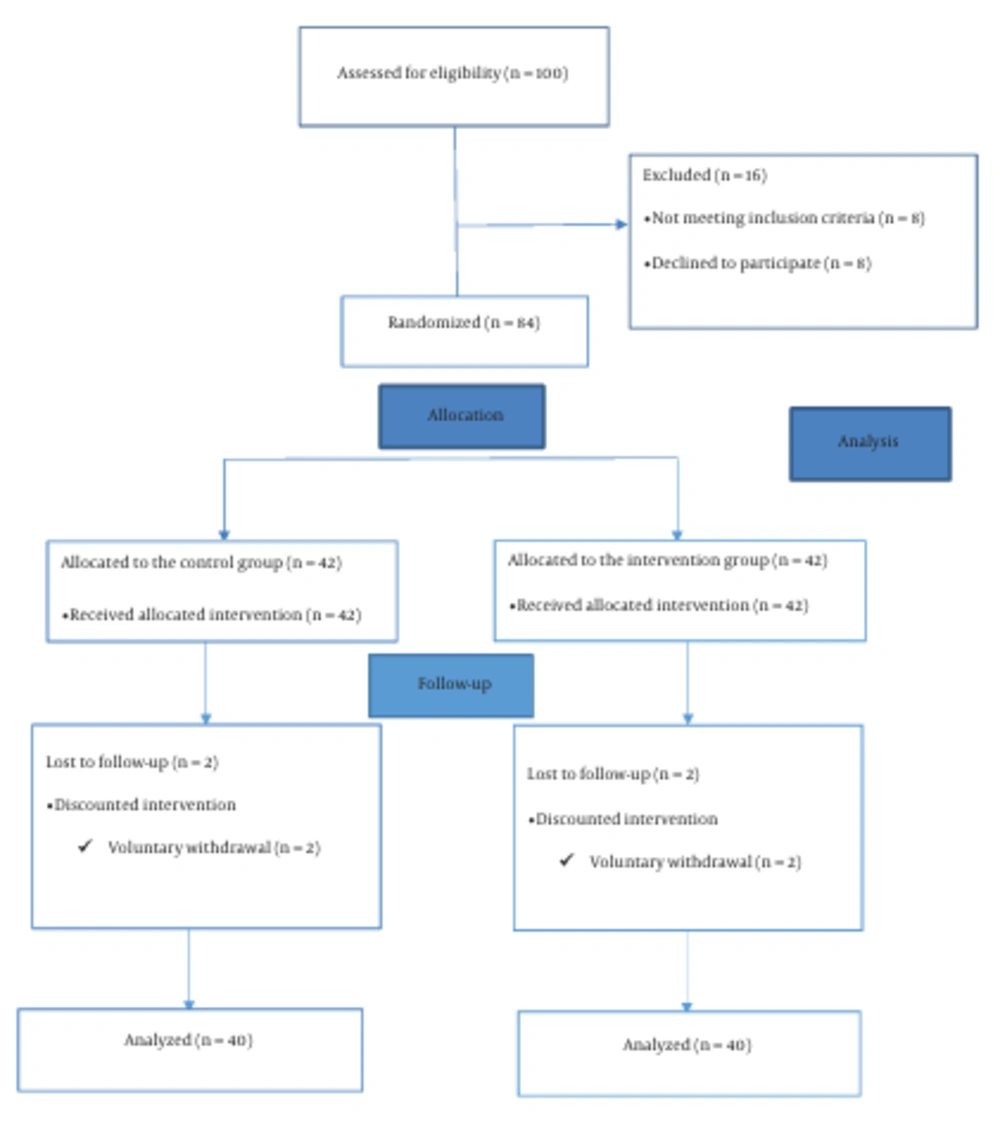
This study is a quasi-experimental study carried out in 2020. Based on previous research (m1 = 29.3, m2 = 55.2, S1 = 34.8, and S2 = 44.0) (24) and considering α = 0.05, β = 0.8, along with a 15% attrition rate, the required sample size was determined to be 42 patients for each study group. A total of 108 patients were screened for eligibility at the Cardiovascular Clinic of Razi Hospital in Birjand city, eastern Khorasan, Iran. The eligibility criteria included being aged 30 – 75 years, having undergone stenting within the last 9 months, possessing normal vision and hearing, not having previously participated in IMB-based interventions, and not suffering from chronic diseases that could impact the quality of life (e.g., chronic kidney disease). The exclusion criteria involved missing more than 2 training sessions or declining to continue with the study. Convenience sampling was employed to select participants who fulfilled the inclusion criteria. Initially, participating patients completed two forms: A demographics form and the Quality-of-Life Short Form questionnaire (SF-12). Subsequently, they were randomly allocated to either the intervention group (n = 42) or the control group (n = 42) through permuted block randomization (block size = 2, allocation ratio = 1:1). The randomization was conducted by a second researcher using sequentially numbered opaque envelopes, each containing a card indicating the group assignment (either intervention or control group). Upon verifying a participant's eligibility, the researcher opened the next sealed envelope in the sequence, and the participant was then allocated to the study group as specified on the card.
