1. Background
Hearing impairment is one of the most important causes of childhood behavioral disorders among the various types of disabilities (1). Bilateral dominant hearing loss affects 1 out of every 750 children (2). Hearing impairment can occur in conjunction with other symptoms and as part of a disease, which is referred to as syndromic hearing loss, or it can occur as a single symptom, which is referred to as non-syndromic hearing loss (3, 4). Given that children form their most fundamental and vital bonds with their families, the failure of families to understand the responsibility and solve children’s social problems can result in negative traits and aggressive behaviors in children. One of the manifestations of disruptive behavior disorders (DBDs) is aggression. Similar to any other behavior, aggression is a multifaceted and complex phenomenon (5).
Different environmental stimuli are combined with various mental and psychological processes, resulting in distinct forms of aggression (6, 7). There is ample evidence that aggression is a major risk factor for delinquency and behavioral disorders (8, 9). As a result, it is critical to identify this component and its precursors accurately. Despite the relatively high prevalence of aggression and its clinical importance, few attempts have been made to classify aggressive behavior systematically and orderly, consistent with clinical objectives. This can be attributed to the psychological and social complexity of aggressive behavior, a lack of consistency in its etiology, or the diversity of aggressive groups (10). Therefore, it is necessary to examine and control the health problems of aggressive children through the implementation of a cohesive plan to help their families adapt and care for their disabled children and improve their health status.
The functional division of aggression is a type of classification used in recent decades to describe aggression. It explains how a person’s internal motivation for aggressive behavior works. There are two types of aggressive behavior based on the function and motivation of the person: reactive and proactive (11). The emotional response to a perceived threat is known as reactive aggression; however, proactive aggression is more common in externalizing disorders, such as antisocial behavior and heavy drug and alcohol abuse (12). Studies have shown that reactive aggression is associated with negative emotions and internalizing disorders in childhood and adolescence (13, 14).
Moreover, previous physical abuse, the early onset of attention problems and impulsivity, being a victim of bullying, suicidal thoughts, incompatibility with peers, poor emotional and behavioral regulation, inconsistent parenting, excessive caution against threat cues, and unpredictable environments all contribute to the development of reactive aggression (15). Aggressive functions are a subset of aggressive behavior that are classified according to their purpose (16). Studies indicate that the structure of these purposes varies depending on how social cues are interpreted (17). As a result, in ambiguous social situations, adolescents with reactive aggression attribute more hostile intent to others. However, proactive aggression occurs when aggression is used to achieve a predetermined goal (11).
According to the schema theory of family relations, beliefs and expectations are formed in children due to family experiences in a stressful environment (18). Cong et al. (19) also assessed the family and its role in the “McMaster” family functioning system model. This model describes the family’s structure, organization, and exchange pattern and tests family relationships on a scale ranging from healthy to severely mentally ill. McMaster’s model is based on the following basic hypotheses of system theory: (1) Family members are inextricably linked; (2) no family member can be studied separately in the absence of others; (3) family structure and organization are essential determinants of the family member’s behavior; and (4) the family interactive pattern strongly influences the behavior of each family member.
This model assesses and measures five aspects of family life: Problem-solving, roles, emotional accountability, emotional companionship, and behavior control. As a result, it is critical to investigate the factors influencing children’s aggression on the part of families, particularly mothers, because mothers spend more time with their children than fathers do, and most of the children’s behavioral consequences are formed by their interactions with mothers (20).
Parents’ attitudes toward having a disabled child can cause aggressive behavior in children. When parents see a disability in their child after nine months of waiting, they will face a score of despair, failure, and depression. The heavy look of pity from relatives, friends, and acquaintances is another factor that negatively affects parents of such children (21). Families with deaf and hard-of-hearing children frequently face serious mental and emotional tensions. Children with hearing impairment put a great burden on parents because this impairment causes serious mental distress and stress for parents (10). A high level of stress in parents of deaf and hard-of-hearing children is associated with aggression and behavioral problems in children (20).
Chronic fatigue has depressive mood symptoms, such as sleep disorders, attention deficits, cognitive deficits, and debilitating fatigue, which can sometimes be contradictory (22). Researchers define fatigue as a feeling of weakness and reduced capacity to perform mental and physical activities (23). The global prevalence of this syndrome ranges from 0.2% to 2.8% (24). Having a deaf or hard-of-hearing child can be stressful for mothers and cause many complications for them, such as chronic fatigue syndrome. Individuals with chronic fatigue patients experience severe disability and discomfort as a result of these symptoms (25). Due to the multidimensional nature of fatigue, particularly in psychological and mental dimensions, the relationship between chronic fatigue and cognitive processes has attracted great attention in recent years (26). For example, Fisher et al. (27) reported that chronic fatigue was more common in parents of disabled children than those of normal children.
In general, investigations into parents’ attitudes toward children with special needs are of special importance and applied value for developing appropriate educational and rehabilitation programs. Having a child with special needs often causes irreparable harm to the family. Some families are so vulnerable to such harm that the mental health of their members suffers severely.
2. Objectives
Accordingly, the present study aimed to investigate the mediating role of maternal chronic fatigue in the relationship between the reactive aggression of deaf and hard-of-hearing children and attitudes toward having a disabled child.
3. Methods
3.1. Design
This correlational-descriptive study used structural equation modeling (SEM) to examine the relationship between variables.
3.2. Population and Sampling
The study population consisted of mothers of all deaf and hard-of-hearing elementary students in special centers for such children in Ahvaz, Iran, in the academic year 2022 - 2023, of whom 202 mothers were selected as the sample through convenience sampling. To this end, a list of educational centers for the deaf and hard of hearing affiliated with the Khuzestan Department of Exceptional Education was provided, and then 215 subjects who met inclusion and exclusion criteria were selected as participants. Based on Wolf et al. (28), the sample size was estimated to be 195 based on the research variables. In this study, the sample size was calculated by considering the drop rate of 10%. In this study, after removing 13 incomplete questionnaires, the data of 202 participants were analyzed.
3.3. Inclusion and Exclusion Criteria
The inclusion criteria were elementary students aged 7 - 12 years, non-affliction of children with diagnosed developmental disorders, and non-affliction of mothers with diagnosed psychological disorders. In addition, the exclusion criteria were distorted questionnaires and unwillingness to continue the study.
3.4. Instruments
3.4.1. Reactive-Proactive Aggression Questionnaire
Developed by Dodge and Coie (29), this questionnaire consists of 19 items in two subscales: Reactive aggression and proactive aggression. In this study, the reactive aggression subscale (7 items) was completed by mothers. The items of this subscale are scored based on a 5-point Likert scale (from 1: Very low deficiency to 5: Very high deficiency). Rezaei and Dehghani (30) reported a Cronbach’s alpha coefficient of 0.81 for the Reactive-Proactive Aggression Scale.
3.4.2. Attitudes of Parents with Special Needs Children Toward Their Children Scale
Developed by Govender (31), this scale consists of 33 items in 5 subscales: acceptance and affection (8 items), shame (3 items), failure (3 items), disappointment (3 items), and extreme support (7 items). The items are scored based on a 5-point Likert scale (from 5: Totally agree to 1: Totally disagree), and higher scores indicate more positive attitudes. Asghari-Nekah and Bolghan-Abadi (32) reported a Cronbach’s alpha coefficient of 0.80 for the attitudes of parents with special needs children toward their children scale (APSNCS).
3.4.3. Chalder Fatigue Scale
This 14-item self-report scale was developed by Chalder et al. (33) to measure the mental and physical signs of fatigue. The items are scored based on a 4-point Likert scale (from 0: Not at all to 3: More than usual). This scale consists of two subscales: physical fatigue (with a mean score of 1 to 8) and mental fatigue (with a mean score of 9 to 14). The cut-off score for this scale is 14. Sakkaki et al. (34) reported a Cronbach’s alpha coefficient of 0.87 for the Chalder Fatigue Scale.
3.5. Ethical Considerations
Informed consent was obtained from the participants in this study. Moreover, ethics approval for this study was obtained from the Ethics Committee of Islamic Azad University, Ahvaz Branch (code: IR.IAU.AHVAZ.REC.1402.026).
3.6. Statistical Analysis
The relationship between the research variables was examined by the Pearson correlation coefficient. Skewness and kurtosis were used to evaluate the normality of the data. In addition, the research model was tested using SEM in SPSS software (version 27) and AMOS software (version 24).
4. Results
Demographic data showed that 102 participants had a female child, and 100 participants had a male child. Regarding educational attainment, 127, 20, 37, and 18 participants had a high school diploma, an associate degree, a bachelor’s degree, and a master’s degree, respectively. In addition, 45 participants were employed, and 157 participants were housewives. Table 1 shows the descriptive statistics of the research variables (i.e., mean, standard deviation, skewness, kurtosis, and Pearson correlation coefficient).