In this study, allocation concealment, as well as blinding of researchers and participants, were not feasible. Participants in the intervention group engaged in an IMB-based educational program. Conversely, patients in the control group received the standard care customary at the Cardiology Clinic. Both groups, comprising 40 patients in the intervention and control groups, returned to the Cardiology Clinic 6 weeks following the initial assessment to complete the SF-12 questionnaire (post-test). Subsequently, all participants were asked to complete the QoL survey again one month after the second data collection phase (follow-up) (Figure 1).
3.2. Intervention
The Information-Motivation-Behavioral (IMB) health behavior change model (25) was applied in this study to address the informational, motivational, and behavioral deficits impacting adherence to treatment regimens among post-PCI patients. The selection of intervention topics was informed by an extensive literature review (26-29), long-term interactions between the researchers and the patients, and consultations with field experts. The participants in the intervention group were organized into 2 groups of 10 and 2 groups of 11. The IMB-based educational program was delivered over 6 weekly sessions, each lasting 60 minutes.
During the first session, patients were introduced to the second author, who explained the expectations from the participants and formed 4 intervention groups. The second and third sessions covered a range of topics, including the nature of IHD, its risk factors and complications, a basic overview of PCI, the importance of adhering to the prescribed regimen, the benefits of exercise and physical activity, the necessity of timely and correct medication usage, an introduction to how the prescribed medications function, the importance of quitting smoking, and stress management techniques for patients. These sessions utilized lectures, slides, question-and-answer segments, and group discussions to facilitate learning. At the end of the third session, an opportunity was provided for patients to ask questions or express concerns related to their illness or condition. The focus of the second and third sessions was primarily on the informational aspect of the IMB model.
In session four, the psychiatric nurse established trusting relationships with the patients, enabling them to openly discuss their feelings and concerns, aligning with the motivational aspect of the intervention. During these sessions, she aimed to boost the patients' positive attitudes and set realistic goals to ensure adherence to their treatment regimen and enhance their health behaviors. Techniques such as active listening, providing feedback, and acknowledging the patients' previous efforts to stick to their treatment plans were utilized. The focus of the fourth session was on the motivation component of the IMB model.
The fifth session was dedicated to teaching and practicing practical skills, including blood sugar management, deep breathing and relaxation exercises, and physical activities, centering on the behavioral skills component of the IMB model.
In the sixth and final session, a comprehensive review of the material covered in the previous sessions was conducted, coupled with a question-and-answer period and practical exercises to reinforce the participants' training. Any outstanding questions or uncertainties were also clarified. Additionally, during this session, participants completed the SF-12 questionnaire again. Importantly, all sessions were conducted in the presence of the patients' primary caregivers. Pamphlets summarizing the content of the educational sessions were distributed to the patients. Lastly, participants were encouraged to maintain telephone contact with the second researcher throughout the follow-up period.
3.3. Data Collection Tools
3.3.1 Demographic Information Questionnaire
A demographics questionnaire was utilized to gather data on the participants, including age, gender, marital status, employment type, and level of education.