Descriptive Data and Correlation Coefficients of the Research Variables
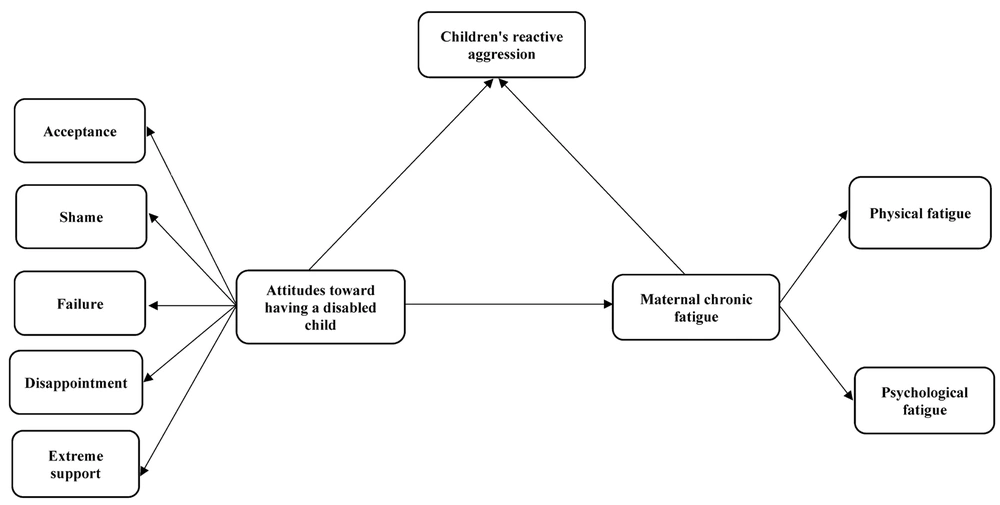
The Pearson correlation coefficient showed a significant correlation between all research variables. Figure 1 depicts the initial proposed model to explain the reactive aggression of deaf and hard-of-hearing children based on attitudes toward having a disabled child and maternal chronic fatigue.
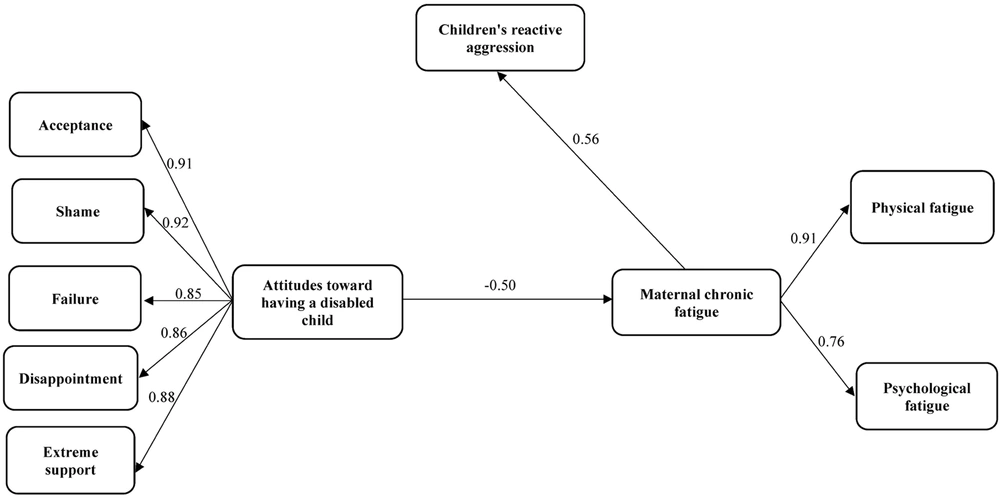
As shown in Table 2, the root mean square error of approximation (RMSEA) for the initial model was equal to 0.087, indicating that the mode needed to be modified. In order to modify the initial model, the path from attitudes toward having a disabled child to aggression was removed. The finalized model, which was well fitted to the data, is shown in Figure 2.
| Fit Indicators | χ2 | df | (χ2/df) | TLI | CFI | RFI | NFI | RMSEA |
|---|---|---|---|---|---|---|---|---|
| Initial model | 39.95 | 18 | 2.22 | 0.97 | 0.98 | 0.95 | 0.97 | 0.087 |
| Final model | 40.43 | 19 | 2.13 | 0.97 | 0.98 | 0.95 | 0.98 | 0.075 |
Fit Indices of the Tested Research Model
Table 3 reports the estimated path coefficients for the examination of direct paths. The results revealed significant relationships between attitudes toward having a disabled child and maternal chronic fatigue (β = - 0.50, P < 0.001) and between maternal chronic fatigue and reactive aggression of deaf and hard-of-hearing children (β = 0.56, P < 0.001). There was no significant relationship between attitudes toward having a disabled child and reactive aggression of deaf and hard-of-hearing children (β = 0.05, P = 0.488). Table 3 shows that maternal chronic fatigue mediates the indirect and significant relationship between attitudes toward having a disabled child and children’s aggressive behavior (β = - 0.35, P = 0.010).
| Path | Path Type | β | P |
|---|---|---|---|
| Attitudes toward having a disabled child → Reactive aggression of deaf and hard-of-hearing children | Direct | 0.05 | 0.488 |
| Attitudes toward having a disabled child → Maternal chronic fatigue | Direct | - 0.50 | 0.001 |
| Maternal chronic fatigue → Reactive aggression of deaf and hard-of-hearing children | Direct | 0.56 | 0.001 |
| Attitudes toward having a disabled child → Reactive aggression of deaf and hard-of-hearing children through maternal chronic fatigue | Indirect | -0.35 | 0.010 |
Direct and Indirect Paths in the Final Model
5. Discussion
The present study aimed to investigate the mediating role of maternal chronic fatigue in the relationship between the reactive aggression of deaf and hard-of-hearing children and attitudes toward having a disabled child. The first study finding revealed a significant relationship between attitudes toward having a disabled child and children’s aggressive behavior. Since no similar study consistent with this hypothesis was found in the literature, this study is the first one that deals with these variables. The Pearson correlation coefficient showed a significant relationship between attitudes towards having a disabled child and aggressive behavior of children, which was mediated by maternal chronic fatigue. To explain this finding, it can be stated that having a disabled child causes a great deal of stress and pressure on parents. Among the stressful factors affecting parents of such children are financial hardships and pressures, such as medical expenses, emotional problems in the family, such as excessive care for the disabled child, rejection of other children, and devoting little time to other family members. As emotional support for cognitive-psychological development during childhood, the mother plays an effective role in their children’s health or behavioral disorders; therefore, the mother’s psychological health plays a major role in the child’s overall development (35). As parents, they might suffer from mental illness, feelings of worthlessness and guilt, impaired physical function, and fatigue. The presence of a disabled child limits the family’s social relationships, recreational activities, and social communication. The lower the level of social relations in this group of families, the greater the parents’ psychological helplessness (7).
The study results showed a significant and positive relationship between maternal chronic fatigue and reactive aggression in deaf and hard-of-hearing children. This is consistent with the findings of Fisher et al. (27), who reported that chronic fatigue was more common in parents of disabled children than those of normal children. To explain this finding, it can be stated that increasing psychological pressures are imposed on parents, particularly mothers when their child is diagnosed with hearing problems, which can result in reactions such as psychological trauma, disappointment, anger, and depression. In this regard, with the emergence of parents' natural defensive reactions, particularly in mothers, aggressive behaviors are observed in children more frequently. Such an event is very shocking, unexpected, exhausting, and psychologically harmful for parents. As one of the reactions that mothers with deaf children exhibit, fatigue is associated with high levels of negative affect, such as anger, depression, and anxiety. Fatigue is one of the long-term and continuous emotional states related to low levels of meaning in life, self-expression, self-fulfillment, and self-expression. In general, children's hearing problems cause the negative cycle of parent-child interaction to remain uncorrected, increasing the mental burden and fatigue on mothers (26).
The results showed that maternal chronic fatigue mediated the significant relationship between attitudes toward having a disabled child and aggressive behavior of deaf or hard-of-hearing children. Regarding this finding, no similar study was found in the literature to be compared to this study. The direct relationship between attitudes toward having a disabled child and aggressive behavior of deaf or hard-of-hearing children was not statistically significant. On the other hand, the results showed that attitudes toward having a disabled child increase maternal chronic fatigue, cause reactive aggression in children, and decrease positive mother-child interactions. A disabled child causes the development of many physical diseases, such as pain, and mental disorders, such as depression and anxiety, in addition to the mental stress it imposes on the family. Therefore, it can be concluded that maternal chronic fatigue acts as a moderator in the relationship between attitudes toward having a disabled child and reactive aggression in deaf and hard-of-hearing children.
5.1. Limitations
Since this study was conducted on mothers of deaf or hard-of-hearing elementary students in Khuzestan province, Iran, the findings should be cautiously generalized to similar populations in other cities and regions. Another limitation of this study was using a self-report tool, which might have influenced the report’s validity due to the participants’ social desirability bias. Given that fathers are at present more involved in their children’s daily lives than in the past, high levels of paternal stress and tension can lead to aggressive behaviors in children and social and family problems. Therefore, future studies are recommended to perform similar investigations on the fathers of such children.
5.2. Conclusions
The study findings suggested that the finalized and modified model was well fitted to the data; therefore, it can be used as an effective tool for identifying the factors reducing aggressive behaviors in deaf or hard-of-hearing children. The model proposed in this study is a new scientific discovery that has the potential to reduce reactive aggression in deaf or hard-of-hearing children. Considering the significant relationship between research constructs, specialized clinics can employ this model to develop effective solutions to reduce problems caused by poor family relationships and help parents choose more logical strategies for dealing with these problems.