3.3.2. The Iranian Version of the Short Form Health Survey 12 (SF-12)
This form was employed to assess the QoL of the study participants. It includes 12 items distributed across eight subscales: Physical limitations, physical functioning, bodily pain, general health perception, vitality, social functioning, role limitations due to emotional problems, and mental health. These items are designed to evaluate two overarching constructs: The Physical Component Summary (PCS) and the Mental Component Summary (MCS), with scores ranging from 0 to 100 for each component. A score of 0 indicates the lowest level of health perceived, whereas a score of 100 signifies the highest. Scoring for the SF-12 was conducted according to the U.S. norm-based scoring system (30). Previous research in Iran has confirmed the SF-12 as a valid and reliable instrument for measuring QoL (31). In this study, the Cronbach's alpha coefficients for the PCS and MCS were 0.71 and 0.74, respectively.
3.4. Ethical Considerations
The Ethics Committee at Birjand University of Medical Sciences approved the study's protocol (Ethical code: IR.BUMS.REC.1398.253). After the study's objectives were clearly explained to the eligible patients, they were reminded that their participation was entirely voluntary. Furthermore, they were assured of the confidentiality of their identities and responses. Finally, patients in the control group were informed that the designed intervention would be made available to them should they express interest in it.
3.5. Statistical Analysis
The collected surveys were coded and imported into SPSS version 24 for analysis. The statistical analysis comprised both descriptive statistics, such as mean, standard deviation, and frequency percentage, and inferential tests. Initially, the Kolmogorov-Smirnov test was applied to evaluate the normal distribution of the data. Given that the data were normally distributed, within-group repeated measures ANOVA, the Bonferroni post hoc test, and the independent t-test were employed for the analysis. A significance level of P < 0.05 was established for determining statistical significance.
4. Results
The final analysis focused on the questionnaires completed by 80 patients, with 40 in the experimental group and 40 in the control group. Table 1 presents a comparison of the demographic characteristics of the patients across the 2 study groups.
| Groups and Variables | Intervention | Control | P-Value |
|---|---|---|---|
| Gender | 0.33b | ||
| Male | 26 (65) | 30 (75) | |
| Female | 14(35) | 10 (25) | |
| Age (year) | 0.70b | ||
| < 50 | 10 (25) | 7 (17.5) | |
| 50 - 60 | 17 (42.5) | 18 (45) | |
| 60 - 70 | 13 (32.5) | 15 (37.5) | |
| Marital status | 0.76b | ||
| Single | 6 (15) | 7 (17.5) | |
| Married | 34 (85) | 33 (82.5) | |
| Educational level | 0.89b | ||
| Primary/Secondary | 18 (45) | 20 (50) | |
| High school | 8 (20) | 7 (17.5) | |
| Associate degree | 6 (15) | 4 (10) | |
| Bachelor degree | 8 (20) | 9 (22.5) | |
| Occupation | 0.64b | ||
| Self-employed | 11 (27.5) | 13 (32.5) | |
| Employee | 6 (15) | 3 (7.5) | |
| Homemaker | 11 (27.5) | 9 (22.5) | |
| Retiree | 12 (30) | 15 (37.5) |
a Values are expressed as No. (%).
b Analyzed by the Chi-square test.
The initial mean QoL pretest scores within the physical health domain showed no significant differences between the 2 groups (P = 0.19). A within-group repeated measures ANOVA was conducted to evaluate the mean physical health scores at 3 different times: Pretest, immediately after the intervention (posttest), and one month following the intervention (follow-up). This analysis revealed a significant change over time within the intervention group (P = 0.001), indicating that the physical health scores experienced significant variations across these time points. In contrast, the control group exhibited no significant change (P = 0.66), implying that the physical health scores remained relatively unchanged throughout the study. Patients in the intervention group demonstrated a statistically significant improvement in their average physical health scores at both the post-test and follow-up compared to the pretest, as highlighted by the Bonferroni test (P = 0.001 and P = 0.004, respectively). However, no significant difference was observed between the follow-up and post-test mean scores (P > 0.05; Table 2).
Before the intervention, the mean QoL scores for the psychological health dimension showed no significant difference between the 2 groups (P = 0.3). A within-group repeated measures ANOVA revealed that the mean psychological health score in the intervention group demonstrated a significant change (P < 0.001) across the three stages: before, immediately after, and one month after the intervention. However, in the control group, no significant difference was observed (P = 0.61; Table 2). The Bonferroni test indicated a significant increase in the mean psychological health score in the intervention group immediately after the intervention compared to before (P < 0.001). Furthermore, one month after the intervention, there was a significant improvement in the mean psychological health score compared to immediately after (P = 0.02). Nonetheless, no significant difference was found immediately after the intervention compared to before (P > 0.05; Table 2).
| Groups Variables and Phases | Intervention Group | Control Group | P-value (Between Group) a |
|---|---|---|---|
| Physical health | |||
| Pretest | 40.10 ± 10.32 | 43.09 ± 9.88 | 0.19 |
| Posttest | 42.93 ± 9.15 | 43.38 ± 10.26 | 0.84 |
| Follow-up | 43.51 ± 8.94 | 43.79±9.81 | 0.89 |
| Repeated measurement b | |||
| Time effect | 0.001 | 0.66 | |
| Group effect | 0.55 | ||
| Psychological health | |||
| Pretest | 41.75 ± 7.02 | 40.10 ± 7.37 | 0.31 |
| Posttest | 43.53 ± 7.50 | 39.38 ± 7.04 | 0.01 |
| Follow-up | 45.63 ± 6.37 | 40.05 ± 9.81 | <0.001 |
| Repeated measurement c | |||
| Time Effect | <0.001 | 0.61 | |
| Group Effect | 0.01 |
aIndependent t-test.
bSphericity Assumed.
c Greenhouse-Geisser.
In the intervention group, the mean changes in the physical health score immediately after the intervention, as well as one month after the intervention, compared to before the intervention, were significantly greater than those observed in the control group (P = 0.03). There was no statistically significant difference between the patient groups in terms of mean changes 1 month after the intervention compared to immediately after the intervention (P = 0.87; Table 3).
The mean changes in the psychological health scores were significantly greater in the intervention group compared to the control group, both in the posttest (P = 0.03) and follow-up phases (P = 0.002) when compared to the pretest scores. However, no statistically significant difference was observed between the mean changes from the posttest to the follow-up between the 2 patient groups (P = 0.12; Table 3).
| Group and Variables | Intervention | Control | P-Value a |
|---|---|---|---|
| Mean Difference ± SD | Mean Difference ± SD | ||
| Physical health scores | |||
| Pretest-Posttest | 2.83 ± 4.37 | 0.29 ± 6.21 | 0.03 |
| Pretest-Follow-up | 3.41 ± 6.23 | 0.7 ± 5.08 | 0.03 |
| Posttest- Follow-up | 0.58 ± 5.59 | 0.41 ± 3.2 | 0.87 |
| Psychological health | |||
| Pretest-Posttest | 1.77 ± 4.56 | -0.72 ± 5.75 | 0.03 |
| Pretest-Follow-up | 3.87 ± 4.92 | -0.05 ± 5.99 | 0.002 |
| Posttest- Follow-up | 2.09 ± 4.87 | 0.67 ± 3.14 | 0.12 |
aIndependent t-test.
5. Discussion
This study aimed to evaluate the impact of an educational program based on the Information-Motivation-Behavioral (IMB) model on the QoL of patients after PCI. Initially, no significant differences were found in the mean QoL scores for the physical health domain between the study groups. However, significant increases in mean scores were observed in the intervention group at both the post-test and follow-up phases, unlike in the control group, where the increases were not statistically significant. Furthermore, the intervention group experienced significantly greater changes in the mean physical health score immediately after the intervention and one month later compared to the control group. This model, when applied to study the QoL of individuals with diabetes by Yao et al. found that the mean QoL score in the physical health domain increased significantly in revealed significant improvements in the physical health domain of the intervention group both immediately and one-month post-intervention (19). The implementation of the training program based on the IMB model provides essential knowledge about disease pathophysiology, contributing factors, diagnostic and treatment methods, nutrition, physical activity, medication usage, adherence to treatment, and stress management through effective communication, reinforcing care interactions, and offering feedback to patients (24). This care program shows promise in improving patient QoL (23, 25) by enhancing motivation and encouraging health-promoting behaviors. In a similar study, Yilmazer et al. investigated the effect of this care model on the QoL of ostomy patients, concluding that the application of this model significantly raised the mean QoL score in the intervention group (26).
The study demonstrated that the mean QoL scores for the psychological health dimension showed no significant difference between the groups at the pretest. However, this average significantly increased both immediately and one month after the intervention in the intervention group, in contrast to the control group, where the increase was not statistically significant. Furthermore, the changes in psychological health scores before and immediately after the intervention, as well as before and one month after the intervention, were significantly more pronounced in the intervention group compared to the control group. Li et al. explored the impact of a care management program on cardiac patients post-PCI, noting that patients often experience stress and anxiety after procedures like stent implantation or coronary balloon placement. This stress can be attributed to physical conditions, impaired physical function, and concerns over potential adverse effects of the procedures. Such uncertainty is a primary factor for their negative emotions and anxiety levels (32). In Li et al.’s study, anxiety and depression scores were significantly lower in the intervention group than in the control group after the care intervention. It is suggested that employing various care models focused on enhancing QoL, promoting treatment adherence, encouraging self-care, and improving care management can positively affect patients' psychological well-being and physical performance (32).
In this study, a family member of the patient was present during the training sessions. Kim et al. identified a positive and significant association between QoL, social support, marital status, and the presence of a primary caregiver in patients with IHD undergoing PCI (33). The involvement of a primary caregiver in this study can be considered a contributing factor to the success of the implemented intervention.
The results of this research showed that the mean scores related to QoL in both physical and psychological health domains experienced a slight increase one month after the intervention compared to immediately after the intervention. However, this increase was not statistically significant. Furthermore, there was no statistically significant difference in the average change in physical and psychological health scores between the 2 groups at the follow-up compared to the post-test phase. In various studies, the model used has shown significant improvements in the QoL of individuals with cardiovascular and diabetic conditions, with these improvements being noticeable immediately after the intervention and at later time points, including one month, three months, and six months post-intervention (19, 34, 35). Given these observations, it is plausible to suggest that the effectiveness of this particular model on different dimensions of QoL may depend on the unique characteristics of the individual's disease. The differences in the types of issues and concerns faced by patients undergoing PCI compared to those experienced by other groups, such as diabetes patients, might explain the observed limited long-term efficacy of the intervention based on the Information-Motivation-Behavioral (IMB) model in this study. In future research, there is a possibility to investigate the effects of periodically reinforcing educational interventions during the follow-up period. The main aim would be to determine how such interventions might enhance the long-term sustainability of the intervention's effects, as per the IMB model, particularly in patients who have undergone PCI.
To the best of our knowledge, this study is the inaugural investigation into the impact of an educational program based on the Information-Motivation-Behavioral (IMB) model on the QoL of patients undergoing PCI. It lays the groundwork for future research designed within the IMB model framework to enhance the QoL of PCI patients. Moreover, considering the scarcity of studies utilizing this model among post-PCI patients to date, upcoming research could aim to thoroughly explore the mechanisms underlying the effectiveness of this model.
A limitation of the current study is its recruitment of participants exclusively from a single cardiovascular center, which may affect the generalizability of the findings. Future research could benefit from being conducted across multiple sites to potentially broaden the applicability of the results. Additionally, this study employed a quasi-experimental design; future studies incorporating full allocation concealment and some form of blinding could help to minimize potential biases.
5.1. Conclusions
The quality of life (QoL) of patients following PCI may be improved through their participation in the Information-Motivation-Behavioral (IMB)-based educational program designed in this study. This research can act as a foundation for developing interventions that have more enduring impacts on patient outcomes.